Review of guidance for the selection of regenerative endodontics, apexogenesis, apexification, pulpotomy, and other endodontic treatments for immature permanent teeth
Abstract
This review guidance is a work in progress because the limitations of regenerative endodontics are still being discovered. The endodontic treatments for immature permanent teeth with a necrotic pulp can vary considerably among endodontic practitioners. Whereas, regenerative endodontic treatments are growing in popularity and are creating ever more complex treatment protocols, involving revascularization and/or autologous platelet-rich plasma and scaffolds to elicit host stem cell de novo tissue formation to reestablish the vitality of immature teeth for the purpose of continuing root maturation. Despite much evolving controversy about their potential benefits, risks, prognosis, and contraindications, this review is aimed to discuss how to ensure that regenerative endodontic treatments are successful, by strictly adhering to case selection criteria, and following precise steps to accomplish and monitor the success of the treatment. A review of the endodontic literature was performed, together with practical observations of the problems and outcomes of performing regenerative endodontic treatments. Traditionally, apexification has long been the treatment of choice provided to immature teeth with a necrotic pulp. Regenerative endodontics may be provided as an alternative to apexification, if the tooth and patient meet all the case selection criteria, and if there are no contraindications. Regenerative endodontics has the unique potential advantage of being able to continue the root development in immature permanent teeth, thereby potentially saving the teeth for the lifetime of the patient. Whereas, conventional endodontic root canal treatment, Cvek partial pulpotomy, apexogenesis, and apexification, should always be provided when these treatments are more likely to benefit the patient because they can be more successful than regenerative endodontics.
INTRODUCTION
Millions of young patients have their immature permanent teeth extracted every year, although most endodontists and paediatric dentists have personalized regenerative endodontic treatment strategies that are available to do almost everything possible to save these teeth (Murray et al., 2007). Regrettably, due to toothache, most patients opt to have a painful tooth extracted (Silva-Junior et al., 2017). Some patients do not apprehend the ability of endodontic treatments to alleviate the toothache, and save their natural teeth, which is preferable over the long term to maintain their quality of life and ability to chew food (Hugo et al., 2009). There is no dispute that dental implants, bridges, and dentures can be aesthetically and functionally valuable to replace missing teeth. But dental implants are a potential source of dental pain, discomfort, lack of tooth sensation, need for invasive bone surgeries, bleeding and peri-implantitis infection problems, risk of failures (Clark & Levin, 2019), and chewing limitations for patients, in addition to the risk of healing complications following tooth extractions (Lodi et al., 2021) cannot be overlooked because of the dentist's responsibility to provide treatments to patients based on an unbiased evidence base (Clark & Levin, 2019). Greater advocacy by endodontists and dental associations of their skills to save natural teeth, is needed to improve the uptake of endodontic treatments, to help counter the increasing trend towards teeth extraction, and the placement of expensive dental implants (Clark & Levin, 2019). Endodontic treatments can be as successful as dental implants. Especially when treatment planning uses a differential diagnosis of the health status of the patient, the status of root development, and the pulp status of the immature tooth, to determine which endodontic treatments are appropriate or inappropriate. Ultimately, the selection of the most appropriate treatment plan is the one key factor that is most likely to benefit the patient by providing them with the highest quality longest lasting endodontic care.
ENDODONTIC TREATMENT TO SAVE TRAUMATIZED AND DISEASED IMMATURE TEETH
Traumatic dental injuries occur frequently in children and young adults, 25% of school children and 33% of adults have experienced trauma to the permanent dentition, with most of the injuries occurring before 19 years of age (Levin et al., 2020). Adult patients who have conventional root canal treatments to save fully mature permanent teeth with an irreversibly injured pulp, diseased necrotic pulp, or accidentally exposed pulp, can benefit from a long-term success rate of over 86% (Elemam & Pretty, 2011). Nevertheless the opposite, a lack of success, can be true for immature permanent teeth following treatment. This is because of their fragile root physiology and anatomy, which creates more complex diagnostic and clinical challenges (Harlamb, 2016). Fragile immature teeth can have dentinal walls which are thin and weak, making them prone to a stress-overload fracture (Lawley et al., 2004). Thus, the success of regenerative endodontic treatment to save fragile immature teeth with a necrotic pulp can be dependent on the endodontists ability to adequately disinfect the root canals. In addition to bringing about the regeneration of replacement de novo pulp-like tissue by revascularization through the root apex, to revitalize the tooth for it to continue the mineralization and maturation of the root dentinal walls to strengthen the tooth root. Thereby making the root stronger to save the tooth by making it more resistant to a fracture.
Some endodontists may lack the training and experience to provide regenerative endodontic treatments. This is because some endodontists who were surveyed admitted they lack a sound knowledge of regenerative endodontics, and only one in five, had a positive perception of its usefulness (Mayya et al., 2021). Hence the need for this review, not only to focus on regenerative endodontics, but also to provide guidance on patient selection, case selection, and the status of root development, to guide the endodontist to use differential diagnosis criteria to select the most appropriate type of endodontic treatment plan for every type of immature tooth. The endodontic treatment options for immature permanent teeth, include regenerative endodontics, conventional non-surgical endodontic root canal treatment, Cvek partial pulpotomy, apexogenesis, and apexification.
A recent survey has shown that most endodontists are willing to obtain training to provide regenerative endodontics to patients (Mayya et al., 2021). However, placing the focus solely on regenerative endodontics as a gold standard can be a risky educational strategy. This is because it may lead some endodontists to incorrectly presuppose that because a tooth is immature, that regenerative endodontics must always be the correct and most beneficial treatment of choice for the patient's tooth. Regenerative endodontics is not always the best choice among all of the available endodontic treatments for traumatized or caries-affected immature teeth. This is because the clinical failure rates of regenerative endodontics to revitalize immature teeth can be as high as 40% (Murray, 2018; Wikström et al., 2022). Post-treatment painful and/or severe swelling flare ups can be observed in one-third of cases, and in almost half of cases, there was no apparent root development and apical closure (Meschi et al., 2021). In contrast, some clinical trials report tooth survival rates above 93% (Elfrink et al., 2021), and overall success rates above 80% for regenerative endodontic treatments (Chrepa et al., 2020). Not all the failures of regenerative endodontic treatments are the fault of the provider endodontist, but the large variations in the reports of success and failure rates, suggest that precise case selection criteria together with precise adherence to the steps to accomplish regenerative endodontics can be extremely important for the success of the treatments (AAE, 2016).
ENDODONTIC TERMINOLOGY FOR TREATMENTS FOR IMMATURE TEETH
It is essential that the endodontic treatment terminologies are defined to be able to communicate with colleagues using the same language. Unfortunately, the definitions can change slightly over time, as also usage between different authors, dental dictionaries, and professional associations. However, mostly the key elements of the endodontic treatment definitions for immature teeth are similar, as summarized here.
Some key terminologies for the endodontic treatments for immature teeth are:
Apexification—A necrotic pulp and irreversible pulpitis procedure which debrides, disinfects, and obturates the root canal of immature teeth. The obturation of the root canal with calcium hydroxide or mineral trioxide aggregate (MTA) will induce an apical calcified barrier to help save the tooth (Goldstein et al., 1999; Rafter, 2005; Shaik et al., 2021).
Apexogenesis—A vital pulp procedure which debrides the coronal injured pulp from the root canal of an immature permanent tooth. The removal of the superficial injured pulp will allow the remaining vital pulp to continue the maturation and physiological development of the roots (Goldstein et al., 1999; Mousivand et al., 2021).
Conventional non-surgical root canal treatment—A necrotic pulp and irreversible pulpitis procedure for mature teeth which uses instruments, irrigants, and chelating agents to debride infected tissues and disinfects the root canal by cleaning, shaping, sealing, and obturation (Metzger et al., 2010; Peters, 2004).
Cvek partial pulpotomy—A vital pulp procedure which debrides 2 mm of coronal injured pulp from a root canal. The removal of the superficial injured pulp will allow the remaining vital pulp to continue the maturation and physiological development of the roots (Mejàre & Cvek, 1993; Sari, 2002).
Irreversible pulpitis—Chronic inflammation of the dental pulp which cannot be reversed to heal the damaged tissues; thus, the prognosis is that the pulp will become necrotic (Ricucci et al., 2014).
Necrotic dental pulp—Death of the cells of the dental pulp (Yu & Abbott, 2007).
Pulp revascularization/revitalization—A necrotic pulp and irreversible pulpitis procedure which disinfects the root canal with antibiotics or/and antimicrobial agents. The periapical tissues are instrumented through the open root apical foramen to cause bleeding into the canal to revascularize it. Thereby, promoting tissue formation within the root canal for the continued deposition of mineral to strengthen dentine and grow the roots of immature teeth (do Couto et al., 2021; Namour & Theys, 2014; Wigler et al., 2013; Wikström et al., 2022).
Regenerative endodontics—A necrotic pulp and irreversible pulpitis procedure which debrides tissues from the root canal, disinfects the root canal, instruments the periapical tissues through the open root apical foramen to cause bleeding into the canal to revascularize it, as described above. In addition to adding a scaffold or biological procedure within the root canal to promote vital tissue formation which will continue the deposition of mineral to strengthen dentine and grow the roots of immature teeth (Chrepa et al., 2020; Elfrink et al., 2021; He et al., 2017; Meschi et al., 2021; Murray, 2018; Murray et al., 2007; Trope, 2008). The steps to accomplish regenerative endodontics are shown in Table 1.
| Patient care and consent |
| Ensure the patient satisfies the case section criteria for regenerative endodontics (Figure 1) and obtain patient approval, and parent and guardian consent for the treatment plan |
| Tooth selection for regenerative endodontics |
| The tooth must be permanent and very immature with a wide-open apical foramen wider than 1.1 mm and have an injured or exposed pulp. The tooth must have thin walls that will benefit from a continued development of the root, so that it can become stronger and less prone to failure in later life |
| Anaesthesia of the immature permanent tooth |
| Establish an anaesthetic block of the tooth using 3% Mepivacaine, without vasoconstrictors, one carpule will be needed every 20 min |
| Disinfection, irrigation, and instrumentation of the tissues within root canals |
| Isolate the tooth with a rubber dam and cut a root canal access wide enough to see all the walls |
| Irrigate the root canal with 20 ml of 1.25% NaOCl with suction to prevent leakage |
| Establish the root canal working length with a hand file and radiograph |
| Introduce a hand or rotary file into the root canal and avoid instrumenting the dentinal walls |
| Pack the root canals with calcium hydroxide or a triple antibiotic paste of Ciprofloxacin, Metronidazole, Minocycline to a final concentration of 0.1 mg/ml, for up to 4 weeks and restore the tooth with a temporary restoration |
| Irrigation, chelation, rinsing and drying root canals |
| Irrigate the root canal with 20 ml of 1.25% NaOCl with suction to prevent leakage |
| Rinse the root canals with a chelating agent of 17% EDTA or Qmiz2in1 for 60 s |
| Final rinse of root canal with sterile saline |
| Dry root canal with paper points |
| Revascularization and scaffolds inside root canals |
| Stir periapical tissue with a bent k-file 3 mm through the root apex to induce bleeding |
| If you wish to use a BCR approach, wait for blood to fill the root canals up to the level of the cementoenamel junction. If you wish to attempt to use PRP or PRF to revascularize the root canal, you should allow an extra 30 min to use phlebotomy to obtain the patient's own blood from a vein in their arm, and to centrifuge it using a PRP or PRF kit before placing the PRP or PRF into the root canal |
| Insert bioabsorbable collagen scaffolds using forceps' to lightly pack the root canal space from the apex to the cementoenamel junction |
| Restore tooth |
| Seal root canal orifice with a 2 mm thick layer of white MTA placed in contact with the scaffolds |
| Restore tooth with composite resin permanent restoration and check occlusion |
| Monitoring healing and recall of patient |
| Monitor tooth for flare ups and periapical tissues for healing and provide a retreatment if necessary |
| Recall patient every 6 months to check tooth for vitality and root development |
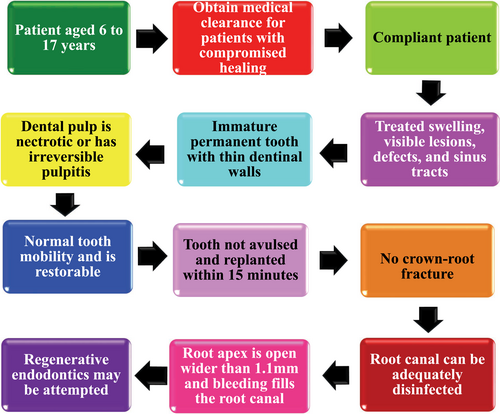
AN OVERVIEW OF THE CASE SELECTION CRITERIA FOR REGENERATIVE ENDODONTICS
The success of regenerative endodontic treatments also including pulp revascularization and revitalization, can vary widely, with a success rate of 60% (Wikström et al., 2022). This suggests the need to adhere to strict case selection criteria to ensure the optimal success of regenerative endodontic procedures can be accomplished. The case selection criteria may include.
Patients aged 6 to 17 years
Regenerative endodontic treatments are not recommended to be provided to deciduous (baby) teeth, due to the risk of retaining these teeth, and interfering with the eruption pattern of the permanent teeth. The youngest age that permanent teeth erupt is 6 years of age (Almonaitiene et al., 2012), thus because regenerative endodontics should only be provided to permanent teeth, the minimum age of patients is 6 years of age.
Regenerative endodontics have been provided to mature adult teeth in patients aged older than 17 years of age (He et al., 2017). However, when adult teeth have thick dentinal walls to withstand fracture, providing regenerative endodontics does not provide the adult patient with any reasonable potential benefits. This is because of the greater risk of failure, greater risk of complications, greater risk of a painful flareup, and greater risk that a retreatment will be necessary, due to the success rate being 60% (Murray, 2018; Wikström et al., 2022). In addition to the regenerative potential of adult mature teeth, being extremely limited (Trope, 2008), suggesting the ability for oral tissue regeneration decreases with patient age and maturity. Conventional non-surgical root canal treatment is the optimum treatment for mature adult permanent teeth, because of the greater long-term success rate of over 86% over 10 years (Elemam & Pretty, 2011) and lowest risk of complications, such as recurrent pain.
Obtain a medical clearance for patients with compromised healing
Successful regenerative endodontic treatment requires revascularization, which is the formation of a blood clot within the tooth (do Couto et al., 2021). Patients who suffer from any systemic disease such as haemophilia, and von Willebrand disease which can compromise blood clotting, or who take blood thinner medicaments (anticoagulants) are at a greater risk of uncontrolled bleeding (Weibert, 1992). Thus, it is not recommended to provoke uncontrolled bleeding in these patients, due to the risk of tissue damage and suffering due to blood loss. Furthermore, because regenerative endodontics also requires healing and dental pulp-like tissue formation (Trope, 2008), where a patient suffers from a systemic disease which inhibits healing, the treatment is more likely to fail and be compromised. When any doubt exists about a patient's compromised health status, medications, and suitability for regenerative endodontics, it is best practice to obtain a medical clearance from the patients' other healthcare providers to prove that the patient is healthy enough for treatment. If the patient's health status suggests that regenerative endodontics will have a poor prognosis for an immature permanent tooth with a necrotic pulp, then apexification can be provided as necessary.
Compliant patient
As few as 39.5% of paediatric patients are compliant with dental clinical follow-up visits (Gune & Katre, 2021). There is the potential for some patients who have begun multiple visit regenerative endodontic treatments, to cease attending visits to complete the final steps in the treatment plan, likely because the toothache was alleviated. Consequently, some patients have antibiotic paste in the root canals of their teeth to disinfect the root canals, without any obturation of the root canals and without a final restoration of the tooth to finish the course of treatment. In this incomplete treatment state, the tooth has a poor prognosis because it will not be able to regenerate, and still may have a lingering infection and necrotic pulp. To avoid the problem of patients failing to complete a course of regenerative endodontics, multiple visit treatments should only be provided to children who have a history of attending dental visits. If there is doubt about a patient's ability to comply with multiple treatment visit requirements, the endodontic treatment should be provided in a single visit, to ensure it can be completed.
Treated swelling, sinus track, and visible lesions
Where a patient has swelling, visible lesions, defects and sinus tracks associated with the root canal of an immature tooth, these must first be resolved, drained, disinfected, treated, and sealed to create a long-lasting hermetic barrier prior to regenerative endodontics, to prevent the microleakage of microorganisms into the root canal. This is because a failure to prevent microleakage and a failure to adequately disinfect the root canal will compromise healing and is likely to fail (Wikström et al., 2022). It is possible to provide a regenerative endodontic retreatment if any of these complications occur after the initial treatment, however it must be recognized that the outcomes may be unpredictable (Mohammadi et al., 2021). The size of periapical lesions may be reduced following regenerative endodontic treatment, but the periapical tissues are unlikely to be completely healed (Kandemir Demirci et al., 2020).
Immature permanent tooth with thin dentinal walls
The most fragile immature permanent teeth in the youngest patients aged 6–9 years with thin dentinal walls are the most likely to benefit from regenerative endodontic treatment (Wikström et al., 2022) because it can continue root development by thickening the dentinal walls, and thereby strengthen the teeth to withstand a stress overload fracture (Lawley et al., 2004). Consequently, there is no obvious benefit to providing regenerative endodontic treatment to teeth which already have thick enough dentinal walls to withstand a fracture. Thus, if the pulp is necrotic or has irreversible pulpitis likely to become necrotic, with thick dentinal walls, the most optimum treatment will be apexification (Goldstein et al., 1999; Rafter, 2005; Shaik et al., 2021), rather than regenerative endodontics.
Dental pulp is necrotic or has irreversible pulpitis
The goal of regenerative endodontic treatment is to debride necrotic and infected tissues from the root canal, disinfect the root canal, and to instrument the periapical tissues through the open root apical foramen to cause bleeding into the canal to revascularize it. Then, adding a scaffold or biological procedure within the root canal to promote vital tissue formation which will continue the deposition of mineral to strengthen dentine and grow the roots of immature teeth (Namour & Theys, 2014; Wigler et al., 2013; Wikström et al., 2022). Therefore, regenerative endodontic treatment is not needed for permanent immature teeth with a vital pulp which is not necrotic or does not suffer from irreversible pulpitis, and these teeth are more likely to benefit from treatment with apexogenesis (Goldstein et al., 1999; Mousivand et al., 2021).
Normal tooth mobility and is restorable/crown-root fracture
A traumatized tooth which is loose and has excessive mobility, and/or which is non-restorable due to the loss of a crown or has suffered crown-root fracture, has a poor prognosis, and cannot be saved using regenerative endodontics alone, the treatments suggested by the traumatology guidelines should be provided (Levin et al., 2020).
Tooth not avulsed and replanted within 15 min
It is frustrating for an endodontist or paediatric dentist have a child with an avulsed tooth make an emergency dental visit, to discover that the avulsed permanent tooth was not cleaned and immediately replanted. Avulsed primary teeth should never be replanted (Hammel & Fischel, 2019). Although many articles discuss the benefits of storage media for avulsed teeth, avulsed permanent teeth should not be kept extra-oral in storage media. Replanted avulsed permanent teeth can suffer from healing complications; periapical radiolucency, external root resorption, ankylosis, which can be minimized by immediately replanting the permanent teeth, especially within 15 min of avulsion (Cho et al., 2016).
Root canal apex is open wider than 1.1 mm and bleeding fills the root canal
Following regenerative endodontic treatment, 25% of the treatment failures were attributed to the absence of bleeding (Wikström et al., 2022), which can also be stated as a failure to accomplish adequate root canal revascularization. The flow of blood from the periapical tissues into the root canal, and to fill the root canal space is essential for revascularization (do Couto et al., 2021; Namour & Theys, 2014; Wigler et al., 2013; Wikström et al., 2022). This is because without an adequate supply of blood there can be no revascularization and no de novo replacement pulp-like tissue formation to revitalize an immature tooth, and to mineralize the dentinal walls and continue root development.
A closed apical foramen in mature teeth, provides very little blood supply to the pulp. Hence revascularization should not be performed when the apical foramen is closed or almost closed. Indeed, it has been demonstrated that the apical foramen must be wide open, and the wider the better to allow an adequate blood supply to revitalize tissues within the root canal. In a study of replanted human incisors, it was shown that an apical foramen width of more than 1.1 mm was needed for successful root canal revascularization (Kling et al., 1986). Some researchers have used K-files to enlarge the size of a closed apical foramen in mature adult teeth, but this instrumentation is risky if the file tip breaks within the periapical tissues. Furthermore, instrumentation of the apex is likely a redundant strategy. This is because if the apical foramen is almost closed, it is likely that the dentinal walls are reasonably thick and not likely to benefit from a dentinal thickening and tooth strengthening against fracture provided by a regenerative endodontic treatment.
Root canal can be adequately disinfected
When regenerative endodontic treatment has failed, 14% of the failures were attributed to a persistent infection (Wikström et al., 2022), which can also be stated as failure to adequately disinfect necrotic and infected tissues from the root canal. The disinfection of the root canals can be effectively accomplished by placing calcium hydroxide, or a broad-spectrum triple antibiotic paste containing of Ciprofloxacin, Metronidazole, Minocycline (do Couto et al., 2021; Windley III et al., 2005) to a final concentration of 0.1 mg/ml, placed inside the root canal for 1–4 weeks (AAE, 2016). Potentially necrotic and infected tissue is also irrigated from the root canal using 20 ml of 1.25% NaOCl using hand and rotary files, followed by a flush of 17% EDTA, and a rinse of saline. Clearly, if there are inaccessible infected and necrotic tissue remnants within the root canals, these are a potential source of infection, and if they cannot be removed, the root canal cannot be adequately disinfected. If the root canal cannot be adequately disinfected, then regenerative endodontics treatment will likely fail, and be observed as a flareup, with swelling lesion, abscess, and pain. Therefore, apexification should be provided to immature permanent teeth with a necrotic pulp if the root canal cannot be adequately disinfected.
Summary for case selection criteria to attempt regenerative endodontics
The case selection criteria are a work in progress because the limitations of regenerative endodontics are still being discovered. The case selection criteria for regenerative endodontics discussed above, are summarized in Figure 1.
DIFFERENTIAL DIAGNOSIS TO SELECT ENDODONTIC TREATMENTS FOR IMMATURE TEETH
The most suitable endodontic treatments for immature teeth will vary depending on the case selection criteria, the status of the dental pulp as vital or non-vital or having irreversible pulpitis with a poor prognosis for continued pulp vitality, and the developmental stage of maturity of the root canals. This is because immature teeth that are almost fully developed, with thick and strong dentinal walls are better able to resist tooth fracture. However, very immature teeth at an early stage of development, with thin and weak dentinal walls are more prone to fracture, and these fragile teeth would most benefit from regenerative endodontic treatment to continue dentinogenesis to strengthen the teeth. Thus, regenerative endodontic treatment is not always optimal for immature teeth, and differential diagnosis should be used to select the most appropriate treatment with the highest success rate between apexification, apexogenesis, conventional root canal treatment, Cvek partial pulpotomy, and regenerative endodontics (Figure 2).
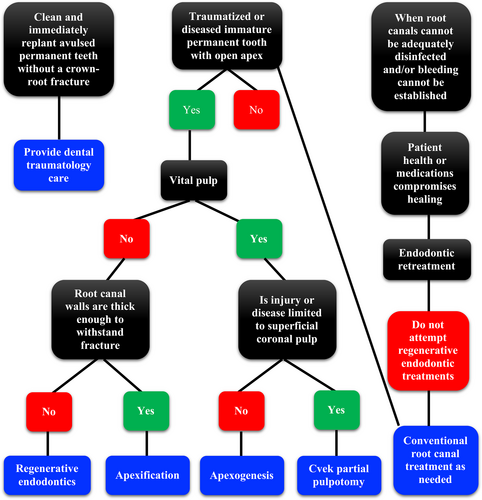
APEXIFICATION
The goal of an apexification is to debride the necrotic pulp from immature permanent teeth, to effectively disinfect the root canal, and to obturate the root canals with calcium hydroxide, MTA, or a bioceramic root repair material, to induce a calcified barrier to help save the tooth (Rafter, 2005; Shaik et al., 2021). A meta-analysis which compared MTA and Endosequence bioceramic root repair materials for apexification, revealed that all three of these biomaterials had similar success rates above 90% (Shaik et al., 2021), which is a 10% improvement, above the 80% reported success rate of calcium hydroxide for apexification (Damle et al., 2016). A drawback of using calcium hydroxide for apexification is that it requires multiple appointments to replace the calcium hydroxide, whereas the MTA need only be applied once (Guerrero et al., 2018). However, the practical limitations of apexification are that it cannot promote maturation of the immature tooth root, and thus cannot increase the thickness of the dentinal walls to strengthen the tooth. Therefore, apexification can be an optimal endodontic treatment for immature teeth with a necrotic pulp where the root dentinal walls are already thick enough to resist a fracture. Nevertheless, apexification is not an optimal endodontic treatment for fragile immature teeth with very thin dentinal roots, because it cannot mineralize the thickness of the dentinal roots to strengthen the tooth to resist a fracture.
APEXOGENESIS
Apexogenesis is a procedure which debrides the coronal injured pulp from the root canal of an immature permanent tooth with a vital pulp. The removal of the superficial injured and or infected pulp is necessary to prevent the spread of necrosis/infection/irreversible pulpitis to allow the remaining vital, uninfected, and uninflamed pulp to continue the maturation and physiological development of the roots (Goldstein et al., 1999; Mousivand et al., 2021). Apexification and apexogenesis are not comparable treatments for the same tooth. This is because unlike apexification discussed above, apexogenesis is a vital pulp-capping treatment, whereas apexification is a non-vital (necrotic pulp) treatment. Apexogenesis maintains the survival of the vital pulp to continue root maturation and thickening, which can strengthen the tooth to resist fracture. Thus, because the pulp is still vital and able to mineralize root dentine, there is also no rational justification for providing a regenerative endodontic treatment or a conventional root canal obturation treatment. The long-term success rate of apexogenesis in anterior teeth and posterior teeth was between 82.5% and 96.4% (Mousivand et al., 2021).
CVEK PARTIAL PULPOTOMY
Cvek partial pulpotomy is a vital pulp procedure which debrides 2 mm of coronal injured pulp from a root canal. The removal of the superficial injured pulp will allow the remaining vital pulp to continue the maturation and physiological development of the roots (Mejàre & Cvek, 1993; Sari, 2002). Cvek partial pulpotomy is similar to Apexogenesis in that it removes some coronal pulp, leaving a vital healthy pulp in the roots of immature teeth, the only difference is that the amount of partial-pulpotomy using the Cvek treatment is fixed at 2 mm, whereas, the amount of partial-pulpotomy for apexogenesis can be less or greater according to the skill of the clinician and relative to the extent of damage to the immature tooth trauma because of the size and position of the caries or fracture (Shah et al., 2022). The long-term healing success of Cvek partial pulpotomy can exceed 93% (Mejàre & Cvek, 1993).
CONVENTIONAL NON-SURGICAL ROOT CANAL TREATMENT
The gold standard treatment for most mature teeth with a painful and/or necrotic pulp is a conventional non-surgical root canal treatment (Nagendrababu et al., 2020). It is a necrotic pulp and irreversible pulpitis procedure for mature teeth which uses instruments, irrigants, and chelating agents to debride infected tissues, and disinfects the root canal by cleaning, shaping, sealing, and obturation (Metzger et al., 2010; Peters, 2004). The long-term survival rates for teeth following non-surgical endodontic treatment can exceed 86%, and the tooth survival after non-surgical endodontic retreatments can exceed 78% (Elemam & Pretty, 2011).
REGENERATIVE ENDODONTICS
This is a necrotic pulp and irreversible pulpitis procedure which debrides tissues from the root canal, disinfects the root canal, instruments the periapical tissues through the open root apical foramen to cause bleeding into the canal to revascularize it. In addition, it introduces a scaffold or biological procedure within the root canal to promote vital tissue formation which will continue the deposition of mineral to strengthen dentine and grow the roots of immature teeth (Namour & Theys, 2014; Wigler et al., 2013; Wikström et al., 2022). In a study which compared blood clot revascularization (BCR), versus platelet-rich plasma (PRP), versus platelet-rich fibrin (PRF), it was discovered that RPR and PRF may be more successful in terms of accomplishing apical closure or a decrease in the size of the root apex, periapical healing response, and root lengthening (Murray, 2018). In a case report by Prasad et al. (2018) apical bridge formation only occurred in incisors treated with PRF.
The outcomes of regenerative endodontic treatment can be highly variable, from a high pooled survival and healing rate of 97%, whereas, if 20% radiographic changes were used as a cut-off point, there were only 16% root lengthening and 40% root thickening (Ong et al., 2020). A meta-analysis and systematic review by Tong et al. (2017) concluded that many knowledge gaps still exist within published studies, and current published evidence is unable to provide definitive conclusions on the predictability of regenerative endodontic outcomes. Furthermore, a meta-analysis and systematic review by Torabinejad et al. (2017) concluded that the literature lacks high-quality studies with a direct comparison of MTA and regenerative endodontic treatment. There is no consensus in using regenerative endodontic procedures in previously treated immature teeth, as at a long-term recall visit, five retreated teeth showed partial or complete apical closure (Cymerman & Nosrat, 2020). The treatment options for failing regenerative endodontic procedures, include apexification, or repeating the regenerative endodontic procedure. Regenerative endodontic retreatment was successful in three cases (Chaniotis, 2017) and a case report (Nosrat et al., 2021).
Regenerative endodontics has the unique potential advantage of being able to continue the root development in immature permanent teeth, thereby potentially saving the teeth for the lifetime of the patient. However, in conventional endodontic root canal treatment, Cvek partial pulpotomy, apexogenesis, and apexification, should always be provided when these treatments are more likely to benefit the patient because they can be more successful than regenerative endodontics (Murray & Garcia-Godoy, 2012).
CONCLUSION: CONTRAINDICATIONS, CONSIDERATIONS, AND ADVANTAGES OF REGENERATIVE ENDODONTICS
Regenerative endodontics will likely continue to be highly controversial, even as the knowledge gap of practitioners and researchers decrease. Thus, ultimately the decisions and choices for the endodontist, must be based on their own skills and knowledge, and the willingness of the patient, their parents, and guardians to save their traumatized tooth.
In the interests of keeping this review concise and unbiased, highlighting the good, the bad, and the ugly facets of regenerative endodontics has been undertaken. Some known advantages of regenerative endodontics are summarized in Table 2, while some practical tips, contraindications, and considerations for regenerative endodontics are summarized in Table 3.
| It is a root canal revascularization alternative treatment to apexification |
| It has the potential to save fragile immature permanent teeth over the long term by continuing root development to thicken the canal walls to help protect them against fracture |
| It can heal periapical lesions and continue apex development |
| It can restore sensitivity to teeth |
| It can prevent the loss of permanent teeth in children and young adults and their lifelong need for dental implants, bridges, or dentures |
| Never provide regenerative endodontics to fully developed teeth, because the body of literature has established that traditional endodontic treatment has a better prognosis |
| Consider if the immature permanent tooth with a necrotic pulp can be saved with apexification or conventional non-surgical root canal treatment, before attempting regenerative endodontics |
| A failure to adequately disinfect the root canal will risk spreading the infection and necrosis to adjacent tissues |
| Never use full strength or undiluted disinfectants. Sodium hypochlorite (NaOCl) must be diluted to a concentration of 1.25% or less, and continuous suction must be used to prevent its leakage, because of the risk of toxic chemical injury to the vital periapical tissues |
| Only debride the intracanal necrotic or infected tissues. Never use hand files or rotary files to instrument the root canal walls or enlarge the apical foramen, because it risks weakening the thin dentinal walls, which may fracture the tooth |
| Never leave the root canals empty, because revascularization will fail if bleeding cannot be established into the entire root canal space |
| Never place donor blood in a root canal, and never add unanchored exogenous stem cells into root canals, because of the potentially severe health hazards |
| Never pack the MTA below the level of the cementoenamel junction, because it will prevent dentine regeneration at that weak tooth fracture point |
| Consider avoiding the use of minocycline for disinfecting root canals to help prevent subsequent tooth discoloration |
| Consider using Biodentine or other biomaterials as intracanal barrier alternatives to white MTA |
| Consider restoring the cervical third of the immature tooth with composite and or fibre posts where these teeth are most prone to fracture |
AUTHOR CONTRIBUTIONS
The corresponding author is the sole contributor for this article.
CONFLICT OF INTEREST
The author is not attempting to sell any product or service to readers. Furthermore, the author denies a conflict of interest that would cause an undue bias, such as the problems and failures of regenerative endodontics to be hidden from readers of this review. For the purposes of full disclosure to readers, the author was involved in drafting the guidelines for the American Association of Endodontists (AAE) on regenerative endodontics. The author has spoken about regenerative endodontics to the American Dental Association and several other national dental and endodontic associations. The author has accepted funding to pursue research on several aspects of regenerative endodontics. The author has obtained ethical approvals to supervise endodontic residents in clinical trials of regenerative endodontics. The author is the holder of an expired patent for an endodontic regeneration kit. The author has a publishing agreement with Springer-Verlag and other textbook publishers to write book chapters on regenerative endodontics. The author's views are his own, he does not write on behalf of any agency, ethics board, editorial board, endodontic or dental association. Moreover, the author is grateful for this opportunity to write this review to disclose the problems and failures, so that they can be prevented, to benefit patients and endodontists.
ETHICAL APPROVAL
This review did not require ethical approval, because it does not present any identifiable human subjects' data. However, as a background, all prior institutional ethical approvals have been obtained to collect all data pursuant to this review, without any acts of misconduct, and without any rule violations by the author.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.