Factors that affect the outcomes of root canal treatment and retreatment—A reframing of the principles
Abstract
This paper undertakes a broad and comprehensive synthesis of relevant clinical, biological, biomechanical, technical and healthcare services data to understand the factors affecting outcomes of periapical healing after root canal (re)treatment. The medical and dental evidence-based era (1980–present) is contextualized with the earlier evidence drive in endodontics (1911–1940) triggered by the focal infection era. The current evidence-based approach has a sharper focus on evidence quality and derivation of practice guidelines. Contrary views question whether guideline-driven, or expertise-development-driven endeavours would best serve outcome improvement in society. The endodontic discipline functions in a broad healthcare framework and sustains industrial, economic and trend pressures that may be deemed to influence outcomes. The nature of root canal treatment and the challenges in determining the factors that affect its outcomes is discussed. The factors potentially affecting periapical healing after root canal treatment are classified into pre-operative, intra-operative and postoperative groups. These categories subsume multiple elements with interactive influences, creating a complex picture, further confounded by some apparently surprising, counter-intuitive and contradictory findings. The technical versus biological conundrum in root canal treatment continues to cause cognitive dissonance. However, due reflection and cross-discipline-synthesis resolve the apparent data conflicts into a very simple, consistent and plausible picture of how root canal treatment works and the key factors that affect periapical healing. Root canal retreatment is considered mainly in the context of its differences from primary treatment as the majority of factors influencing outcomes are common to both. The exceptional difference is that retreatments have a proportionately reduced probability of healing by virtue of compromised apical root canal ramification access or modified host/infection interactions. Root canal (re)treatment outcomes are dominantly influenced by the nature of prior dynamic host/infection interaction (pre-operative patient factors) and how the direction of this dynamic is influenced by two factors: (1) the active efficacy of the operators' root canal treatment protocol to sustain a microbial ecological shift (intra-operative treatment factors) and dampen periapical inflammation; and (2) the passive ability of the functional tooth (and its restoration margin) to maintain its integrity to resist infection reversal (postoperative restorative factors).
INTRODUCTION
History of the evidence-based era and endodontic outcomes
The medical and dental professions have been obsessed with the “levels of evidence” underpinning their clinical practices for the last 40 years, as witnessed by the logarithmic rise in the breadth and depth of such publications. The focus on evidence of outcomes for root canal treatments, however, began much earlier in the 1900s because of the damaging effects of the “focal infection” challenge (Hunter, 1911) on dental curricula. Leading opponents of the focal infection theory challenged the validity of its evidence on the grounds of poor study design, lack of controls and confounding factors. Johnson (1926) encouraged dentists to take a more rational approach to decisions about their patient management and advocated retention of pulpless teeth when amenable to successful treatment. Fortunately, skillful endodontists promoted quality root canal treatment, adopting aseptic principles and diagnostic radiography, as well as using bacteriological, histological and clinical methods to assess and report treatment outcomes, albeit without the sophistication of modern experimental design and statistical analysis (Appleton & Grossman, 1932; Auerbach, 1938; Blayney, 1922; Buchbinder, 1936; Callahan, 1914; Coolidge, 1927; Crane, 1926; Grove, 1926; Hinman, 1921; Johnston, 1923; Prinz, 1917; Puterbaugh, 1926; Rhein, 1926). The use of rubber dam, good canal access, asepsis, microbial control, chemical agents to dissolve organic tissue, chloro-percha to better fill root canal systems and emphasis on the coronal seal were advocated early on (Crane, 1921; Rhein, 1912). These highly skilled, visionary clinicians, practicing the principles still followed today, became the custodians of the art of Endodontics and helped to swing the pendulum back to tooth conservation, so that by the 1950s, endodontic treatment was accepted by the medical profession and the endodontic specialty was given approval in the USA.
New cost-economic pressures posed a threat to the survival of the endodontic discipline again from the 1990s, this time through treatment planning decisions centering on the question of whether to “save the tooth” or “extract and replace” it with an apparently more predictable implant-supported crown (Torabinejad & Goodacre, 2006). The science of evidence-based practice belatedly averted ongoing irrational options-appraisals leaning towards extraction of savable teeth (Doyle et al., 2006; Gulabivala & Ng, 2019b; Iqbal & Kim, 2006; Kim & Solomon, 2011; Pennington et al., 2009). Once again, the pendulum has swung firmly back in favour of maintaining restorable teeth through predictable endodontic management (Sadowsky, 2021).
Key drivers of endodontic service delivery and their relevance to treatment outcomes
Progress and development in endodontics and endodontology, in common with other medical or dental disciplines, has been driven by the coalescence of numerous independent driving forces in society. The key driver for any healthcare profession is the societal imperative to improve the health of the population as cost-effectively as possible, without imposing an economic burden. These aims are coupled with the desire for both efficacy and efficiency in treatment delivery. Support industries grow up around these global aims to service the delivery needs of health professionals by developing tools and materials suitable for the purpose, at the price of manufacture and profit for the business. Given that healthcare professionals may deliver their remits within different funding frameworks, they too may become embroiled in the business element. There has therefore evolved a complex dynamic between endodontic healthcare, business, and service delivery (Gulabivala, 2018). That publicly funded healthcare bodies and private business willingly invest in root canal treatment is tacit indication by the system that the procedure works and serves a useful purpose.
All components of this complex delivery system must have a vested interest in improving their respective contributions to enhance their measures of success, therefore requiring close interaction amongst them through partnerships in research and development and propagation of protocols, devices, and materials. The proposed model assumes that the key measures of efficacy and efficient service delivery are product-based, although that may not entirely hold true for root canal treatment because of the biological nature of the problem it seeks to resolve (Gulabivala et al., 2019; Ng et al., 2011a, 2011b; Ng, Mann, & Gulabivala, 2011; Ng, Mann, Rahbaran, et al., 2008). Added to this are the facts that root canal system complexity and clinician expertise may be confounding factors (Chambers et al., 2009; Yee, 2019). Nevertheless, endodontics has become a gadget-oriented discipline, with dentists keen to adopt new technology in the interests of efficiency, efficacy and economy.
Nature of expected and available evidence and its value to service delivery
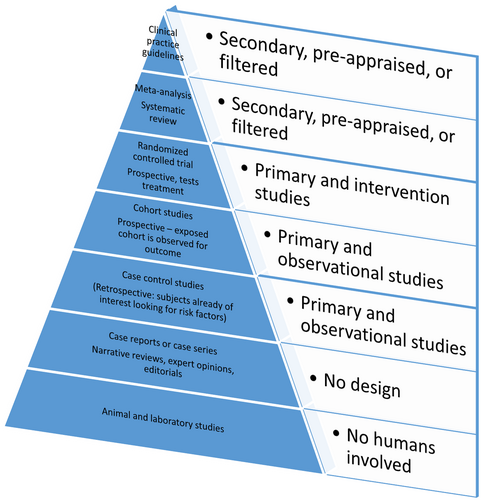
Confidence and assurance in the validity and predictability of root canal treatment is desirable because there remain elements within society that doubt the evidence (Meinig, 1996). Received wisdom suggests that high-quality evidence is typically obtained from pooled outcome data from suitable studies ideally all following consensus guidelines, with a large and representative enough patient and dentist population. The anticipation is that such pooled data, when homogenous may distil and rank key biological, technical and clinical factors that exert a dominant influence on outcomes. Available study types rarely meet these expectations and have been ranked into a hierarchy (Figure 1) based on their methodological quality, design, validity, and applicability to patient care. The highest evidence level is deemed to be derived from a synthesis of quality primary data (randomized controlled trials), by a select group of workers, using a systematic and accepted process that identifies appropriate material, screens for matching entry criteria, filters for quality, extracts useable raw data, pools it, and calculates an estimated overall outcome. Based on such pooled data, guidelines may be agreed by consensus workshops to inform and recommend best practice (Sanz Herrera et al., 2020; Scholmerich, 2000). The intention is to propagate a standardization of approach to raise overall levels of performance by the dentist population working for the overall patient population. With the methodological advances in evidence evaluation, tools and checklists have been developed to guide assessment of risk of bias: RoB2 (https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials); ROBINS-1 (https://methods.cochrane.org/methods-cochrane/robins-i-tool); Newcastle Ottawa Scale for observational studies (http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp), and to designate through grading, the certainty of evidence into the categories of ‘very low’, ‘low’, ‘moderate’ or ‘high’, when making recommendations in clinical guidelines (https://gdt.gradepro.org/app/handbook/handbook.html). The merits of such standardized approaches are self-evident, but they also carry the risk of falling into the trap of ticking boxes without exercising due diligence and intuitive analysis, and thinking out of the box. The approach must not be allowed to stifle productive and innovative synthesis, to facilitate domain knowledge development (Greenhalgh et al., 2018). A proliferating mass of systematic reviews informs on the sufficiency or otherwise of the available evidence, often reaching the conclusion that the evidence quality is inadequate for reliably confident conclusions about best practice or generalizability to the population at large. The majority of the published outcome data may be deemed of moderate or low quality and is thus less amenable to mathematically robust summation. The outcome for the clinician then is no useful guidance, unless they undertake a deep and personal intuitive synthesis that may add to their own domain knowledge, albeit without external consensus. The evidence base for non-surgical root canal treatment is more comprehensive than that for other endodontic procedures. Although the quality and scope of the research does not always reach the highest prescribed hierarchical levels, it does nevertheless provide a breadth and depth of insight for the individual who is open to full and deep exploration of the literature.
In addition to predictability and consistency in treatment delivery, patients also value prognostic accuracy (predicting, projecting, prophesising or foretelling) to aid decision-making in selection of treatment choices. Prognostication skill is an art predicated on mentally weighing the relative balance of different factors affecting treatment outcomes. Such insight is a part of the “expert domain knowledge”, a conglomerate derived through active experience in the application of biological principles coupled with composite outcome data to surmount a spectrum of treatment challenges. Such skill is not gifted by guidelines but is individually developed. The overall tooth prognosis extends beyond endodontics (periodontic, restorative and occlusal aspects), where each element subsumes further subsidiary factors influencing overall prognosis, therefore the clinician must go beyond endodontic guidelines and reach for a broader insight for predictable management.
Population-based summary outcome data may help clinicians to inform patients about the general outcome trend to be expected for their problem but only the dentist's personal audit caseload, case-mix and outcome data are likely to persuade the patient of the suitability of the dentist's skill and knowledge for their care. Such personal data serves the dual purpose of motivating and directing practitioners to refine their technique and knowledge to enhance predictability of their own outcomes (Chambers, 2001).
The flaw in the evidence-based system is that dentists following guidelines blindly, will not work, because the process does not place emphasis on the progressive improvement and development of the individual dentist in understanding the clinical problem and solving it from first principles (Chambers, 2001). Improvement in the outcomes of individual dentists, the ultimate goal, requires integrated correction and development in numerous domains (cognitive, technical, clinical) through dedicated, diligent practice by the dentist, in which the guidelines form only a small directional role (Chambers, 2001; Scholmerich, 2000). Paradoxically, the best study outcomes in the literature can be attributed to a larger proportion of “best individual performances” amongst the studied dentist cohorts, yet in the hierarchy of evidence, the opinion of such high performers (experts) is relegated to the bottom of the pyramid. Exploration of the relationship between evidence-based outcomes and high expert performance at an individual level, merits much deeper consideration (Ericsson, 2009; Ericsson et al., 2018). The distribution of high expert performers across the century of outcome data is not skewed towards the “era of evidence-based practice (1980–present)”, suggesting that the “evidence-base” per se, is not a prior requirement for expertise development. Such an idea may also help to distinguish between domain knowledge (that which makes an expert) and evidence-based knowledge (that which helps to refine the conceptual basis for understanding the problem and how to manage it, or domain knowledge). The evidence-base may contribute to domain knowledge but is not an essential requirement to derive an intuitive conceptual understanding of the biology and biomechanics of the problem, it is the latter that forms a platform for expertise development (Ericsson, 2009; Ericsson et al., 2018) and predictability of outcomes.
Purpose and nature of root canal treatment and its outcome challenges
Root canal treatment is a procedure used to either prevent apical periodontitis or once established, to treat and resolve it. These two ends of the biologic disease spectrum also define the two ends of the outcome spectrum, since the highest success rates are attributed to periapical disease prevention and the lowest to disease resolution, particularly when the measures of disease are at their worst (large, suppurative, symptomatic lesion). Prevention of apical periodontitis broadly encompasses prevention of primary dental diseases as it is their sequel (caries, tooth surface loss, periodontal disease and traumatic injuries). More parochially, it is prevention of spread of pulpitis to apical periodontitis through pre-emptive vital pulp therapy, or partial/total pulpectomy. The absence of apical periodontitis implies the absence of apical bacterial colonization, probably coupled with vital, healthy pulp tissue apically. The prime requirement for management of such a condition is asepsis during the technical execution of instrumentation, irrigation and obturation. The expected probability of retaining periapical health is 90%–99% if asepsis is treated as sacrosanct, regardless of the choice of clinical protocol (Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008), tools or hands of the clinician. That is, the success rates can be predictably and consistently high in the hands of a diverse group of dentists using different protocols.
In teeth associated with periapical lesions, the challenge is much more substantial in the form of removal of established bacterial biofilm in the apical root canal anatomy. The larger the lesion, the greater the infection diversity (Sundqvist, 1976), and the challenge of its eradication (Bystrom & Sundqvist, 1981). In this scenario, the responses to the adopted treatment protocols in the hands of different clinicans vary substantially, offering a spectrum of effectiveness in microbial control and thus outcomes. The predictablity of outcomes is therefore starkly different at the two ends of the biological spectrum.
The immediate effects of bacterial load reduction may be evident in the root canal system straightaway through the culture test but periapical healing shows latency, taking months, if not years to fully manifest. The majority of periapical lesions heal within 1 year (Azim et al., 2015; Ng et al., 2011a, 2011b) but some can take up to 4 years or longer (Strindberg, 1956). The follow-up of cases presenting with widened apical periodontal ligament space for 10 years revealed unfavourable future healing only in a small proportion of the cases (28%, 4/14) (Halse & Molven, 2004). The persistence of inflammation in the periapical tissues (Nair et al., 2005) is attributed to persistent residual infection in the apical anatomy, plus the effect of any extruded root filling material (Matsumiya & Kitamura, 1960; Nair et al., 2005; Vera et al., 2012).
Optimal technical completion of root canal treatment is one of the most tactile-skill-dependent procedures in the surgical field and attracts dental artisans with a passion and obsession for such finely detailed work (including the desire to deploy available tools and gadgets), committing the practitioner to a focus on the technical elements. This does not absolve the clinician or process of disease management from the usual host of meta-cognitive decision-making, including biological, patient-related, organization-related, and management-related. The pre-eminent biologically important outcome of such treatment, intra-canal bacterial load control, is at the best, a side-effect of the technical and chemical procedural manipulations rather than a direct and conscious act of observable microbicide. The dentist may have conscious or unconscious microbicide intent (clinician thinking about the microbes and their killing) but the greater part of the mental focus will generally be concentrated on the technical outcome; namely the “root-filling aesthetic” (flow, centeredness, apical extension, smoothness, and homogeneity). This dissociation between the technical and biological elements, which in some practitioners may cause cognitive dissonance (Seltzer & Bender, 2003), was aptly captured by Noyes (1922), a hundred years ago (“We are not trained to think in terms of biological concepts, but we are to act in mechanical procedures”) and by Naidorf (1972) 50 years ago (“The preoccupation of dentists with “techniques” has channelled endodontics into a state of technical excellence that often is not accompanied by a biologic awareness of the basic pathologic problems with which we are dealing or the biologic consequences of our therapy. The schism between clinicians & basic scientists is propagated by a tendency of each group to confer with themselves rather than with each other”). This problem remains prevalent today because despite advances in biological understanding of the disease process, the principles of treatment have not changed and remain technically focussed.
Despite the attempts of mainly clinical academics to change the status quo (Bergenholtz & Spangberg, 2004; Naidorf, 1972; Noyes, 1922), the product market has largely persuaded the business part of the system that efficiency and profit should remain the key priority and focus. Hence the danger of habituation with and over-reliance on type of tool and gadget. Clinical outcome research might yet prove the uniting element by aiding the synthesis of the different strands of influence (biological, biomechanical, technical, clinical) into a coherent picture of how root canal treatment might work and thus what may be required to evolve the procedure further to an even more effective or consistently predictable solution.
Outcome measures of root canal treatment
The uncertainty in outcome, created by periapical healing latency, possibly led to alternative quality control measures during root canal treatment, such as the culture test as deployed during the focal infection era. The test fell out of favour in contemporary practice, not least because root canal treatment had already become widely accepted (Molander et al., 1996a, 1996b) but also the procedural step was percieved to compromise cost-effectiveness. The postoperative absence of clinical signs and symptoms, coupled with radiographic evidence of technically optimal root-filling have become established in routine practice as the immediate (and sometimes the final) outcome measures at completion of the procedure (Bender et al., 1966a, 1966b).
Prediction of prospective periapical healing is informed by postoperative absence of signs of infection and inflammation, including absence of pain, tenderness to pressure/percussion of the tooth, tenderness to palpation of the associated soft tissues, swelling and sinus. In the medium term it may be informed by radiographic reduction in periapical radiolucency size, ultimately to lead to normal periodontal ligament space (Ng et al., 2007). The ideal histological goal would be periapical tissue regeneration with cementum formation over the apical termini to biologically isolate the root canal system.
Clinically, the periapical status of root-treated teeth is assessed using radiographic imaging, typically the conventional two-dimensional variety, which despite compressing 3D into 2D data and reducing sensitivity through anatomic superimposition, especially for molars (Huumonen et al., 2003), gives a sufficient indication of progress. In order to standardize radiographic interpretation, a five point scale for measuring periapical healing, the periapical index (PAI) (Orstavik, 1996; Orstavik & Horsted-Bindslev, 1993) has been used but it precludes direct comparison with dichotomous data, except by pooling the five scores into “healthy” (PAI 1 or 2) or “diseased” (PAI 3–5) states (Orstavik et al., 1987).
Three-dimensional imaging in the form of cone-beam computed tomography (CBCT), overcomes such anatomical superimposition and improves sensitivity (de Paula-Silva et al., 2009; Kanagasingam, Hussaini, et al., 2017; Kanagasingam, Lim, et al., 2017; Patel et al., 2009; Petersson et al., 2012; Sogur et al., 2009; Stavropoulos & Wenzel, 2007). Routine use of CBCT for diagnosing periapical status is not recommended (Brown Jacobs et al., 2014; Holroyd & Gulson, 2009; Patel et al., 2019; Scarfe, 2011) owing to its higher radiation dosage (×2–3) (Arai et al., 2001; Holroyd & Gulson, 2009). The higher sensitivity of CBCT for judging periapical status (Kruse et al., 2017, 2019; Liang et al., 2011; Patel et al., 2012), yields lower healed rates and longer durations for complete healing. It may be noted though that the periapical diagnostic accuracy of CBCT may be lower for root-filled teeth compared with non-root-filled teeth (Kruse et al., 2019) due to beam-hardening artefacts.
Periapical healing is only judged to be successful when the surrogate measures of both radiographic and clinical criteria have been satisfied (Friedman & Mor, 2004; Ng et al., 2007); persistent symptoms can arise in a small proportion of cases despite complete radiographic resolution (Polycarpou et al., 2005) and may be due to neuropathy. It is a moot point whether the neuropathy is correlated to delayed healing and a subtle surrogate measure for ongoing healing.
The dichotomous criteria for discriminating successful or failed periapical healing proposed by Strindberg (1956) have been widely adopted or adapted and embrace both radiographic and clinical elements (Table 1). Friedman and Mor (2004) suggested the alternative terms “healed”, “healing” and “diseased” to avoid seeding confusion from the patients' perspective. Nevertheless, the terms concur, the “healed” category corresponding to Strindberg's (1956) “success”, and “healing” corresponding to (Bender et al., 1966a, 1966b) “success” (Table 1). The length of time taken for complete periapical healing requires extended study periods, which are, in turn, accompanied by recall rate declines at the longer follow-ups. Some observers therefore accept a looser (Ng et al., 2007) or more lenient (Friedman & Mor, 2004) threshold for success at partial (reduced lesion size) rather than complete healing, the latter described as “stricter” (Ng et al., 2007) or a “more stringent” (Friedman & Mor, 2004) measure. Adoption of shorter duration recall, tacitly assumes a continuously linear healing scale to predict the longer term outcome but healing-dynamics studies do not support this notion (Bystrom et al., 1987). Healing rates vary and those for large lesions are often faster and for small lesions slower (Esfahani, 2016).
| Strindberg (1956) | Bender et al. (1966a, 1966b) | Friedman and Mor (2004) |
|---|---|---|
|
Success: Clinical: No symptoms Radiographic: The contours, width and structure of the periodontal margin were normal, or The periodontal contours were widened mainly around the excess filling. |
Success: Clinical: Absence of pain/swelling Disappearance of fistula No loss of function No evidence of tissue destruction Radiographic: An eliminated or arrested area of rarefaction after a post-treatment interval of 6 months to 2 years |
Healed: Clinical: Normal presentation Radiographic: Normal presentation |
|
Failure: Clinical: Presence of symptoms Radiographic: A decrease in the periradicular rarefaction, or Unchanged periradicular rarefaction, or An appearance of new rarefaction or an increase in the initial rarefaction. |
Diseased: Radiolucency has emerged or persisted without change, even when the clinical presentation is normal, or Clinical signs or symptoms are present, even if the radiographic presentation is normal. |
|
|
Uncertain: Radiographic: There were ambiguous or technically unsatisfactory control radiographs which could not for some reason be repeated; or The tooth was extracted prior to the 3-year follow-up owing to the unsuccessful treatment of another root of the tooth. |
Healing: Clinical: Normal presentation Radiographic: Reduced radiolucency. |
This narrative review on the outcomes of root canal treatment seeks to understand the nature of root canal treatment through integration of outcome data with associated biological, chemical and biomechanical data to offer explanations of the nature of the process and the probable reasons for the observed outcomes.
OUTCOMES OF NON-SURGICAL ROOT CANAL TREATMENT
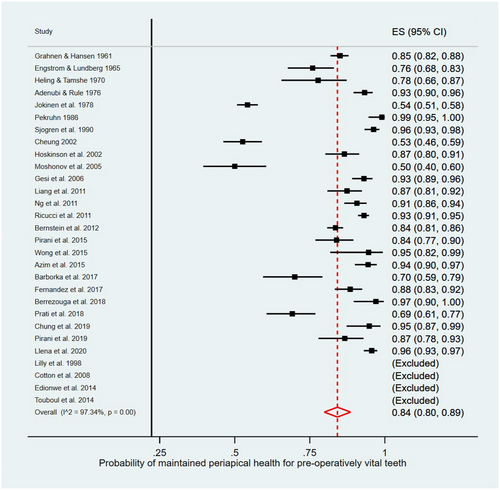
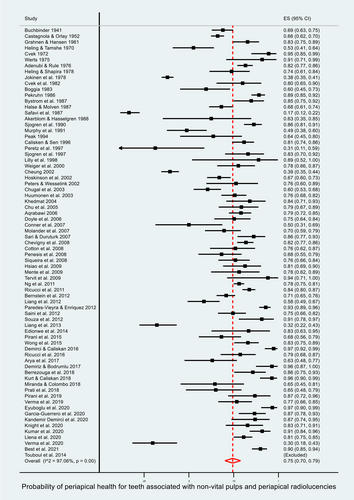
Numerous systematic reviews and meta-analyses have been performed on outcomes of root canal treatment since those published by the authors on the factors affecting primary root canal treatment (Ng et al., 2007; Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008). The authors have continued to use their published methods to update their meta-analyses (with new and emerging data to the end of 2020) (Random effect metaprop or metan, STATA IC version 16.1, STATA Corporation), although only published in textbook chapters. The updated meta-analyses reveal that 84% of vital pulpectomy cases retain the absence of apical periodontitis (Figure 2) but apical periodontitis cases result in the absence of apical periodontitis in 74% of cases (Figure 3).
Factors that affect periapical health status following root canal treatment
Root canal treatment is subject to enormous variation in the way it is performed depending on interpretation and execution of any given protocol by an operator, not to mention the variations imposed by the environment and patient requirements. Root canal treatment is a multi-step procedure, where each sequential step is dependent on the adequacy of the previous for its cumulative efficacy. From a research perspective, characterizing and accurately recording variations in protocol execution is massively challenging because of the range and scope of variables to be recorded. Not only the individual steps (factors), but also any interaction between them must be accounted for. All of these factors cannot be randomized, only some may be amenable to control in well-designed and executed randomized controlled trials, data on other factors may only be recorded and remain at risk of bias, particularly due to recruitment or drop-out problems. Strict participant (patient and dentist) selection may aid control of cohorts and compliance with protocols but by virtue of that control, may limit the generalizability of findings. In addition, the effects of pre-operative factors and some treatment steps cannot be randomized and can only be accounted for or investigated in observational studies. Well-designed randomized controlled trials, coupled with population-based observational studies, therefore provide better complementary insight (Booth & Tannock, 2014). In this context, the value attributed to a study is better judged by the quality and utility of the emergent data than the design, per se.
- Patient and tooth factors (age, sex, general health or immune status, tooth anatomy, pre-operative pulpal and periapical status);
- Treatment factors (operator characteristics, tooth management and isolation, canal system access, working length control at all stages, canal shaping/enlargement, irrigation, medication, culture test outcome and obturation); and
- Postoperative restorative factors (amount, distribution and quality of remaining tooth structure and its integrity, type of restorative material, full or partial coverage, timing of permanent restoration, quality and maintenance of marginal adaptation, abutment or non-abutment, and occlusal dynamics).
Some of these factors have a profound impact on periapical healing, whilst others show a negligible effect or had not accrued sufficient evidence. Patient and tooth factors characterizing the nature of disease consistently show the most potent effect (periapical status), whilst most of the treatment factors, individually, exert only a weak effect, except for the apical extent of root canal filling (treatment) relative to the root apex (root canal terminus), the quality of root-filling, and the quality of the postoperative restorative care, which show profound influences on periapical health. Systematic reviews, triangulation from individual studies, and intuitive synthesis (Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008), suggest that the main and most important factors already stand revealed, even though the quality of individual studies may often be judged sub-optimal by various published study quality measures. Confidence in the reliability of the data may be asserted through the statistical measures deployed and is often the most common form of indication in published works. It cannot be over-emphasized though that the prior deep personal study of the raw rather than the synthesized data, confers a much greater sense of perspective, understanding and confidence in the findings. It is the former type of knowledge rather than a summary synthesis that serves to knit together a thorough biological, clinical and technical understanding of how the procedure works, forming a key part of the domain knowledge underpinning expertise (Ericsson, 2009; Ericsson et al., 2018).
Each of the main and subgroup of factors that may influence outcomes of root canal treatment are now analysed and synthesized with other evidence to understand the probable underlying mechanisms.
Patient and tooth factors
Effect of age, sex, health
The routinely collected demographic data on factors such as the patient's age and sex, show no significant influence on root canal treatment outcome, even though youth and old age may be anticipated to produce some effect through immune responsiveness. A proportion of the variation in periapical healing outcomes may be attributed to differences between individual patients' host responses (Ng et al., 2011a, 2011b; Yee, 2019). Although, the notion is further supported by the weak influence of “general health” of the patient on periapical healing, specific health conditions, such as diabetes (Doyle et al., 2006; Fouad & Burleson, 2003) and “compromised innate immune response” (Marending et al., 2005), may have a significant influence, although with limited evidence for the mechanistic pathway and strength of effect. Emerging evidence suggests that polymorphisms of various genes involved in periapical healing may have an effect on outcomes (Farmani, 2018; Mazzi-Chaves et al., 2018; Morsani et al., 2011; Petean et al., 2019; Rocas et al., 2014; Silva-Sousa et al., 2020; Siqueira et al., 2009, 2011).
Effect of tooth type
The commonly accepted perception that single-rooted teeth must exhibit a higher rate of periapical healing than multi-rooted teeth, is shown to be untrue by the collective data, as well as the majority of individual studies. This entirely plausible preconception is driven by the simpler canal anatomy, easier access, and comfort of dentists to complete root canal treatment in such teeth. In sharp contrast, posterior teeth harbour more difficult access, unpredictable canal numbers and location, complicated canal negotiation and enlargement due to severe and multiple canal curvatures, as well as the perception of difficulty and likelihood of failure (Laukkanen et al., 2021). The psychologically greater prospect of being daunted by treating molars may prevent dentists from embarking on such treatments and thus there may be a bias in those undertaking posterior tooth root canal treatments. The rare studies (Benenati & Khajotia, 2002; Field et al., 2004) that find in favour of anterior teeth generally have not considered the confounding effect of periapical disease, which once accounted for, reveal that tooth type does not exert a strong influence on periapical healing rates. That the studies collectively find no overall difference between anterior and posterior teeth is an extremely powerful message about the factors influencing outcome rather than being a confounded outcome as is sometimes supposed (Al-Nuaimi et al., 2018; Patel et al., 2012). The most logical and obvious explanation for this lack of difference in periapical healing between anterior and posterior teeth must lie in the dominance of the impact of “apical canal complexities” (and their interaction with infection) rather than “canal system complexities” (Azim et al., 2015); the parameter of “apical canal complexities” may exhibit greater similarities between different tooth and root types.
Effect of pulpal and periapical status
The preoperative pulp status (vital or necrotic) has no influence on the outcome of periapical healing (Rossi-Fedele & Ng, 2022), unless there is, in addition, an associated periapical lesion (Rossi-Fedele & Ng, 2022), that is, the canal system is infected. Necrotic pulp tissue neither causes apical pathosis nor influences its healing (Moller et al., 1981). Periapical healing is predominantly and powerfully influenced by the presence and size of the preoperative periapical lesion (Ng et al., 2011a, 2011b; Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008), which therefore carries a huge confounding risk when analysing the influence of any other factor. The periapical lesion typically signals infection in the complex apical canal anatomy, which is known to be difficult to control (Nair et al., 2005; Vera et al., 2012). The even greater negative influence of larger periapical lesions may be attributed to the greater diversity of bacteria (number of species and their relative abundance) in such teeth (Sundqvist, 1976), making the infection even more difficult to control (Bystrom & Sundqvist, 1981). Other, mainly speculative explanations for a negative influence of larger lesions are that they may have longer-standing infections with deeper penetration of bacteria in dentinal tubules and accessory anatomy (Shovelton, 1964) and potentially represent cystic transformation (Nair, 2006), or a more exaggerated host response that may in turn fail to switch off in the presence of residual bacteria (Nair et al., 2005).
Other negative preoperative factor influences on outcomes, such as pain, tenderness of tooth to percussion, tenderness of associated soft tissues to palpation, associated swellings or sinus tracts, periodontal probing defects of endodontic origin and root resorption may all represent a more aggressive periapical host-microbial interaction with greater tissue destruction and therefore reduced potential for periapical tissue regeneration (Weiss, 1966). The negative influence of sinus tract and swelling (chronic and acute forms of suppuration, respectively) may also be related to proliferation of microbiota into the periapical tissues, presumably hindering or delaying periapical healing.
Effect of tooth integrity
Preoperative clinical evidence of compromised tooth structure, such as in the form of reduced amount, distribution, quality (sclerosed dentine) or integrity (cracks) of enamel or dentine may reduce the prospect of periapical healing (Al-Nuaimi et al., 2018; Sim et al., 2016; Tan et al., 2006). This important factor is considered further under postoperative factors.
In summary, the preoperative clinical finding of periapical lesion, particularly of large size, with preoperative pain (Friedman et al., 1995), sinus tract (Ng et al., 2011a, 2011b), swelling (Ng et al., 2011a, 2011b) and apical resorption (Strindberg, 1956) are negative prognostic factors significantly reducing the probability of periapical healing after root canal treatment. The presence of these factors signals a clear message to the clinician of the potential biological challenges facing management of the tooth without yet having considered the technical treatment challenges. In addition, compromised coronal tooth structure or the restoration interface, also reduces the prospect of periapical healing, presumably by reducing the prospect of sustaining control of the internal tooth environment and its infection.
Treatment factors
The technical versus biological conundrum
As already mentioned, the paradox of the importance of biological insight over technical skill in the performance of root canal treatment was highlighted a 100 years ago (Blayney, 1922; Noyes, 1922) and remains pertinent today. Although clinicians may psychologically feel that their treatment imposes the greatest influence on periapical healing, through the effortful precision of their technical execution and consequent bacterial load reduction (Bystrom et al., 1985; Bystrom & Sundqvist, 1981, 1983, 1985), the precise relationship between their practical (mechanical and chemical) steps and bacterial demise are unclear and only rudimentarily charted. The technical complexity of root canal treatment typically “diverts” the dentist's attention towards the technically challenging tasks of gaining access, finding the canals, negotiating them without blockage, enlarging them without iatrogenic error, disinfecting the geometrically complex root canal space, and filling it completely without extrusion. It takes a diligent and biologically insightful dentist to keep the technical and biological elements intertwined in mind and execution. For example, improvements in the technical quality of root-fillings through training in Nitinol (NiTi) instrumentation and single-cone root-filling did not result in a parallel improvement in periapical healing status (Koch et al., 2014). This may suggest that reducing the technical burden of instrumentation alone through adoption of NiTi instruments, is insufficient. The question of whether a “biologically oriented” or a “technically oriented” practitioner might enjoy higher rates of periapical healing is an interesting but sparsely explored research question.
Effect of operator skill and knowledge (competence)
The general theme of the previous section is continued along a specific line in this section. The impact of operator insight and skill (using the surrogate measure of training qualification and experience) has been investigated to a limited extent. Clinicians with higher educational or training backgrounds (amongst undergraduate students, general dental practitioners, postgraduate students and specialists) display outcome rates commensurate with their training and experience level (Ng et al., 2007). It is difficult to segregate the complex constellation of cognitive, technical and clinical skills expressed by the dentist in completing the treatment. It is not just the refined and insightful technical execution that matters, but also how the overall understanding of the biological problem influences the operators' intra-operative decision-making, especially, the motivation and integrity with which the procedure is performed (elements difficult to measure) (Ericsson et al., 2018).
The authors' Eastman study, using multi-level modelling, accounting for the relative influence of operator, patient, tooth and procedure on periapical healing and iatrogenic outcomes, revealed only a moderate degree of operator influence (14% of total variation) on periapical healing and an even smaller degree (4% of total variation) on iatrogenic errors (Yee, 2019). Meanwhile, patient-level characteristics accounted for 17%, and tooth-level 69%, of the total variation of the healing outcome. Patient-level (26%), and tooth-level (70%) characteristics accounted for most of the variation of the iatrogenic error outcome. The findings imply that the dominant influence on outcomes comes from factors not completely under the direct and independent control of the operator but are a function of the nature of interaction of the operator with the patient- and tooth-related factors. That is to say, the expertise with which the operator negotiates the presenting clinical and biological problem may have the greatest “operative” bearing on the outcome. Contemporary tools and protocols alone, do not yet allow direct and absolute control (predictable management) over cases with high biological and technical complexity.
Deconstruction of root canal treatment into its procedural steps
Root canal treatment may be deconstructed into procedural components to evaluate their individual impacts on the final composite outcome. The procedural components might include rubber dam isolation, access preparation, canal system identification and location, canal negotiation, length determination, canal enlargement parameters, lavage and disinfection of the canal system (conventionally called irrigation and medication), and obturation. The afore-mentioned inter-dependence of the procedural steps means that to apportion the effect of treatment on periapical healing to any one step, as well as to any interaction between them, requires comprehensive prospective data collection coupled with sophisticated statistical analysis.
Effect of rubber dam isolation
The universally recommended but often neglected rubber dam isolation in modern root canal treatment has not been robustly tested for its effect on the outcome of periapical healing. Incidentally, one observational study on root canal retreatment (Van Nieuwenhuysen et al., 1994) found a significantly higher periapical healing rate when rubber dam was used, compared with cotton roll isolation. Another reported a significantly lower prevalence of periapical lesion development after post placement in root canal-treated teeth under rubber dam (Goldfein et al., 2013). The additional benefits listed for adopting rubber dam isolation include safety (prevention of instrument inhalation), medico-legal compliance, improved access, and a controlled and disinfected operative field (European Society of Endodontology, 2006).
A randomized controlled trial comparing root canal treatment with or without rubber dam isolation is highly unlikely to yield a significant difference in periapical healing. This is because the major influence on outcomes is conferred by the established infection in the apical anatomy, which is unlikely to be altered by any transient coronal salivary contamination. Given the minimal effect coronal salivary contamination has on an exposed pulp over many days (Cox et al., 1985), any minor contamination during root canal treatment is unlikely to alter the apical biofilm physiology and established host-microbial dynamics. The key value of rubber dam isolation is in securing control of the operative field during the procedure to allow the necessary meticulous completion of stepwise tasks of root canal treatment with control, precision, and diligence.
Effect of access cavity design
The entry hole through the occlusal surface of the tooth to the root canal system is called the “access cavity”. Its shape and location (or design) are dictated by the precise anatomical juxtaposition of the pulp chamber to the tooth surface providing the most direct access to the chamber and/or straight-line trajectory to the apical parts of the root canal system. The location, direction and size of the access cavity should be tailored to balance the needs of canal access and minimization of tooth structure damage that might affect the tooth's strength or aesthetics (Mannan et al., 2001), assuming the operator has appropriate and precise orientational control over the cutting tool.
The pendulum has gradually and rightly swung towards adopting more conservative access cavities in the interests of maintaining tooth strength, but the trend has irrationally continued towards conservative extremes that may potentially compromise root canal debridement; indeed, such miniscule cavities were once labelled as “errors” in the annals of root canal treatment (Stock, 1988).
Nevertheless, 3D CBCT data have enabled the design and execution of ultra-conservative access cavities (or “ninja access cavities”) aiming to preserve dentine and increase tooth survival (Plotino et al., 2017). A prime goal of restoring root-treated teeth is tooth structure preservation and protection, so that in biomechanical function, they exhibit more favourable stress distribution (Wang et al., 2020); however, whether these cavities increase fracture strength in vivo and elongate long-term tooth survival remains unknown (Ozyurek et al., 2018; Sabeti et al., 2018). The most important question about ultra-conservative access cavity designs is whether they compromise root canal system preparation, debridement and obturation, which has only been addressed in laboratory studies (Tufenkci & Yilmaz, 2020); longer-term clinical trials are awaited to demonstrate improved periapical healing and tooth survival. In the meantime, conventional access cavities serve their purpose to aid predictable facilitation of root canal treatment without compromising periapical healing or survival outcomes.
Effect of use of magnification and illumination
Having accessed the pulp chamber, optimal visualization of its floor to identify all canal orifices and negotiate (or “thread”) them with instruments for enlargement, benefits from good illumination, and if possible, magnification. Indeed, some operators even use magnification and illumination for preliminary stages such as anaesthesia and access cavity preparation, which makes little sense, since these elements require broader 3D perspective for correct orientation, which may be lost under certain types of magnification. The virtues of magnification and illumination during the root canal location and negotiation phase and indeed for most of the root canal treatment procedure are almost universally extolled by Endodontists (Patel & Rhodes, 2007) because of the “feeling” of control over the process. In addition, it may aid location of all canal orifices, although each of these lead to a single pulp canal system, unless the canal is completely separate. It is worth noting that the canal orifices at the root apex are more important for periapical healing than those in the pulp chamber. In any case, systematic reviews have failed to identify objective evidence for improved periapical healing outcomes related to utilization of magnification (Del Fabbro et al., 2009; Ng et al., 2011a, 2011b), other than in assisting location of additional canals (Ng et al., 2011a, 2011b). A definitive view on the benefit of a microscope on periapical healing outcomes may perhaps emerge through a randomized controlled trial but on current evidence and the fact that the main barrier to improved periapical healing is control of the invisible apical intra-radicular infection, a positive effect is highly unlikely.
In the context of expertise development, it is also worth noting that “threading” a canal “without looking” is something seasoned endodontists can do. It is a composite skill involving practical knowledge of anatomy, tactile sensitivity and mental visualization that incorporates the ability to “mentally see” and physically traverse a “flight path” that enables the clinician to place a file into the canal with relative ease. Reliance on microscopes may potentially override the development of such a skill, which is a prelude to the tactile skill required for further apical negotiation into the unknown curvatures and apical foramina beyond (Ericsson et al., 2018).
Effect of negotiation of instruments to the canal terminus
The ability to negotiate the main canal system channels (“canals” are expanded parts of the system that allow files to traverse a path from coronal entry to apical exit) to their termini with a root canal instrument has been identified as the single most important treatment factor contributing to a favourable periapical healing outcome in teeth with apical periodontitis (Ng et al., 2011a, 2011b; Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008). The same may not be true for teeth without apical periodontitis (Byström, 1986; Cvek et al., 1976), where reaching canal termini is not essential and may even jeopardize periapical status (Chugal et al., 2003; Seltzer et al., 1969, 2004). These findings make absolute biological sense.
In the case of teeth without apical periodontitis, it is likely that the pulp stumps in the apical delta are still viable, healthy, and uninfected. This coupled with the fact that the narrowing of the neurovascular bundle with the approach to the exit, also concentrates the fibrous element of the connective tissue (by reduction in the ground substance), creating the “pulp stump”, where the pulp typically tears on extirpation (Seltzer et al., 1969, 2004). Maintaining such pulp stumps by preparing short of the canal terminus, better prevents the development of apical periodontitis, subsequently (Ng et al., 2011a, 2011b; Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008; Seltzer et al., 1969).
In the case of teeth associated with apical periodontitis, the entire purpose of root canal treatment is to gain full access to the complex apical anatomy to enable its disinfection. Without securing this requisite, the treatment is doomed to fail as there is little opportunity to influence the apical infection, except by the fortuitous interception of ecological shift in the microbiota incurred by any attempts thereof. It is emphasized that access to the entire apical anatomy (including all the multiple exits) must be secured and not just the single exit that the negotiating file might happen to traverse. Over-focus and over-instrumentation of that randomly selected single exit (by dint of trajectory), without adequate irrigation, may risk blocking the other apical canal delta tributaries and their infected exits. The presence and infection of multiple apical exits is typically betrayed clinically by the size and distribution of the periapical lesion about the root apex, a sign to which the informed clinician will be alerted.
It is well accepted that root canal system disinfection should extend to its apical termini. The goal may be expressed in different ways in the outcome literature as extension to the “apical constriction”, “0.5–2 mm from the radiographic apex”, or “cemento-dentinal junction” (European Society of Endodontology, 2006). “Patency at canal terminus” and “apical extent of canal instrumentation” were the only significant prognostic factors for root canal treatment amongst those related to mechanical preparation of canals (“type of instrument”, “patency at canal terminus”, “apical size”, “taper and extent of canal instrumentation”), which are putatively measures of the apical extent of canal cleaning (Ng et al., 2011a, 2011b). Achieving technical patency at the canal terminus significantly increased the odds of periapical healing 2-fold (Ng et al., 2011a, 2011b), whereas the odds of successful healing was reduced by 12%–14% for every 1 mm of the canal short of the terminus that remained “un-instrumented” (Chugal et al., 2003; Ng et al., 2011a, 2011b). It is worth noting that sometimes, the natural anatomy or iatrogenic faults preclude achievement of “mechanical” or “physical” patency but nevertheless an electronic apex locator (EAL) may still give a reading (Abdelsalam & Hashem, 2020), albeit short of “zero”. This infers the existence of “electrical patency” or continuity of a conductive medium to the canal terminus. In such circumstances, active irrigation with sufficient pressure may facilitate some apical debridement (Lorono et al., 2020) by allowing penetration of the irrigant further than the instrument. A completely blocked canal would disable electrical continuity and hence complete circuit, so an EAL would show “no reading”; a signal that the potential for apical irrigation is non-existent.
It may be stated categorically and with confidence that one of the major goals of root canal treatment in teeth with apical periodontitis, is to obtain and maintain apical canal patency for predictable root canal treatment (Ng et al., 2011a, 2011b; Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008). This conceptually simple goal is, practically, one of the most difficult things to achieve and is where many root canal treatments flounder at an early stage in the hands of a novice. Obtaining patency, and maintaining it, is a key tactile skill in root canal treatment and typically requires the use of stainless-steel instruments for sensitive and controllable scouting and negotiation. Such negotiation must be accompanied by judicious irrigation and lubrication with sodium hypochlorite and or EDTA (Ng et al., 2011a, 2011b) to avoid blockage, which is a risk throughout this process. Lack of mechanical negotiability of canals may be attributed to many factors including the presence of undetected acute curvatures, division of the main canal into a fine plexus of apical canals, natural obstructions (“denticles”, pulp stones, tertiary dentine), or dentine/organic debris accumulation because of poor instrument control or irrigation (Seltzer et al., 2004).
Effect of mechanical root canal enlargement to the canal terminus
In the original conceptualisation of root canal treatment, the mechanical preparation of the canal held a pre-eminent place in debridement by virtue of its association with removal of “infected material and dentine”. It was believed that the canal terminus diameter should be enlarged (Crane, 1921), by at least three file sizes (Grossman, 1970). The purpose of canal enlargement has undergone a conceptual paradigm shift and is now described as sufficient selective sculpting of the canal wall to facilitate the delivery of irrigants and medicaments for disinfection, followed by delivery of the root filling material to the entire boundary and volume of the root canal system (Gulabivala et al., 2005). It is this paradigm shift, which has propelled the focus and drive for research on root canal irrigation over the last two decades; and seen the proliferation in irrigation devices available commercially. The precise dimensions and optimal shape to facilitate these elements remain a matter of debate because available laboratory and clinical studies suggest that a diverse range of shapes and sizes can all potentially fulfil the purpose (Baugh & Wallace, 2005). The question of precise dimensions is impossible to answer definitively because the combined chemical and mechanical preparation effects (chemo-mechanical) cannot be divorced from each other as they are intimately interlinked and interdependent. The lack of definitive correlation between the physical dimensions of the machined preparation and microbial control is understandable because microbial ecological shift rather than size and shape of the prepared canal terminus influences the outcome (see section on “Quality control of root canal disinfection and persistent bacteria”).
The prime reason for root canal enlargement is to enable irrigant delivery into the small volume of the root canal system, which makes liquids behave like solids in their flow characteristics; expansion of the canal volume marginally improves the flow of irrigant fluids. Other variables that might influence fluid flow include the irrigant's viscosity, density, length scale and velocity (Gulabivala et al., 2010).
A variety of instruments of different cutting designs, tips, tapers, diameters, materials of construction and series transitions (multiple instrument series to single file), have been deployed to mechanically enlarge root canal systems to defined apical sizes and tapers (Schilder, 1974). Numerous laboratory studies testify to their properties, efficacy and utility (Hülsmann et al., 2005), but their efficacy in clinical canal enlargement has been evaluated in only three prospective observational studies (Koch et al., 2014; Ng et al., 2011a, 2011b; Pettiette et al., 2001). In one (Ng et al., 2011a, 2011b), the better success rates for NiTi instruments (hand or rotary) compared with stainless steel instruments were attributed to prior tactile skill development using stainless steel files by the senior students. The ability to gain and maintain apical patency as well as to avoid procedural errors would be better instilled in such students through progressive and continual coaching. A further confounding factor in the study may be that such senior trainees would also be more likely to have established a better understanding of biological rationale and effective intra-operative decision-making. NiTi instruments also appear capable of achieving the same in selected mild to moderate complexity primary root canal treatment cases undertaken by undergraduates (Pettiette et al., 2001).
The effect of apical size of canal preparation on treatment outcome has been considered in a number of studies (Hoskinson et al., 2002; Kerekes & Tronstad, 1979; Ng et al., 2011a, 2011b; Saini et al., 2012; Souza et al., 2012; Strindberg, 1956). Enlargement of the canal to three sizes larger than the first file to bind apically led on average to an apical size of ISO 30, which was sufficient for periapical healing in a randomized controlled trial (Saini et al., 2012). Observational studies (Hoskinson et al., 2002; Ng et al., 2011a, 2011b; Strindberg, 1956), not specifically designed to test the effect of apical canal size found no statistically significant influence attributable to this factor but all reported the same inverse trend of decreasing periapical healing rates with increasing size of apical preparation, which seems counter-intuitive and unexpected. Two explanations may be advanced for this clear trend from three independent studies. One is that larger apical preparations may be prone to incur iatrogenic errors, such as blockage, transportation and ledging. A second explanation is that larger apical preparations would generate more dentine debris with a greater propensity to block bacterially contaminated apical canal exits that had not been instrumented. The effect would be further confounded by a coupling with a poor irrigation regimen, thus potentially jeopardizing periapical healing.
The apical stagnation zone and vapour lock phenomena that hamper irrigation may act in concert with the generated dentine and organic debris to allow it to congeal from a “slurry” into “dentine mud”, to create either a passable (“pick-able”) or unpassable (“unpick-able”) blockage. Faced with this scenario, the impatient or neophyte dentist typically forces the instruments to regain their designated length(s), resulting in the classically described procedural errors of apical transportation, canal straightening, ledging and perforation (Gulabivala et al., 2010). These explanations do not account for the higher failure in initially large canals, where presumably immature roots present a different debridement challenge. In such cases, where the canal shape is less amenable to planing by conventional instruments, it is speculated that an intracanal brush with a larger effective diameter may provide better debridement (Gu et al., 2009). Available study outcomes reject the intuitively “logical” notion of more effective bacterial debridement with larger apical preparations (Card et al., 2002; Parris et al., 1994; Rollison et al., 2002).
The principle of considering chemical and mechanical (or chemo-mechanical) debridement together, applies equally well to the apical size and taper of the canal. Guideline (European Society of Endodontology, 2006) recommendations stipulate only that canal preparation should be tapered from crown to apex; a minimum taper size is not indicated. Intuitively, this makes perfect sense because of the natural tapering shape of roots. Even this parameter elicits a paucity of sufficient direct evidence for its influence on root canal treatment outcome. Observational studies (Hoskinson et al., 2002; Ng et al., 2011a, 2011b; Smith et al., 1993), incidentally reporting on the effect of canal preparation taper on primary treatment and retreatment outcome give no specific recommendation either. Smith et al. (1993) found a “flared” preparation (wide taper) resulted in a significantly higher rate of periapical healing compared with a “conical” preparation (narrow taper), using loose criteria; the taper sizes were not specified, and potential confounders were uncontrolled. Other studies (Hoskinson et al., 2002; Ng et al., 2011a, 2011b) using strict criteria, found no significant difference between narrow (0.05) and wide (0.10) canal tapers, achieved using stainless steel ISO files. The latter study (Ng et al., 2011a, 2011b) also compared stainless steel file stepback preparation (0.05 and 0.10) and tapers of 0.04, 0.06, and 0.08 (achieved using non-ISO, greater taper, nickel–titanium instruments) but again found no significant difference in treatment outcome associated with them. They cautioned that the absence of randomization in their study could result in confounding from the initial canal size, instrument type and operator experience. Creation of 0.05 (1 mm step-back) or 0.10 (0.5 mm step-back) tapers using stainless steel instruments demands trained, controlled, manipulation with tactile sensitivity to avoid over-instrumentation, which can readily produce a much greater diversity of tapers and shapes, confounding the outcomes.
Despite the disparate and “sub-gold standard” level of evidence, triangulation of available data on the effects of prepared canal taper on periapical healing outcome, intuitively suggests over-enlargement of canals is unnecessary to achieve periapical healing. Apical preparation size of ISO 30 coupled with a minimal 0.05 taper is more than sufficient, conditional upon adequate irrigation. The chemical, biological and hydrodynamic mechanisms required to be at play in “adequate irrigation”, however, remain elusive, although there is plenty of circumstantial evidence and speculation from laboratory studies (Gulabivala et al., 2010; Lee et al., 2004). Collaborations between fluid dynamics specialists (Gulabivala et al., 2010), (micro) biologists and endodontists (Gulabivala, 2004) may ultimately yield these answers.
Procedural errors during root canal preparation are more common amongst novices or junior dentists and are typically classified into canal blockage, uncontrolled canal shaping (ledging, apical zipping and transportation, straightening of canal curvature) tooth/root perforation (sub-classified into pulp chamber or radicular levels), or instrument separation. Amongst these, the effect of canal blockage has been reported above, whilst the influence of uncontrolled canal shaping has not been specifically investigated. Iatrogenic root perforations result in significantly lower chances of periapical healing (Cvek et al., 1982; de Chevigny et al., 2008a, 2008b; Imura et al., 2007; Marquis et al., 2006; Ng et al., 2011a, 2011b; Sjogren et al., 1990). MTA® has found favour as a contemporary perforation repair material, attributed to its biocompatibility and seal effectiveness (de Chevigny et al., 2008a, 2008b; Gorni et al., 2016; Main et al., 2004; Mente et al., 2010). The further specific effects of location and size of perforation, time lapse before defect repair, adequacy of perforation seal, and operators' experience, were found to have no significant influence on long-term outcome of root canal treatment with iatrogenic perforation repaired using MTA (Mente et al., 2014), However, a larger scale and longer term follow-up study reported that perforations of larger size, located in the middle third of canal and associated with a periodontal probing defect, had poorer healing outcomes (Gorni et al., 2016).
Instrument separation during canal preparation may reduce periapical healing success rates significantly (Ng et al., 2011a, 2011b; Strindberg, 1956) when there is pre-existing apical pathosis (Spili et al., 2005). The stage at which instrument separation occurs in relation to degree of prior canal disinfection may also influence the outcome. The prevalence of such errors ranges from 0.5% to 7.4% for stainless steel instruments (Panitvisai et al., 2010) and 1.3% to 10% for rotary nickel–titanium instruments (Madarati et al., 2013). The corono-apical location of separated instruments in the canal system had no effect on treatment outcome, however, whether they were successfully bypassed or removed to regain apical patency did make a positive impact on treatment outcome (Ng et al., 2011a, 2011b; Ungerechts et al., 2014).
These disparate outcome data all converge to make sense when viewed in the biological context of the purpose of root canal treatment as one of microbial load reduction through disinfection or infection prevention through asepsis. Instead of over-focusing on the details of mechanical preparation protocol, instrument types, their mode of manipulation, their sequence of use or canal segment priorities, it would be better to conceptualize the problem from the perspective of gaining and maintaining access to the infection in the apical canal anatomy and coupling the technical goals of canal enlargement with chemical debridement (Gulabivala et al., 2010). In conclusion, none of the mentioned factors on their own, have any significant impact on periapical healing, other than to individually contribute to or collectively conspire to help achieve the main goal of gaining patency and access to the apical infection for effective disinfection.
Effect of root canal irrigation
The role of root canal irrigation is inextricably linked with mechanical preparation and the conceptual ground for this section has already been laid in the last section. To advance the discussion, a diverse range of neutral or chemically active agents has been used to irrigate root canal systems. They have been used singly or in various combinations in clinical practice but not all of them have been systematically or purposefully investigated through appropriate laboratory, animal or clinical study models. The irrigants reported on include water/saline, local anaesthetic solution, sodium hypochlorite, iodine, chloramine, sulphuric acid, EDTA, hydrogen peroxide, organic acid, Savlon®, urea peroxide and Biosept® (quaternary ammonium compound) (Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008). The majority of studies used sodium hypochlorite as an irrigant (Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008) for primary or secondary root canal treatment, consistent with guidelines (European Society of Endodontology, 2006) recommending solutions possessing dual disinfectant and tissue-solvent properties.
Root canal irrigation has been demonstrated to have a significant impact on intracanal bacterial load reduction in clinical studies (Bystrom & Sundqvist, 1981, 1983), but counter-intuitively, the effect of different irrigants (with or without active antibacterial effect, even of different NaOCl concentrations) on periapical healing is not substantially different (Adenubi & Rule, 1976; Harty et al., 1970; Smith et al., 1993). This stark and surprising observation must also signal an important phenomenon demanding an explanation.
First, to report the consolidated findings, one prospective observational study (Ng et al., 2011a, 2011b) exploring the effect of irrigant on periapical healing rates following root canal treatment found that a higher concentration of sodium hypochlorite (5% vs. 2.5%) made negligible difference to treatment outcome. In other studies, too, higher concentrations of NaOCl did not yield the expected improved periapical healing or bacterial load reduction (Bystrom & Sundqvist, 1985; Cvek et al., 1976). This trend of absence of difference in bacterial load reduction (comparing 0.5% to 3.0% or 5.0% NaOCl) (Bystrom & Sundqvist, 1985; Ulin et al., 2020) or periapical healing (comparing 0.5% or 1% to 5% NaOCl) (Cvek et al., 1976; Verma et al., 2019) is consistent across studies.
The belief within the profession and the market that individual irrigant solutions did not possess all the requisite properties, led to the development of commercially branded and marketed mixed products to enhance overall potency (QMix™ 2 in 1 [Dentsply, Tulsa Dental Specialties], BioPure MTAD [Dentsply Tulsa Dental Specialties]). Such mixed solutions show promise in laboratory studies (Pappen et al., 2010; Wang et al., 2012) consistent with single pure solutions but again lack evidence (microbiological or periapical healing) in their clinical applications.
The most commonly adopted adjunctive agent to NaOCl, Ethylenediaminetetraacetic acid (EDTA), profoundly improves periapical healing rates by 1.3–2.3 odds for primary and secondary root canal treatment, respectively (Ng et al., 2011a, 2011b). The synergistic action of alternate irrigation with sodium hypochlorite and EDTA had already been demonstrated for bacterial load reduction (Bystrom et al., 1985) but long-term (≥2 years) periapical healing outcome (Byström, 1986) did not correlate with their microbiological findings. The synergistic effect between the two disinfectants had been attributed to the chelating properties of the sodium salts of EDTA and removal of the smear layer to expose deeper lying bacteria (Zehnder, 2006).
EDTA solution was originally recommended as a root canal irrigant to assist negotiation of narrow or sclerosed canals and for smear layer removal. EDTA has since also been attributed other functions, including the ability to aid loosening of compacted debris in the non-instrumented canal anatomy, facilitating deeper penetration of sodium hypochlorite solution into dentine by opening dentinal tubules (likely of dubious clinical value), and possibly most importantly for aiding breakup and detachment of biofilms adherent to root canal walls (Bryce et al., 2009; de Almeida et al., 2016; Gulabivala et al., 2005). Of all these justifications, the last function is probably the most important for improvement in periapical healing and the least recognized for it because of the erroneous focus and obsession with the “smear layer”, which is merely surface-deformed and displaced dentine. The question may be posed why dentine has this unique property of “surface smearing”; for which a hypothetical but plausible explanation might be that it is an evolutionary selection trait designed to temporarily close exposed dentinal tubules.
The additional use of 10% povidone-iodine for irrigation confers no supplementary benefit to treatment success, which may not be surprising given that iodine and sodium hypochlorite are both halogen-releasing agents, acting on common protein groups (McDonnell & Russell, 1999). The alternative agent, chlorhexidine had originally been justified on grounds of its substantivity in root dentine (Rosenthal et al., 2004), relative lack of toxicity (Loe, 1973) and broad-spectrum efficacy (McDonnell & Russell, 1999). However, 2% chlorhexidine irrigant has been shown to be less effective than 1% NaOCl in reducing bacterial load to undetectable levels (70% vs. 80% negative load, respectively) (Zandi et al., 2016), although there was no difference in periapical healing at 4-years (81% vs. 82%, respectively) (Zandi et al., 2019). In another study, the additional use of 0.2% chlorhexidine irrigant, surprisingly, reduced the success of treatment significantly (Ng et al., 2011a, 2011b). The use of chlorhexidine is currently deprecated for the toxic interaction product (para-chloro-aniline) from its reaction with sodium hypochlorite, which is deemed cytotoxic and carcinogenic (Basrani et al., 2007; Bui et al., 2008). Apart from mutually depleting the antibacterial moiety of both solutions, the precipitate may potentially irritate periapical tissues and block dentinal tubules or accessory anatomy, particularly the apical infected anatomy. Chlorhexidine has also been associated with two types of immune sensitivity reactions (Rose et al., 2019; Teixeira de Abreu et al., 2017) and coupled with the other issues is now not widely advocated for root canal irrigation, despite its continued promulgation.
The physical aspect of irrigation dynamics has taken on a significantly more important conceptual dimension in root canal disinfection over the last two decades (Gulabivala et al., 2010) and its beneficial effects have been repeatedly demonstrated in in vitro studies. However, there is a paucity of clinical research evidence to underpin its intuitively obvious advocacy for improved periapical healing (Liang et al., 2013). The latter study failed to confirm a significant influence of ultrasonically agitated NaOCl irrigant on periapical healing. The lack of direct effect on periapical healing may simply reflect the fact that although such agitation may have a robust effect on the flow and mixing of irrigants in the part of the canal system above the stagnation zone (Gulabivala et al., 2010), its effect within the stagnation zone and therefore the encapsulated apical anatomy, where the critical infection remains, is probably negligible (de Gregorio et al., 2010). The novel multi-sonic device, GentleWave system (Sonendo, Inc.) displayed the promising outcome of 92% healed rate but critical evaluation of the data showed that only 19% of the teeth had necrotic pulps and the outcome was not stratified by periapical status (Sigurdsson et al., 2016). A further study on teeth with periapical lesions of sizes larger than PAI > 3, managed with the device protocol, showed complete healing in 82% after 12 months (Sigurdsson et al., 2018), which is on par with other approaches.
The lack of any obviously significant difference in periapical healing between chemical agents of different types and different concentrations is best explained by the physical and chemical stagnation caused by the apical stagnation zone phenomenon. Fluid in the stagnation zone lacks flow due to the closed-end-tube effect of the canal and its small volume, confining the chemical exchange to diffusion, which is an extremely slow and inefficient process (Gulabivala et al., 2010). The vapour lock effect, in addition may prevent adequate contact between the irrigant and canal contents. It is therefore hardly surprising that chemical irrigants with different antibacterial potencies, may show commensurate bacterial load reduction in the coronal two-thirds of the canal (sample-able part of the canal system), but regardless of their potency, all of them are “neutralized by the buffer” of the stagnant fluid zone containing the apical infected anatomy (Nair et al., 2005; Vera et al., 2012). This explains the voluminous laboratory literature on root canal system debridement, which universally show a lack of proper “cleaning” in the apical third of root canal systems (Gulabivala et al., 2010), as well as the consequent lack of influence on periapical healing (Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008).
Effect of number of treatment visits and interappointment medicaments
As already established, the performance of pulpectomy in the absence of apical periodontitis has very different disinfection requirements from those with established root canal infection and apical periodontitis. In the former teeth, maintenance of asepsis is the prime requirement, whilst facilitating residual pulp tissue removal using sodium hypochlorite, which may be enhanced by calcium hydroxide dressing, where judged necessary, due to its tissue denaturation properties (Hasselgren et al., 1988). In the latter teeth, even rigorous disinfectant irrigation is not completely effective in eliminating all the adherent bacterial biofilm (Nair et al., 2005), leaving residual bacteria to multiply and recolonize the canal system (Byström, 1986; Bystrom & Sundqvist, 1985). It is therefore desirable to supplement chemo-mechanical debridement at the end of the first visit with inter-appointment medication of the canal system using an agent capable of destroying or incapacitating residual bacteria and denaturing residual toxins and tissues; such an agent should ideally have a long-lasting effect that would be sustained over the entire inter-appointment period to prevent bacterial regrowth. The long-lasting effect may be a function of either sustained high concentration or a slow-release device or mechanism that acts as a buffer, allowing reversal of a chemical equilibrium reaction. The multi-visit approach also allows a second or further opportunity for chemo-mechanical debridement and a chance to gauge the early periapical host response through the presence/absence of exudate or pus, before placing the root filling.
There is a paucity of studies investigating the influence of inter-appointment medicaments on treatment outcome. The use of a variety of root canal medicaments in outcome studies, without proper segregation of their use or effect, precludes definitive conclusions to be drawn about them. The traditionally tested medicaments include calcium hydroxide, creosote, and iodine solutions (Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008), whilst more recent agents include 2% chlorhexidine gel alone or mixed with calcium hydroxide, and triple antibiotic pastes but they lack long-term clinical outcome data.
Calcium hydroxide, with its unique combination of properties, including antibacterial effect, tissue/toxin denaturation, and low aqueous solubility product (conferring a continuous-release capability and lasting effect), has enabled it to serve as an inter-appointment medicament for many years with predictable outcomes (Best et al., 2021; Kandemir Demirci et al., 2020; Ng et al., 2011a, 2011b). However, its antibacterial ability has come under close scrutiny, with opponents suggesting that the material is not suitable for purpose (Sathorn et al., 2007). Although a final and definitive resolution to this debate maybe yet to arrive, the current evidence unfortunately divides the discipline into proponents and antagonists of the agent, the authors firmly taking the former side.
A mixture of calcium hydroxide and chlorhexidine has been proposed based on the speculation of greater effectiveness against E. faecalis (Basrani et al., 2003; Gomes et al., 2003; Schafer & Bossmann, 2005). Such targeting of this species is unwarranted based on available evidence. Nevertheless, clinical trials have revealed no differences in efficacy amongst several tested: Ca(OH)2, 2% chlorhexidine gel, mixture of Ca(OH)2 plus 2% chlorhexidine gel, or triple antibiotic paste (Arruda et al., 2018; Manzur et al., 2007).
Equally, advocates of single-visit treatment remain despite the definitive evidence of residual viable bacteria in the root canal system after chemo-mechanical debridement. In teeth lacking apical root canal infection and apical pathosis, the case for single-visit treatment is strong as it should better serve to prevent bacterial contamination. In teeth with preoperative apical pathosis, the biological rationale for single-visit treatment is less clear and the debate about the merits and demerits of single versus multiple visit treatments remains an on-going controversy. The debate is fueled by considerations of cost-effectiveness (Schwendicke & Gostemeyer, 2016), practical-sense, business-sense, postoperative pain (Nunes et al., 2021) and biological rationale (Spangberg, 2001). Randomized controlled trials (Fonzar et al., 2017; Gesi et al., 2006; Molander et al., 2007; Paredes-Vieyra & Enriquez, 2012; Penesis et al., 2008; Peters & Wesselink, 2002; Trope et al., 1999; Weiger et al., 2000; Wong et al., 2015) on the issue have found no significant influence attributable to number of visits but they all lack statistical power and are compromised by potential bias related to recruitment and management protocols for cases not completed within the designated number of visits (Figini et al., 2007, 2008; Manfredi et al., 2016; Sathorn et al., 2005; Su et al., 2011). The debate on the merits of single versus multiple visit treatments will continue unabated given the respective strengths and nature of the motivational drivers amongst the opposing advocates. The issue may only be resolved by properly documented, large randomized controlled trials because unrecorded confounders (operator skill, biological or technical case complexity, patient compliance and recruitment bias) would continue to play out their biasing effect in non-randomized studies.
Effect of quality control of root canal disinfection and persistent bacteria
The focal infection era spawned the technique of quality-checking bacterial disinfection using an inter-appointment culture test prior to root-filling; the measure served a historic purpose in returning credibility to root canal treatment at the time. Obturation would only be embarked on if a negative culture test result was returned, “confirming” the absence of bacteria in the (sample-able part of the) root canal system (Buchbinder & Wald, 1939; Frostell, 1963; Morse & Yates, 1941). Over time, the perceived predictability and favourable prognosis of root canal treatment without microbiological sampling was realized and this quality control practice fell out of clinical favour because of its perceived deficiencies (time-consuming nature, difficulty, inaccuracy, laboratory-support-resource-rich) coupled with concerns over cost-effectiveness and business imperative (Molander et al., 1996a, 1996b). Despite the perceived deficiencies, a preobturation negative culture result increased periapical healing success twofold (Figure 4). One study (Seltzer et al., 1963) showing a 10% higher success rate when a negative culture test was returned in the presence of periapical disease, nevertheless, may have contributed to the beginning of the demise of the culture test. Demonstration of the predictability of bacterial load reduction with various chemo-mechanical strategies (Bystrom et al., 1985; Bystrom & Sundqvist, 1981, 1983, 1985; Sjogren & Sundqvist, 1987) may have consolidated its fate as a routine measure.
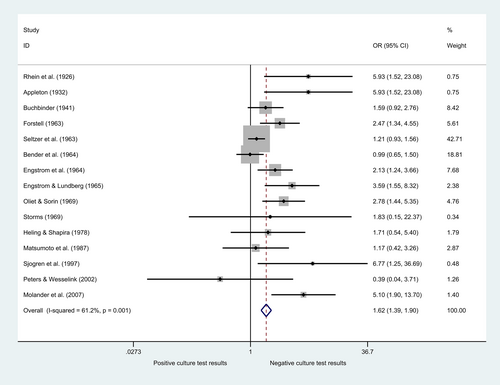
The effect of different stages and steps of root canal treatment (mechanical preparation, irrigation, medication) on the intra-radicular microbiota have been evaluated in numerous studies (Akpata, 1976; Auerbach, 1953; Bence et al., 1973; Bystrom et al., 1985; Bystrom & Sundqvist, 1981, 1983, 1985; Card et al., 2002; Chu et al., 2006; Cvek et al., 1976; Dalton et al., 1998; Engström, 1964; Gomes et al., 1996; Grahnen & Krasse, 1963; Ingle & Zeldow, 1958; Koontongkaew et al., 1988; Kvist et al., 2004; Lana et al., 2001; Markvart et al., 2013; Molander et al., 1990; Nicholls, 1962; Orstavik et al., 1991; Paquette et al., 2007; Peciuliene et al., 2000, 2001; Peters et al., 2002; Reit et al., 1999; Reit & Dahlen, 1988; Shuping et al., 2000; Siqueira, Guimaraes-Pinto, & Rocas, 2007; Siqueira, Magalhaes, & Rocas, 2007; Sjogren et al., 1991, 1997; Sjogren & Sundqvist, 1987; Stewart et al., 1961; Vianna et al., 2007; Wang et al., 2007; Xavier et al., 2013; Yared & Dagher, 1994), and a systematic review (Siqueira & Rocas, 2008), both qualitatively and quantitatively. Some studies merely reported the presence or the absence of bacteria, whereas others identified and quantified intra-radicular microbiota before and after the designated stages of treatment.
The effect of the steps upto and including “mechanical preparation” of the canal(s) on the microbiota has been tested using “neutral” irrigants such as water or saline; such studies show that negative cultures were achieved in 31% (range 0%–79%) (weighted pooled average) of the cases. The use of sodium hypochlorite (concentration range 0.5%–5.0%) irrigation during the steps upto and including ‘mechanical preparation’, increased the frequency of negative cultures immediately after debridement to 52% (range 13%–95%) (weighted pooled average) (Gulabivala & Ng, 2019a, 2019b).
Despite such microbial reduction, the majority of studies report culture-reversals during the inter-appointment period if antibacterial dressing was avoided. Culture reversals may be attributed to either regrowth of residual bacteria because of inadequate chemo-mechanical debridement or recontamination by bacterial leakage, from restorative margins or tooth cracks. It is important to diagnostically distinguish between the two causes because the former may be correctible, and the latter potentially may not be. The currently deprecated cotton wool dressing underneath the access restoration serves as a useful diagnostic aid for leakage into the tooth by sign-posting the location and extent of staining (Gulabivala & Ng, 2014), whereas other alternatives (Sattar et al., 2017) are not as useful in this context. The use of inter-appointment, antibacterial intra-canal dressings, increased the frequency of negative cultures at the subsequent visit to an average of 71% (range 25%–100%) (weighted pooled average) of cases (Gulabivala & Ng, 2019a, 2019b).
Bacterial taxa recovered from preobturation cultures include Enterococcus, Streptococcus, Staphylococcus, Lactobacillus, Veillonella, Pseudomonas, Fusobacterium species and yeasts. Some studies attribute statistical associations between the presence of individual species and treatment failure. As an example, one study noted an overall failure rate of 31% in cases with positive cultures, 55% for teeth with Enterococcus species and 90% for teeth with Streptococcus species (Frostell, 1963). Another study with good quality root canal treatment on 54 teeth with asymptomatic apical periodontitis and an overall success rate of 74%, attributed 80% success in the absence of bacteria, 33% for those with detected canal bacteria before obturation and 66% for those with Enterococcus faecalis (Sundqvist et al., 1998). It is stressed that these are merely associations and not cause–effect relationships; a fuller picture may only emerge by exploring the full interaction between the total microbial diversity and other treatment outcome factors.
An interpretive perspective is added to these clinical-microbiological findings from a controlled experimental monkey-model study (Fabricius et al., 2006), involving infection of monkey's teeth with four- or five-strain bacterial microcosms to test the effect of debridement and obturation on periapical healing outcome. They found that of the canals with residual bacteria following chemo-mechanical debridement, 79% were associated with periapical non-healing, compared with only 28%, when no bacteria remained. Multiple residual species were more frequently associated with non-healing than single species survival. Absence of bacteria after chemo-mechanical debridement was associated with periapical healing, independent of root-filling quality but bacterial persistence was correlated to a greater degree with non-healing in the presence of poor-quality root-fillings than with technically well-performed root-fillings. Furthermore, when bacteria were detected after root-filling removal, 97% showed absence of periapical healing, compared with only 18% when bacteria were not detected. The study re-emphasized that optimal periapical healing conditions are achieved by reducing bacteria below detection limits before permanent root-filling and that obturation played an important role in helping to control residual infection.
Regardless of the sampling technique, the use of a negative culture result to inform progress of treatment has a positive impact on treatment outcome. More recently, alternative bacterial tests, such as, fluorescent vital dye has been tested for use as a rapid chair-side root canal microbial detection method to predict periapical healing with promising results (Knight et al., 2020). The evidence shows the value of such a quality-control measure to return root canal treatment to a biological fold.
Effect of acute exacerbation during treatment
Any invasive operative procedure is liable to elicit some pain or discomfort by virtue of its inherent injurious impact triggering an acute inflammatory response that may be superimposed on any pre-existing inflammatory or prevailing immune response. If the pre-existing pain is severe, treatment should not make it substantially worse through the inflammatory process alone but may do so through initiation of sensitization and neuropathy by lowering of neural firing thresholds or broadening of the field of involvement (Nixdorf et al., 2010, 2015). However, when preoperative pain is absent, mild or moderate, treatment may induce or make the pain worse for 24–48 h (Torabinejad et al., 1994); this is normal and patients should be fore-warned and fore-armed, psychologically and if necessary, pharmaceutically. In rare situations, the trajectory of pain may worsen over the following days, and this may be due to adverse alterations in the microbiota, immune reaction or neuropathic sensitization. The precise aetio-pathogenesis of such inter-appointment pain is ill-defined but could be triggered by chemical, mechanical, thermal or microbial injury to the periradicular tissues, conditioned by psychological (Seltzer & Naidorf, 1985a, 1985b) or neurological influences (Nosrat et al., 2020). Although such pain did not have a significant association with periapical healing in two studies (Kerekes & Tronstad, 1979; Sjogren et al., 1990), the London Eastman study (Ng et al., 2011a, 2011b) found that pain or swelling occurring in 15% of cases after chemo-mechanical debridement, was significantly associated with reduced probability of periapical healing. The speculative explanations may reside in incomplete chemo-mechanical debridement (either due to poor protocol compliance or greater microbial diversity) leading to a shift in canal microbial ecology favouring the growth of more virulent micro-organisms or extrusion of contaminated material during canal preparation or obturation, resulting in an acute or chronic foreign body reaction or (transient) extra-radicular infection (Siqueira, 2003).
Effect of root filling material and technique
Notwithstanding the observations on residual microbial presence in the root canal system and its relationship with obturation or root-fillings, investigation of the individual effects of obturation technique and root-filling material on treatment outcome is complicated by the inter-action between core root-filling material, sealer and placement technique. The most commonly used core root-filling material in the majority of outcomes studies was gutta-percha with various types of sealer or gutta-percha softened in chloroform (chloropercha) (Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008). The sealer types may be classified into zinc oxide eugenol-based, glass ionomer-based or resin-based (Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008). Recently introduced materials such as Resilon®, SmartSeal®, Mineral Trioxide Aggregate (Pace et al., 2014; Ree & Schwartz, 2017; Simon et al., 2007), silicate-based (Bardini et al., 2020) and bioceramic-based (Chybowski et al., 2018) materials have not penetrated clinical practice sufficiently to yield significant long-term data. The healing rate of teeth obturated with Resilon® (Resilon Research LLC) and Epiphany sealer (Pentron Clinical Technologies) was reportedly comparable with conventional gutta-percha/sealer in 1–2-year follow-ups (Cotton et al., 2008) but 5-year follow-ups (Barborka et al., 2017; Strange et al., 2019) showed higher failure rates. Apart from this exception, root-filling material or placement technique, per se, have no significant influence on treatment outcome (Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008). The impact of root-filling material is surprisingly manifested much more profoundly in its apical extent in relation to canal terminus and radiographic quality of obturation.
Effect of apical extent of root filling
The apical extent of root-fillings in relation to the root apex, is one of the many intra-operative factors under the control of the operator and is one of the most frequently investigated factors, because it offers a readily and constantly available assessment measure in retrospective studies. It is often analysed categorically by division into three types of root-filling extensions: (1) more than 2 mm short of radiographic apex (short); (2) within 2 mm of the radiographic apex (flush); and (3) beyond the radiographic apex (long) (Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008). This measure has a significant influence on periapical healing rates, regardless of preoperative periapical status (Ng et al., 2011a, 2011b; Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008). “Flush” root-fillings are associated with the highest success rates (81%) and “long” root-fillings (extruded) the lowest (66%) (Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008).
Retrospective root canal treatment outcome studies fail to distinguish between the effects of apical extent of instrumentation and apical extent of obturation because the former information is generally missing. The prospective Eastman study (Ng et al., 2011a, 2011b), measured both these parameters and found them to affect periapical healing, independently and significantly. This is consistent with the observations already made about obtaining patency to the canal terminus and accuracy of length determination and its maintenance. The length measures of canal preparation and root-filling extension naturally correlate with each other because canals are normally filled to the prepared canal length. The single measure “apical extent of root filling”, therefore informs about both the apical extent of canal cleaning and obturation. The exceptions were overextended instrumentation or extruded cleaning agents without root filling extrusion, or extruded root filling material without apical over-extension during preparation.
The issue of apical extrusion of root-filling sealer surprisingly divides the discipline between polar opposite views, despite the extremely clear and one-sided outcome data. Some endodontists pursue extrusion of “sealer puffs” through the main apical foramina and lateral/accessory canals as a “school of thought”, in the belief of its value as “good practice” (Nguyen, 1994). Their argument centres on the belief that sealer extrusion is only possible in the presence of thorough apical debridement and is taken as a measure of apical debridement quality and they therefore anticipate healing would follow predictably, albeit with some delay.
The collective outcome data are categorically clear, however, that extrusion of root filling material (gutta-percha) hinders, delays or prevents periapical healing (Ng et al., 2011a, 2011b; Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008). The biological mechanisms of action are persistent inflammation and foreign body reaction (Koppang et al., 1992; Nair et al., 1990; Sjogren et al., 1995; Yusuf, 1982). Gutta-percha may be contaminated by magnesium and silicon particles from the talc used in their manufacture (at least historically) and can induce a foreign body reaction (Nair et al., 1990). Experimental implantation of large pieces of gutta-percha subcutaneously in guinea pigs were encapsulated in collagen, whilst fine particles of gutta-percha induced an intense, localized tissue response (Sjogren et al., 1995). Clinical data do not show an exactly parallel effect on periapical healing based on extent of extrusion (Ng et al., 2011a, 2011b; Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008) but they have the additional problem of potential bacterial contamination of the extruded gutta-percha, although this hypothesis is unproven.
The data on periapical sealer extrusion draws contradictory conclusions. Extrusion of a glass ionomer-based sealer significantly reduced periapical healing rates (Friedman et al., 1995), whilst a zinc oxide eugenol based-sealer showed no significant effect, although only a quarter of the cases had exhibited extrusion (Ng et al., 2011a, 2011b). The discrepancy may be attributed to the differences in sealer type and duration of treatment follow-up. Radiographic assessment of sealer resorption may be complicated by the radiolucency of its toxic components and the insufficient sensitivity of radiographic methods to detect trace amounts (Ng et al., 2011a, 2011b). Radiographic disappearance of extruded sealer is clearly due to disintegration or dispersal of the radio-opaque component (barium sulphate) but this may be independent of the sealer constituent eliciting a host reaction that may still be resident in the vicinity (Nair et al., 1990).
Some extruded sealers, glass ionomer-based (Friedman et al., 1995), zinc oxide eugenol-based (Huumonen et al., 2003), silicone-based (Huumonen et al., 2003), and Endomethasone® (Boggia, 1983), remained in the periapical tissues after 1 year. Whilst traces of a calcium hydroxide-based sealer (Sealapex®) could be detected after 3 years (Sari & Okte, 2008). Longer term studies show more complete resorption of extruded sealer over time, for example, 69% of zinc-oxide eugenol-based sealer after 4 years (Procosol®, Roth Elite®) (Augsburger & Peters, 1990), and 45%–85% of resin-based sealer after 4–10 years (AH Plus, Dentsply/DeTrey) (Goldberg et al., 2020; Ricucci et al., 2016; Sari & Okte, 2008). Conversely, extruded sealer has been known to persist even after 10 years in 40% of cases (Goldberg et al., 2020). Ng et al. (2011a, 2011b) advanced two explanations for the difference between the effect of extruded core gutta-percha and zinc oxide/eugenol sealer; the antibacterial properties of the latter may help to control residual microorganisms, whilst it is also more soluble and readily removed by host cells compared with gutta-percha.
The overwhelmingly clear conclusion must be that the penetration of a chemically active foreign material, devoid of regenerative potential, into a wound, infected or uninfected, would hardly enhance healing and is more likely to delay or prevent healing. It is best to avoid extrusion of root filling materials of any type to obtain the best periapical healing outcomes. The notion of using bio-inductive materials that may support periapical healing is yet to be proven.
Effect of root-filling quality
Another one of the widely investigated parameters of root canal treatment has been the radiographic measure of “root filling quality”; once again because of its ready, constant and un-degraded availability in retrospective studies. “Root-filling quality” describes the radiographic perception of its “completeness” in extending to the apical and lateral boundary walls of the canal system without voids or extrusion. The stated rationale for complete obturation of the root canal system is to prevent bacterial re-contamination from residual canal infection or new infection from coronal, apical or lateral portals. Both residual or new microbial invaders may be prevented from recolonizing the root canal system by a “tight” seal with the canal wall and an absence of voids within the body of the material. “Root-filling quality” may be taken as a surrogate measure for quality of execution of the root-filling technique or even more broadly, quality of execution of the entire root canal treatment procedure, as discussed before on quality control of disinfection. Also, good quality obturation is reliant on properly executed preliminary steps in canal preparation. A systematic review (Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008) reported that the criteria for judging the quality of root fillings remain poorly defined (de Chevigny et al., 2008a, 2008b; Hoskinson et al., 2002; Sjogren et al., 1990), with the use of vague phrases such as “unsatisfactory root-filling”, “inadequate seal”, “poor apical seal” or “radiographic presence of voids”. The main problem, however, is that it is an attempt to grade the three-dimensional relationship between root-filling material and the canal system, using a two-dimensional detection method lacking adequate sensitivity. Despite the severe inadequacies in the two-dimensional approach for judging root-filling quality, the measure “satisfactory root-filling” is nevertheless consistently associated with significantly higher success rates than “unsatisfactory root-fillings” (Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008) even with CBCT (Fernandez et al., 2017; Liang et al., 2011), reflecting its powerful impact.
Post root canal treatment factors
Effect of quality and type of restoration
The quality and type of coronal restoration after root filling has a major impact on the probability of periapical healing. Teeth with “satisfactory” coronal restorations exhibit three-fold better periapical healing rates compared with those with “unsatisfactory” restorations (Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008). This is another one of the startling observations as it seems to compete with the presence of apical pathosis as a major influence, suggesting a connection with microbiota ingress or their reactivation. Definition of the term “satisfactory” restoration varies in detail from study to study, for example: (1) no evidence of marginal discrepancy; (2) no evidence of marginal discoloration; (3) no evidence of recurrent caries; and (4) absence of a history of restoration decementation (Hoskinson et al., 2002; Ricucci et al., 2011).
Furthermore, the criteria for “unsatisfactory restorations” (Hoskinson et al., 2002; Ricucci et al., 2011) do not account for the presence or the absence of an intact inner restorative core. To obviate this problem, the London Eastman study (Ng et al., 2011a, 2011b) adopted the following more severe definition for unsatisfactory restorations: (1) obvious signs of exposed root filling; and (2) potential leakage indicated by marginal defects and history of de-cementation. Applying these standards, the study revealed an extremely profound effect (Odds Ratio = 10.7; 95% CI: 3.7, 31.5) of restorative status on the probability of periapical healing.
Other studies made different comparisons of restorative status, such as permanent versus temporary restorations (de Chevigny et al., 2008a, 2008b; Friedman et al., 1995; Ng et al., 2011a, 2011b); crown versus plastic restorations (de Chevigny et al., 2008a, 2008b; Friedman et al., 1995; Ng et al., 2011a, 2011b; Sjogren et al., 1990); presence versus absence of posts (Friedman et al., 1995; Ng et al., 2011a, 2011b); and non-abutment versus abutment teeth (Ng et al., 2011a, 2011b; Sjogren et al., 1990). Permanently restored teeth were associated with significantly higher periapical healing rates than their temporarily restored counterparts (de Chevigny et al., 2008a, 2008b; Friedman et al., 1995) but not always (Chugal et al., 2007; Ng et al., 2011a, 2011b). The type of permanent restoration (de Chevigny et al., 2008a, 2008b; Friedman et al., 1995; Ng et al., 2011a, 2011b; Sjogren et al., 1990) had no significant influence on periapical healing.
Provision of a sub-seal over the root filling to avert the impact of future coronal restoration leakage seems wise, should the restoration margin fail, or the restoration be lost altogether. Materials used for such sub-sealing include glass ionomer (GIC) or zinc oxide eugenol cement (Saunders & Saunders, 1994) but have not been found to confer any additional benefit on treatment success (Kumar et al., 2020; Ng et al., 2011a, 2011b) because in both studies, the primary seal was not breached. In summary, the provision of a good quality coronal restoration, regardless of type, should be considered an important and final part of root canal treatment and has a profound influence on periapical healing.
Effect of imposed functional occlusal stresses on root-treated teeth
The stresses imposed on root-treated teeth are a function, first, of the manner in which the patient uses them, and secondly, their functional prominence in the occlusal scheme. The pattern of static and dynamic occlusal loading stresses in teeth is dictated by holding or guiding contacts, as well as their status as single units or abutments (bridge/denture). Prosthetic abutments (fixed or removable) may bear more unfavourable loads, as may last-standing teeth in the dental arch (Matsumoto & Goto, 1970). Evidence suggests such teeth exhibit lower periapical healing rates, presumably through development of cracks and fractures due to fatigue (Walton, 2002, 2003), or a greater propensity for restorative margin failure.
In conclusion, the prominent impact of restorative factors on periapical healing is highly suggestive of the importance of tooth integrity as well as the restoration/margin integrity, whatever, the precise definition of that statement might prove to be in the future. At present, the understanding of the nature of this phenomenon remains neophytic and is classed merely as “microleakage” or “nanoleakage”.
OUTCOME OF NON-SURGICAL ROOT CANAL RETREATMENT
Root canal retreatment (or secondary root canal treatment) is conducted when primary root canal treatment fails to resolve periapical disease and sub-standard features of the previously executed procedure can be identified for improvement. Consequently, all factors affecting primary root canal treatment are liable to influence the outcome of secondary root canal treatment, plus any unresolved biological problems, as well as new iatrogenic issues introduced by the primary treatment attempt. Such features may include deficiencies in access cavities, location and negotiation of the entire anatomy (radiographic), insight about the robustness and diligence in the primary chemomechanical debridement (history), or root-filling quality (radiographic).
Procedurally, root canal retreatment requires removal of any obstructing restorative materials plus previous root filling material to re-access the entire root canal system, particularly to obtain patency to the contaminated apical anatomy. Ideally, all of this should be achieved without any dentine removal either coronally or intra-radicularly. Having completed this phase, the accessible root canal anatomy should be re-examined and re-gauged to determine its prepared dimensions. At this stage, the canal system may be re-assessed for missed anatomy or corrected for any iatrogenic procedural errors, including blockages and finally, its shape may be modified into a more optimal form to facilitate better irrigation and re-obturation. The periapical healing rates of root canal retreatment are slightly lower compared with primary treatment. This is attributed to persistently obstructed access to the apical infection; and/or potentially more resistant microbiota, which the host immunity is unable to overcome.
The mean weighted probability of complete periapical healing is 69%, about 6% lower than in the case of primary treatment on teeth with apical periodontitis (Ng et al., 2011a, 2011b; Ng, Mann, & Gulabivala, 2008; Ng, Mann, Rahbaran, et al., 2008).
The factors influencing outcomes of periapical health after root canal retreatment are identical to those affecting primary root canal treatment, except for elements peculiar to secondary root canal treatment as mentioned above. Hence, a separate treatment of the data is unnecessary. Of the potential prognostic factors unique to retreatment cases, the main one showing significant influence on outcome after treatment was the ability to remove or bypass pre-existing root filling material or separated instruments during retreatment to achieve canal patency at the terminus (Ng et al., 2011a, 2011b).
CONCLUDING REMARKS
The complex picture of factors influencing the outcomes of root canal (re)treatment ultimately distils down to a very simple principle, which explains all the apparently surprising findings.
The net effect of all the various root canal treatment protocols ever used has been the same, to enable control of infection in the instrumented root canals. The single most important intra-operative factor is the proximity to the canal terminus of apical extent of debridement and the apical extent of root-filling (without periapical extrusion). Extrusion of root filling material consistently delays or prevents periapical healing. However effective the protocol is in exerting control over the microbiota within the instrumented parts of the root canal system, the complex apical anatomy remains infected (Nair et al., 2005). Interaction between this residual apical infection and host defences (original cause of apical periodontitis) continues beyond the completion of the root canal treatment procedure, but with an altered dynamic in all healing cases. Matsumiya and Kitamura (1960) correctly judged that root canal treatment induced sufficient bacterial control in the instrumented part of the root canal system to dampen apical inflammation without completely switching it off. This is because of the residual bacteria in the apical anatomy, which do however, progressively become inactive or die because their nutritional source, the inflammatory exudate, reduces in concert with the dying bacteria. Completion of active root canal treatment (or sometimes chemo-mechanical debridement) marks the beginning of a new phase in the dynamic apical encounter, in which the apical immune mechanisms gradually re-exert control over the surviving intra-radicular apical infection. The precise dynamic (Nair, 1997) may vary from tooth to tooth, and host to host, dependent on the relative strength of the two arms (infection versus host defences) of the interaction, resulting in the typically variable but nearly-always extended periapical healing period (1–4 years plus).
The rates of periapical healing over the previous century show no significant differences because the principles of root canal treatment had remained the same over that period, despite conceptual and protocol variations. Whilst the protocol changes have improved the efficiency and predictability of the technical outcome, they have not altered the efficacy of periapical healing. This is perfectly logical because none of the root canal treatment protocols over the last century have altered the nature of the intra-operative or postoperative apical host/microbial dynamic. It should therefore not be expected that the biological outcomes would be any different by chronological (decade of treatment) or geographic (location in the world) distribution.
All the factors that have a direct effect on the apical host/microbial dynamic have a powerful prognostic effect on periapical healing (preoperative periapical status including signs and symptoms of infection and size of lesion, patency to canal terminus, apical extent of canal instrumentation and root-filling, quality of restoration and remaining tooth structure). Whilst all the factors that have no or only an indirect influence on the apical host-microbial dynamic exert no or only a weak prognostic effect on periapical healing (age, sex, general health, tooth type, rubber dam use, magnification and illumination use, access cavity design, root canal instrumentation choice and technique, dimensions of canal preparation, root canal irrigation choice and technique, root filling material choice and technique). Effective apical root canal irrigation and medication can have an impact on the apical dynamic (Vera et al., 2012), as may the genetic expression of host immunity, and are yet likely to emerge as important influencing contenders in future studies.
Root canal treatment may be summarized as the management of pulpal or periapical infected wounds through the application of age-old surgical principles of wound management, debridement and dressing (obturation) to allow healing. Put simply, once the dynamic host/microbial interaction is established at the periapex, it is sustained across the pre-operative, intra-operative and postoperative phases of root canal treatment. Adequate root canal treatment “actively” shifts the ecological balance in favour of the host immune defences, dampening the inflammation and commencing a new phase in the interaction. Breaches in the tooth (cracks) or marginal integrity (leakage) may “passively” allow reversal of the targeted microbial demise and host interaction, hence the remarkably powerful impact of this factor on outcomes. This then is the reframed and re-stated principle of root canal treatment. It strongly and logically argues for a two-stage (two-visit) management of teeth with apical periodontitis, in which the debridement phase only is ideally completed within one visit.
Prognostication should therefore take account of the feasibility of both biological (periapical lesion size and symptoms) and technical (root canal system complexity and operator competency) control of the root canal infection, as well as the prospect of sustaining any root-canal-treatment-induced microbial control through tooth and restorative interface integrity. The endodontist must, therefore, also have insight about factors influencing tooth restoration and survival.
AUTHOR CONTRIBUTIONS
The two authors contributed equally to conception, data analysis, writing and critical appraisal.
CONFLICT OF INTEREST STATEMENT
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
ETHICAL APPROVAL
This investigation did not involve human or animal subjects.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.