Present status and future directions: Removal of fractured instruments
Funding information
Self-funded.
Abstract
The success rate of fractured instrument retrieval varies because it is dependent mainly on several factors including the visibility of the fractured instrument, the length of the fractured instrument in relation to the curvature of the canal and the techniques applied to each case. This review aims to update the present status on removal of fractured instruments to identify factors and variables that could affect the success of fractured instrument retrieval based on both the preparation techniques and the instrument retrieval techniques. On the other hand, future directions of fractured instrument retrieval should focus on management of nonvisible fractured instruments since the removal of those instruments is deemed unpredictable with the current techniques, whereas the removal of visible fractured instruments is considered predictable now. Another possible direction of it is that there might be no more instrument fracture due to possible significant changes in the root canal preparation technique which may dispense with the use of rotary instruments.
INTRODUCTION
The presence of fractured endodontic instruments within the root canal system has a negative prognostic effect on orthograde endodontic treatment (Spili et al., 2005) since they hinder the cleaning and shaping of the apical root canal (Lin et al., 2005). Additionally, there has been an increase in the incidence of instrument fracture within root canals since the introduction of nickel-titanium (NiTi) rotary instruments (Gambarini, 2001; Ruddle, 2004) since they break more frequently than stainless steel (SS) hand instruments (Tzanetakis et al., 2008). Specifically, the fracture rates of SS hand instruments and NiTi rotary instruments are 0.25%–6% (Crump & Natkin, 1970; Hülsmann & Schinkel, 1999; Iqbal et al., 2006; Spili et al., 2005) and 1.3%–10.0% (Iqbal et al., 2006; Ramirez-Salomon et al., 1997; Spili et al., 2005; Wu et al., 2011), respectively. Moreover, 66%–78% and 91% of NiTi rotary instruments have been reported to fracture because of cyclic and torsional fatigue failure respectively (p < .01; Shen et al., 2009). This suggests that fractured NiTi rotary instruments were most likely not engaged in the canal walls. Contrastingly, fractured NiTi hand instruments, which rotate very slowly with more apical and lateral pressure, were most likely engaged in the canal walls, and therefore were more difficult to remove due to increased torsional engagement with the canal walls. Additionally, austenitic-phased NiTi instruments have a super-elastic tendency to straighten out in a curve leaning on the outer curvature wall, which leads to more resistance to dislodgement compared with those in a straight canal.
Accordingly, it is easier and more important to prevent instrument fracture than performing instrument retrieval. The most effective means of reducing the incidence of instrument fracture may involve changing how the instruments are used in root canals. For example, compared with the rotary motion, the reciprocating motion of NiTi rotary instruments significantly reduces the cyclic fatigue (De-Deus et al., 2010; Karataş et al., 2016; Varela-Patiño et al., 2010; Webber, 2015). Additionally, files made using thermally-treated NiTi (M-Wire) have physical and mechanical properties that increase flexibility and improve resistance to cyclic fatigue compared with files made using conventionally processed NiTi wires (Al-Hadlaq et al., 2010; Johnson, 2007; Pereira et al., 2012; Ye & Gao, 2012). A previous study (Gündoğar & Özyürek, 2017) showed that HyFlex EDM files (Coltene/Whaledent) in the martensitic phase at body temperature had a higher cyclic fatigue resistance compared with Reciproc (R25; VDW) and WaveOne (Primary; Dentsply Maillefer) files manufactured from M-Wire in the austenitic phase at body temperature, which perform the reciprocal motion. This could be attributed to HyFlex EDM files having a higher austenite transformation finish temperature than Reciproc and WaveOne files (Gündoğar & Özyürek, 2017). Regardless, instrument fracture can occur even when using recently developed thermomechanically treated NiTi endodontic instruments as long as they are made of metal (Shim et al., 2017).
The aim a to perform a critical review and discuss the current clinical techniques for fractured instrument removal as well as provide a clear direction for future clinical developments based on current literature.
PRESENT STATUS
Incidence of instrument fracture
The incidence of instrument fracture widely ranges from 0.4% to 23% (Alapati et al., 2005; Al-Fouzan, 2003; Iqbal et al., 2006; Pettiette et al., 2002; Ramirez-Salomon et al., 1997; Schafer et al., 2004; Spili et al., 2005). Notably, the incidence of instrument fracture amongst endodontists was as high as 5% (Alapati et al., 2005; Parashosh et al., 2004; Shen et al., 2009). Additionally, 93.6% and 79.5% of endodontists and general practitioners, respectively, have experienced instrument fracture (Madarati et al., 2008). This could be attributed to endodontists treating more challenging cases in molars compared with non-endodontists. Contrastingly, other studies have demonstrated that the incidence of instrument fracture amongst dentists with low experience is higher than that amongst dentists with higher experience, including specialists (Ehrhardt et al., 2012; Fiore et al., 2006; Iqbal et al., 2006; Knowles et al., 2006; Ramirez-Salomon et al., 1997; Shen et al., 2009; Tzanetakis et al., 2008; Wolcott et al., 2006).
More instruments are fractured in molars, especially mandibular molars, than in anterior teeth (Tzanetakis et al., 2008), which is due to several factors, including canal accessibility, root canal diameter and root canal curvature (Cujé et al., 2010; Nevares et al., 2012; Shen et al., 2004). The incidence of instrument fracture is significantly greater (almost thrice) in molars than in premolars (Iqbal et al., 2006). Furthermore, the prevalence of instrument fracture in the apical third (52.5%) was found to be significantly higher than that in the coronal third (12.5%) and middle third (27.5%) of the canal (Tzanetakis et al., 2008).
Instrument fracture is influenced by the canal anatomy; moreover, it is determined at the discretion of the treating clinician. There is a positive correlation between anatomical challenges in root canals and the incidence of instrument fracture since both the radius and angle of the canal curvature are the main determinants of the fatigue resistance of NiTi files (Alghamdi et al., 2020; Pruett et al., 1997; Shen et al., 2004). Moreover, a recent study reported decreased fatigue resistance for all instruments in canals with middle or coronally located curvatures than in canals with apical curvatures (Alghamdi et al., 2020).
Amongst specialists, reciprocating file systems were found to have a lower incidence of instrument fracture than rotary files systems (Ahn et al., 2016; Bueno et al., 2017; Cunha et al., 2014); moreover, compared with rotary motion, reciprocating motion has been proven to be safer against cyclic fatigue and torsion fracture (Ahn et al., 2016; Kim et al., 2012). Accordingly, instruments with reciprocating motions have an extended lifespan (Pirani et al., 2014).
Martensite-phase NiTi files at body temperature have a higher fatigue resistance than austenite-phase ones (Alghamdi et al., 2020; Shen et al., 2011; Vasconcelos et al., 2016). Increased temperature decreases the resistance to cyclic fatigue failure for all types of NiTi instruments (Shen et al., 2018). Additionally, Pedullà et al. reported that instruments with a 0.04 taper in the martensitic phase had a higher cyclic fatigue resistance than those with a 0.06 taper (Pedullà et al., 2020), which indicates that the extent of tapering is negatively correlated with the resistance to cyclic fatigue. From a dimensional perspective, the diameter of similarly designed files is negatively correlated with the fatigue life (Schneider, 1971). Therefore, a file with a large diameter and extensive taper is less resistant to cyclic fatigue than files with lesser values for these parameters, especially around the curve. Shen et al. reported similar torsional fatigue resistance of the NiTi instruments in both martensitic and austenitic phases; contrastingly, martensite-phase NiTi instruments showed significantly higher cyclic fatigue resistance than austenite-phase ones (Shen et al., 2018). Taken together, the incidence of instrument fracture can be greatly reduced by using a file with a small diameter and less taper in the martensitic phase at body temperature to shape the canal, especially around a severe curve (Hieawy et al., 2015; Pedullà et al., 2020).
Factors affecting instrument retrieval
The dental operating microscope (DOM) along with small-diameter ultrasonic tips allow minimally invasive root canal preparations and facilitates the safe removal of fractured instruments (Cujé et al., 2010; Fu et al., 2011; Nevares et al., 2012; Suter et al., 2005; Ward et al., 2003; Wong & Cho, 1997). Here, visualization and accessibility to the fractured instruments are crucial factors for successful instrument retrieval (Nevares et al., 2012). Accordingly, predictive factors for instrument retrieval include instrument retrieval protocols (Carr, 1992; Eleazer & O’Connor, 1999; Gettleman et al., 1991; Pierre & Reit, 2003; Roig-Greene, 1983; Ruddle, 2004; Wong & Cho, 1997); location, visibility, size, length, and type of the fractured instrument; root canal curvature; curvature radius; and operator experience and fatigue (Alomairy, 2009; Cujé et al., 2010; Gencoglu & Helvacioglu, 2009; Pruett et al., 1997; Rahimi & Parashos, 2009; Shen et al., 2004; Souter & Messer, 2005; Terauchi, 2012; Terauchi et al., 2021; Ward et al., 2003).
Tooth type
The tooth type affects the success of instrument retrieval based on anatomical tooth factors, including visualization and accessibility to the fractured instrument (Cujé et al., 2010). The retrieval success rate for fractured instruments that are visible inside the root canal was approximately twice that for instruments that were not visible (Nevares et al., 2012). Posterior teeth have more complex root anatomy than anterior teeth. Specifically, the roots of posterior teeth exhibit curvature and concavities, which typically cannot be detected clinically or 2D-radiographically, and thus may induce iatrogenic accidents during retrieval attempts. Therefore, instrument retrieval from posterior teeth is considered more difficult than that from anterior teeth in addition to the fact that limited mouth opening in patients increases the difficulty of fractured instrument retrieval. Furthermore, compared with mandibular teeth, maxillary teeth allow easier retrieval of fractured instruments due to the force of gravity directing the fractured instrument into a coronal direction.
Types of instrument fractures
Instruments fracture through two mechanisms, namely cyclic and torsional fatigue. Cyclic fatigue results from repetitive tension/compression cycles when rotating in a curved canal. Torsional fatigue can be induced when the instrument rotates whilst binding within the canal (Cheung, 2007; Yum et al., 2011). However, torsional fatigue does not occur when using ultrasonics in both the preparation and retrieval phases since the procedure does not involve rotation of the fractured instrument, which can lead to torsional fatigue failure. Secondary fractures of fractured instruments may result from cyclic fatigue caused by ultrasonic vibration. Martensite-phase NiTi instruments showed higher cyclic resistance than conventional or austenite-phase NiTi instruments (Lee et al., 2019). Fractured austenite-phase NiTi instruments tend to straighten out on the outer curvature wall, which may require a longer time for extending the space along the inner wall to loosen them given the instruments’ restoring forces despite the creation of an inner space of about one-third of the fractured instrument length. Alternatively, compared with austenite-phase NiTi instruments, fractured SS or martensite-phase NiTi instruments of the same length exhibit lower restoring forces, and therefore may require less preparation and retrieval time (Peters et al., 2017). It may take more time to retrieve or secondary fractures may occur more frequently for fractured austenite-phase, compared with martensite-phase, NiTi instruments in the canal whilst activating ultrasonics on them.
Length of the fractured instrument
Most fractured instruments in root canals are made of NiTi (Spili et al., 2005), with the mean fragment length being 3 mm (Jiang et al., 2010; Wu et al., 2011). Wu et al. showed that files with a larger diameter or more taper led to a longer fragment length than those with lower corresponding values (3.32 ± 0.73 mm vs. 2.42 ± 0.73 mm; Wu et al., 2011). A recent study showed that a longer fragment length (>3.1 mm) and canals with greater curvature (>30°) led to longer preparation time, which could result from a significantly increased contact area along the canal walls (Fu et al., 2011). Fractured instruments of 4.6–5.7 mm required at least double the time for ultrasonic retrieval compared with those <4.5 mm (34 s on average). It may be difficult to remove fractured instruments >5.7 mm using ultrasonics solely. Contrastingly, most fractured instruments <4.6 mm could be solely removed using ultrasonics within 10 s. A recent study showed that for each 1-mm increase in the fragment length, the preparation time is expected to increase by 79.9 s (Fu et al., 2011). Additionally, the fractured instrument length may be correlated with the canal curvature (Fu et al., 2011); specifically, shorter instruments (<3.1 mm) related to smaller canal curvatures (<30°) were mostly loosened within <1 min and removed from the canal using ultrasonics within a few seconds. Therefore, the fractured instrument length is positively correlated with the preparation and retrieval times in accordance with the canal curvature.
Size of the fractured instrument
Compared with small-diameter files, large-diameter files presented a higher fracture incidence around a curve (Wu et al., 2011). The preparation time for loosening the fractured instruments was positively correlated with the fractured instrument length since longer fragments require a greater dentin amount to loosen (Terauchi et al., 2021).
Location of the fractured instrument
Wu et al. reported that 47.5% and 61.5% of the NiTi instruments fractured in the mesiobuccal canals of the mandibular and maxillary molars respectively (Wu et al., 2011). Moreover, most NiTi instruments are prone to fracture in the apical third of root canals (Iqbal et al., 2006; Wu et al., 2011). Therefore, there is a high, moderate and low success rate for removing fractured instruments located before, around and beyond the canal curvature respectively (Iqbal et al., 2006; Lopes et al., 2007; Ward et al., 2003).
Root canal curvature
NiTi instruments show a greater tendency to fracture in canals with a curvature >25° than those with a curvature <25° (p < .001; Farid et al., 2013; Wu et al., 2011). Moreover, the success rate of instrument retrieval significantly dropped from 83% to 43% when the canal curvature was >20° (Cujé et al., 2010; Shen et al., 2004). Additionally, the retrieval success rate was found to be favourable when the canal curvature was low and the curvature radius was >4 mm (Alomairy, 2009; Cujé et al., 2010; Estrela et al., 2008). Fractured instruments located in curved canals >30° required long times to remove in both the preparation and retrieval phases; contrastingly, fractured instruments below 3.1 mm could be easily removed using ultrasonic instruments regardless of canal curvature (Terauchi et al., 2021). Taken together, the retrieval success rate is negatively and positively correlated with the canal curvature and radius, respectively, due to increased visibility and accessibility (Alomairy, 2009; Fu et al., 2011).
Operator fatigue and experience
The duration of instrument retrieval attempts should not exceed 45–60 min since the success rates may drop with increased treatment time (Suter et al., 2005). The reduced success rate could be associated with the operator's fatigue or procedural accidents, including canal perforation and over-enlargement, which may predispose the tooth to vertical root fracture.
Furthermore, there were significant differences in the instrument retrieval time and dentin sacrifice rates between experienced and less experienced operators (p < .05; Terauchi et al., 2007), which indicates that experienced operators can predictably remove fractured instruments without unnecessarily sacrificing tooth structure or causing iatrogenic accidents.
Instrument retrieval protocols
Instrument retrieval protocols can be divided into three categories: mechanical, chemical and surgical methods. Surgical methods should be performed as a last resort since they are invasive and require a significant amount of dentin sacrifice involving root-end resection when the fractured instrument is in the apical or middle third of the canal. However, surgery should be considered first when the fractured instrument is mostly extruded beyond the apical foramen or completely outside the root since it does not require an invasive amount of dentin sacrifice. Chemical methods using solvents, including iodine trichloride, nitric acid, hydrochloric acid, sulphuric acid, iodine crystals and iron chloride solution, to corrode the fractured metallic instrument (Hülsmann, 1993), as well as electrolysed sodium fluoride and sodium chloride solutions for instrument dissolution as an electrochemical process (Ormiga et al., 2010), are inefficient for instrument retrieval given the considerably long time required to dissolve the whole metallic instrument. Moreover, they are considered unpredictable since these chemical solvents can only touch the fractured instrument surface in the canal, which may cause damage to the surrounding soft and hard tissues. Therefore, compared with nonmechanical methods, mechanical methods, especially those using ultrasonics, allow higher success rates, minimally invasive preparation and faster instrument retrieval (Cujé et al., 2010; Fu et al., 2011; Nagai et al., 1986; Nevares et al., 2012; Terauchi et al., 2021). However, the success rates of instrument retrieval using ultrasonics widely vary from 33% to 100%, with the average retrieval time ranging from 3 to >60 min (Alomairy, 2009; Nagai et al., 1986; Terauchi et al., 2007, 2021) due to differences in the instrument retrieval protocols according to the location and visibility of the fractured instrument (Al-Fouzan, 2003; Cujé et al., 2010; Ramirez-Salomon et al., 1997; Ruddle, 1997; Terauchi et al., 2021; Ward et al., 2003). Nonetheless, compared with nonmechanical methods, mechanical retrieval methods are more reliable and practical; accordingly, they are frequently used in clinical settings.
MECHANICAL PROTOCOLS FOR INSTRUMENT RETRIEVAL
All mechanical protocols for instrument retrieval comprise two steps. The first step is preparing the root canal using rotary or ultrasonic instruments to loosen the fractured instrument. The next step is making retrieval attempts using special devices or ultrasonics to remove the fractured instrument.
Generally, mechanical methods for instrument retrieval can be classified into two groups, namely those involving trephine burs to trough the fractured instrument periphery in the preparation step followed by removal attempts using devices and those involving ultrasonics or special files to create a tiny space only on the side of the fractured instrument in the preparation step followed by removal attempts using devices or ultrasonics. These devices include special files and loops to remove the fractured instruments.
Mechanical devices involving trephine burs include the Masserann Kit (Micro-mega), Cancellier Extractor Kit (SybronEndo), Endo Extractor (Brasseler Inc.), Endo Rescue (Komet/Brasseler), Micro-Retrieve & Repair System (Superline NIC Dental) and iRS (Dentsply Tulsa Dental). These systems use a hollow cutting-end tube with a diameter of 0.7–2.4 mm to expose the coronal portion of the fractured instrument in the preparation step. However, they require considerable dentin sacrifice to place the extractor for grabbing the fractured instrument given the large diameter tube used with respect to the canal size. Therefore, the use of trephine burs of any size is restricted to anterior teeth or straight portions in posterior teeth (Friedman et al., 1990; Nagai et al., 1986; Okiji, 2003; Ruddle, 2004) since both the trephine burs and large-diameter extractors are used in a straight line to the fractured instrument. The use of such instruments around a curve to the fractured instrument may cause additional complications, including excessive dentin removal and root perforation, which may predispose the tooth to root fracture over time (Hashem, 2007; Saunders et al., 2004; Souter & Messer, 2005; Spili et al., 2005). Taken together, systems involving trephine burs can be used to remove fractured instruments only in the coronal third of the canal mainly in anterior teeth.
Systems involving ultrasonics or special files include the Canal Finder System (FaSociete Endo Technique); EndoPuls system (EndoTechnic); and small-diameter ultrasonic tips, including a CPR-7 titanium alloy ultrasonic tip (Obtura-Spartan Corp.), ET25 (Satelec Corp) and TFRK-S (DELabs). The systems comprise a special handpiece and special files, which generate a vertical movement to bypass the fractured instrument (Hülsmann, 1990; Lévy, 1990). However, great caution is required when bypassing the fractured instrument around a curve given the risk of perforating the root canal, pushing the fractured instrument in a further apical direction, or even extruding the fractured instrument beyond the apical foramen. Moreover, instrument retrieval using the Canal Finder System has an overall success rate of only 68% (Hülsmann & Schinkel, 1999). Compared with the aforementioned systems, ultrasonics are safer, more conservative in dentin sacrifice and more successful even in posterior teeth in both the preparation and retrieval steps (Cujé et al., 2010; Terauchi et al., 2007, 2021). Nonetheless, all the aforementioned protocols are not standardized for predictable instrument retrieval, which is attributed to their differences in the success rates of instrument retrieval. However, a recent study suggested that fractured instruments visible under a DOM can be predictably removed using ultrasonic instruments alone through a single standardized retrieval protocol that minimizes potential variables (Terauchi et al., 2021) compared with the aforementioned nonstandardized protocols (Table 1).
| Author | Year | Study design | Sample size | Tooth | Separated fragment | Intervention | Time (median) | Definition of success | Success rate |
|---|---|---|---|---|---|---|---|---|---|
| Hulsmann et al (Hülsmann, 1990) | 1990 | In vivo and ex vivo comparative study | n = 62 | Human dentition | N/A | Canal Finder System and ultrasonics | N/A | Retrieval or bypass | Overall: 58% (36/62) Removal: 37% (23/62) Bypassing: 21% (13/62) |
| Hulsmann et al (Hülsmann & Schinkel, 1999) | 1999 | In vivo Case series | n = 113 | Human dentition | H-file, Reamers, lentulo, GG, light speed, profile, ultrasonic file | Canal Finder System | N/A | Retrieval or bypass | Overall: 60% (13/22) Removal: 32% (7/22) Bypassing: 27% (6/22) |
| Yu et al (Yu et al., 2000) | 2000 | Ex vivo Comparative study | n =18 | Incisors | H-Files #25, #40, #50 | Nd:YAG laser | 5.1 min | Retrieval | Overall: 56% (10/18) |
| Ebihara et al (Anjo et al., 2004) | 2003 | Ex vivo comparative study | n = 24 | Single rooted human teeth | K-File | Nd:YAG laser | 5.28 min | Retrieval | Overall: 63% (5/8) |
| Ward et al (Ward et al., 2003) | 2003 | Ex vivo | n = 90 | Simulated canals artificial blocks and extracted human teeth | Profile.04% taper rotary file | Ultrasonics | N/A | Retrieval |
Overall: 79 (71/90) Artificial blocks: Before curve and at the curve 100% (20/20) Beyond the curve 25% (5/20) Extracted teeth: Before curve and at the curve 100% (10/10) After Curvature 60% (6/10) |
| Shen et al (Shen et al., 2004) | 2004 | In vivo | n = 72 | Different maxillary and mandibular teeth | Profile Rotary files & NiTi k files | Bypassing the fragment by using hand files, then Removing the SI by ultrasonic vibration of either K-files or ultrasonic tips; if not removed, then by Braiding the fragment with Hedstro€m files | N/A | Bypass or Retrieve |
Overall: 53% (38/72) Removal: 44% (32/72) Profile rotary file 41% NiTi k files 60% Before curvature 100% After curvature 60% maxillary and 30% mandibular |
| Souter et al (Souter & Messer, 2005) | 2005 | In vivo and Ex vivo |
Ex vivo: n = 45 vivo: n = 60 |
Mesiolingual canals of mandibular molars | Profile file (#35/.04 taper) | Ultrasonics and GG platform | N/A | Retrieval |
Ex vivo: 91% (41/45) In vivo: 70% (42/60) |
| Terauchi et al (Terauchi et al., 2006) | 2006 | In vivo case reports | n = 4 | Mandibular molars | Manual k files and rotary Ni Ti files | Loop device | N/A | Retrieval | Overall 100% |
| Terauchi et al (Terauchi et al., 2007) | 2007 | Ex vivo | n = 98 | Mandibular incisors |
#20/0.10 taper Rotary file |
Masserann kit (N = 33) Ultrasonics (N = 35) File Removal System (N = 30) |
FRS needed less time than US and Masserann kit | Retrieval |
Masserann kit: 91% (30/33) Ultrasonic: 86% (30/35) File Removal System: 100% (30/30) |
| Alomairy (Alomairy, 2009) | 2009 | Ex vivo comparative study | n = 30 | Mesial canals of molars | Profile.06 taper rotary endodontic instruments |
Ultrasonics (N = 15) Instrument Removal System (N = 15) |
40 min for US 55 min for IRS |
Retrieval |
Overall success 70% (21/30) Ultrasonics: 80% (12/15) Instrument Removal System: 60% (9/15) |
| Gencoglu and Helvacioglu (Gencoglu & Helvacioglu, 2009) | 2009 | Ex vivo | n = 93 | 63 straight canals & 30 curved canals | Not specified | K-files in straight and curved canals Ultrasonics in straight and curved canals Masserann only in straight canal | N/A | Retrieval or bypassing |
Overall 93.3% Ultrasonics: 94% (34/36) K-files: 75% (27/36) Masserann: 48% (10/21) |
| Caje et al (Cujé et al., 2010) | 2010 | In vivo | n = 170 | Maxillary and mandibular teeth | Manual k files and rotary Ni Ti files | Ultrasonics | N/A | Retrieval |
Overall: 95% (162/170) Maxillary molars 93% Maxillary premolars, anteriors, canines and mandibular canines 100% |
| Fu M et al (Fu et al., 2011) | 2011 | In vivo retrospective study | N/A | N/A | Manual k files and rotary Ni Ti files | Ultrasonics | N/A | Retrieval | Overall: 88% (58/66) |
| Nevares et al (Nevares et al., 2012) | 2012 | In vivo | n=112 | Maxillary and mandibular posterior teeth | Manual and rotary NiTi files | Ultrasonics alone or associated with bypassing with hand files | N/A | Retrieval or bypassing |
Overall: 71% (79/112) Visible SI: 85% (58/112) Invisible SI: 48% (21/112) |
| Shiyakov et al. (Shiyakov & Vasileva, 2014) | 2014 | In vivo comparative study | n = 45 | Mandibular and Maxillary molars |
Stainless steel files Ni Ti rotary files Lintulo spirals |
Ultrasonics Bypass |
N/A | Retrieval or Bypassing |
Overall: 64.44%(29/45) Ultrasonics: 84.61%(22/26) Bypass: 36.84%(7/19) |
| Pierre et al. (Wohlgemuth et al., 2015) | 2015 |
Ex vivo Comparative study |
n = 36 | First and Second molars | #10, #15, #20 K-file | GentleWave System | 10.44 min | Retrieval |
Overall: 72% Apical: 61.3% Midroot: 83.3% |
| Himani et al. (Garg & Grewal, 2016) | 2016 | Ex vivo comparative study | n = 40 | Mandibular First and second molars | Protaper F2 | Ultrasonics with staging platform using ProUltra and EMS tips |
Proultra: 63.89 min EMS: 50.22 min |
Retrieval |
Overall: 87.5% Mild curvature:100% Moderate curvature: 90.9% Severe curvature: 80.95% |
| Musale et al. (Musale et al., 2016) | 2016 |
In vivo Case report |
n = 1 | Lower first primary molar | H file | Ultrasonics | N/A | Retrieval | 100% success |
| Yang et al. (Yang et al., 2017) | 2016 | Ex vivo comparative study | n = 43 | Mandibular molars | K3 #25/.06 | Ultrasonics with staging platform using microtube or trepan bur with microtube |
Ultrasonic/microtube: 25 min Trepan bur/microtube: 9 min |
Retrieval | Overall: 46% |
| Xu et al. (Xu et al., 2017) | 2017 |
Ex vivo Comparative study |
n = 23 | Mandibular molars | K3 #25/.06 | Microtrepan bur and/or microtube | N/A | Retrieval | Overall: 100% |
| Alireza et al. (Adl et al., 2017) | 2017 |
Ex vivo Comparative study |
n = 60 | Mandibular First molars | Flex Master, K3, RaCe and Hero Shaper #30/.04 | Bypassing using K-files #8,#10,#15 | 30 min | Bypassing in less than 30 min | Overall: 91.6% |
| Yang et al. (Yang et al., 2017) | 2017 | Ex vivo comparative study | n = 21 | Mandibular molars | K3 25/.06% | Ultrasonics and trephine burs |
Trepan bur group (8.9 ± 3.5 min) ultrasonic group (25 ± 11.9 min) |
Retrieval |
Overall success 100% dentin thickness & geometry with trephine bur >ultrasonics. |
| Arya et al. (Arya et al., 2019) | 2019 | In vivo | n = 3 |
|
Manual and rotary Ni Ti files | Retrieval using ultrasonics | N/A | Retrieval | Overall: 100% |
| Meidyawati et al. (Meidyawati et al., 2019) | 2019 | In vivo case report | n = 1 | Mandibular first molar | Manual k file | Micro-forceps | N/A | Retrieval | 100% |
| Arslan et al. (Arslan et al., 2020) | 2020 | In vitro comparative study | n = 30 | Dentin blocks | Apical 5 mm of rotary instruments with different taper. | Ultrasonic tips with different tapers and assessment of time of activation that leads to secondary fracture and failure of retrieval process using 25/.08 K3XF, 25/.06 K3XF, and 25/.04 K3XF instruments | N/A | Non occurrence of secondary fracture of ultrasonic tips | Taper.08% fractured less than.06% and.04%. |
| Yue X et al. (Meng et al., 2020) | 2020 | Comparative Ex vivo study | n = 69 | N/A |
Stainless steel group and nickel titatium group. (n = 23 each) |
|
N/A | Retrieval |
|
| Meng et al. (Meng et al., 2020) | 2020 | Ex vivo | n = 34 | Mandibular incisors | 5 mm apical 25.06% k3 rotary file | Trepan bur/microtube technique | 8.55 ± 5.81 min | Retrieval time for retrieval | Overall success rate 76.47% |
| Pruthi P et al. (Pruthi et al., 2020) | 2020 | Comparative Ex vivo study | n = 80 | Mandibular molars | ProTaper F1 in coronal one third and middle one third | Proultra ultrasonic tips versus Terauchi file retrieval kits (TFRK) | Mean time for TFRK was less than ultrasonic tips | Retrieval |
Overall success 90% ultrasonics group 95% for TFRK group |
| Terauchi et al. (Terauchi et al., 2021) | 2021 | In vivo Comparative study | n = 128 | 75 molars, 28 premolars, and 25 anterior teeth | Manual and rotary Ni-Ti files. | Mean time assessment for retrieval of broken instrument using ultrasonics and loop device | 3.68 min | Retrieval |
Overall success 100% 89.8% using ultrasonics alone |
| Pradhan et al (Pradhan et al., 2021) | 2021 | In vivo | n = 1 | Lower first molar | Rotary Ni Ti instrument | Retrieval using ultrasonics | N/A | Retrieval | Success 100% |
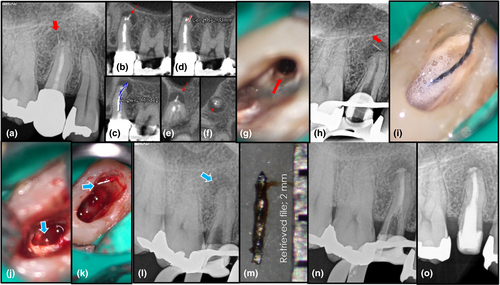
STANDARDIZED PREPARATION PROTOCOL FOR VISIBLE INSTRUMENT RETRIEVAL
First, cone-beam computed tomography (CBCT) imaging is preoperatively used to measure the fractured instrument length and canal curvature as well as to locate the inner wall of the fractured instrument. The canal curvature is calculated by measuring the angle generated by a straight line drawn from the orifice to the coronal end of the fractured instrument and a line parallel to its long axis (Cujé et al., 2010; Estrela et al., 2008; Lin et al., 2005; Suter et al., 2005). Subsequently, the treatment protocol for instrument retrieval is developed based on the CBCT findings.
The preparation step begins with canal enlargement to the fractured instrument using a no. 2 or 3 Gates Glidden (GG) drill when the canal curvature is <15° or a large-diameter martensite-phase NiTi file size, including the #60/.02 taper HyFlex EDM finishing file (Coltene/Whaledent AG), when the canal curvature is >15°. If the initially encountered canal size is larger than the no. 3 GG drill, the canal is not enlarged. However, GG drills can still be used to just enlarge the straight canal portion before the curve using a brushing motion against the outer wall to reduce the curvature.
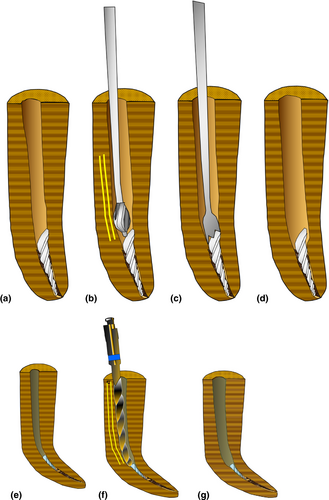
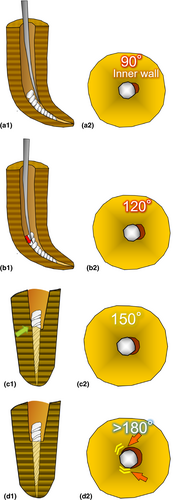
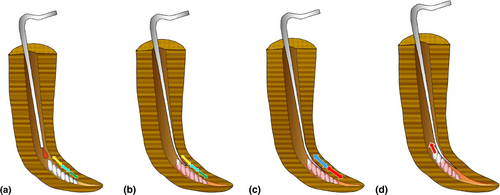
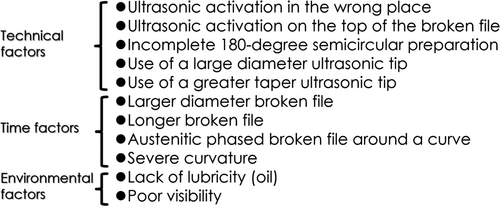
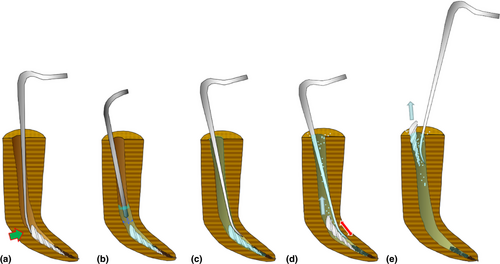
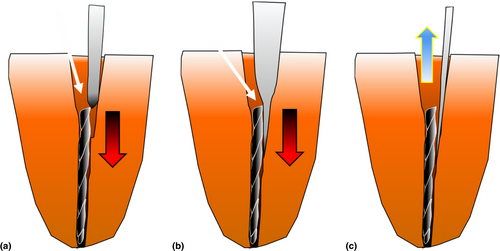
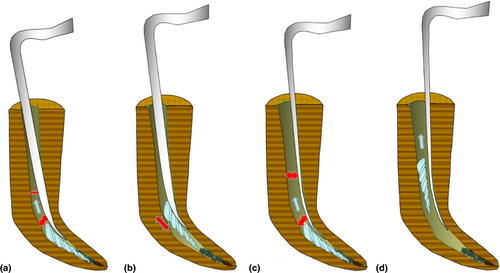
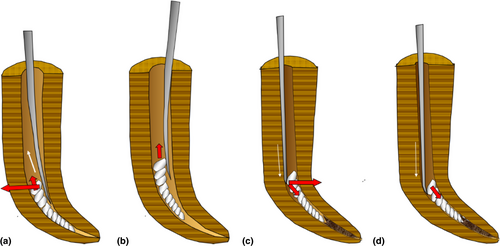
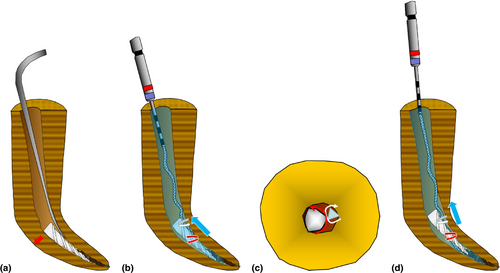
Subsequently, a microtrephine (DELabs) bur is used to expose the coronal 1-mm portion of the fractured instrument when the canal curvature is <15° (Figure 1), but not when the canal curvature is >15° since it may cause ledge formation around the curve. Small-diameter ultrasonic tips such as TFRK-12/6/S ultrasonic tips (DELabs) or tips modified into a sword shape are used to cut a 90° semicircular space on the inner wall of the fractured instrument, which is extended to 180° using a straight spear-shaped ultrasonic tip to loosen the fractured instrument. When the fractured instrument is in a straight line canal, the semicircular space is created on the thickest canal wall side observed on the axial view of the CBCT image. The space depth to be cut is generally one-third of the fractured instrument length (Figures 2 and 3); furthermore, the space bottom is required to be even in the semicircular space (Figure 3). However, in case the fractured instrument is not loosened even after cutting beyond one-third of the instrument length, the space should be extended more apically loosening is observed or the fractured instrument is relocated from its original position. An apical extension of the space may be required, especially for austenite-phase fractured instruments or canal curvatures >30° (Figure 4). Ultrasonic preparations should be performed at 10%–20% of the maximum power setting (Cujé et al., 2010; Lin et al., 2005; Tzanetakis et al., 2008) using clear silicon oil as the lubricant with reasonable visibility or under dry conditions. The preparation phase is considered complete upon observation of loosening of the fractured instrument under the DOM even before the semicircular space reaches 180°, which is followed by the retrieval attempt phase. In case loosening of the fractured instrument is not observed with ultrasonics after the aforementioned preparation procedures, it is important to reconsider three main factors that affect successful loosening of the fractured instrument, which are described in Figure 5.
STANDARDIZED PREPARATION PROTOCOL FOR NONVISIBLE INSTRUMENT RETRIEVAL
Similar to visible instrument retrieval, the treatment plan for nonvisible instrument retrieval is made based on the CBCT findings. Subsequently, the canal is enlarged to the nonvisible fractured instrument as described above.
Visible and nonvisible instrument retrieval have almost similar preparation protocols. The only difference is that the preparation phase for nonvisible instrument retrieval is limited to a 90-degree semicircular space on the inner wall performed without visualization, which makes it unpredictable. Large flexible martensite-phase NiTi rotary files, including the #60/.02 taper HyFlex EDM finishing file (Coltene/Whaledent), are used to enlarge the curved canal portion to the fractured instrument in the presence of EDTA. The canal size should be approximately 0.15 mm larger than the fractured instrument size, which should be wider than the ultrasonic tip used to create space on the inner wall to allow the removal of the fractured instrument through the space. No canal enlargement is required if the canal size is thrice larger than the coronal diameter of the fractured instrument.
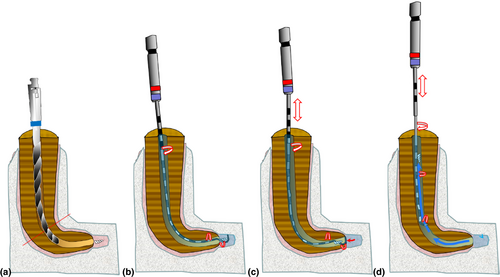
Since the fractured instrument cannot be initially visualized and the semicircular space created in the preparation phase cannot be predictably extended from 90° to 180°, wet conditions are required throughout the procedure. First, the canal should be filled with oil (biocompatible silicone oil) to facilitate loosening the fractured instrument in the preparation phase since this step is performed without visualization and the tactile sensation obtained from the ultrasonic tip is the only predictor of determining whether the fractured instrument is loosened. For successful loosening of the fractured instrument in nonvisible conditions, it is important to first obtain a sticky (resistance) feeling when withdrawing the ultrasonic tip from the space between the canal wall and fractured instrument, which indicates engagement to the canal wall. Second, it is important to be aware of any sudden transition from a sticky feeling to a loose feeling upon withdrawal whilst deepening the space by moving the ultrasonic tip in an up/down motion, which suggests that the fractured instrument is loosened. Moreover, the canal should be periodically irrigated with EDTA to remove debris.
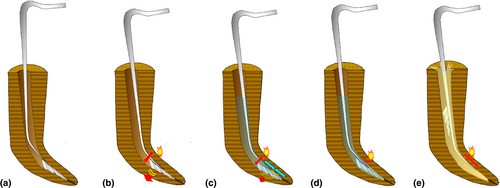
In nonvisible conditions, the ultrasonic tip should be thin and sharp enough to feel the tiny gap between the inner canal wall and the fractured instrument. First, a thin spoon-shaped tip (TFRK-6/12, DELabs) or a customized sword-shaped tip is precurved to fit the canal curvature and used to grope for a sticky feeling obtained with the fingers holding the handpiece (Figure 6a). In case a large-sized tip, including a greater tapered or progressive-tapered tip, is used, the ultrasonic tip placed in the space will push the fractured instrument in an apical direction due to the large diameter before the creation of a thin space in the gap between the fractured instrument and inner wall. Moreover, it is quite common to hear or feel a click and obtain a sticky feeling when the sharp ultrasonic tip slides over the fractured instrument into the gap in the inner wall. If a sticky feeling is obtained when the ultrasonic tip is withdrawn from the gap, it is important to obtain a radiograph with the ultrasonic tip placed in the gap to confirm its position on the inner wall. In case the radiograph reveals that the ultrasonic tip in the gap on the inner wall, the tip is ultrasonically activated to initiate a 90° semicircular preparation (Figure 6). Specifically, the ultrasonic tip is directly activated on the fractured instrument from the inner curve in both pecking and pulsing motions throughout the preparation phase to prevent secondary fracture and tip breakage. It is almost infeasible to create a 180° semicircular space or laterally extend the space in nonvisible conditions. For similar reasons, the ultrasonic activation intensity should be as low as practically possible, that is, it should not exceed 30% of the maximum power in the preparation phase. Since this conservative preparation step continues with ultrasonic activation directed to the fractured instrument on the inner wall, any dentine walls in contact with the fractured instrument are eliminated through indirect ultrasonic vibration transferred from the ultrasonically vibrating tip via the fractured instrument, which eventually results in fragment loosening (Figure 6b–e). The preparation phase is considered complete when the sticky feeling with the ultrasonic tip is lost or when the fractured instrument emerges from the nonvisible curve, with the retrieval phase being conducted next. The advantage of this preparation technique is its minimal invasiveness; contrastingly, its disadvantage is the unpredictability of complete loosening of the fractured instrument as well as the risk of secondary fracture or tip breakage if aggressively performed. Additionally, successful loosening of the fractured instrument is always time-consuming.
In case the fractured instrument is beyond the apical foramen, it is unnecessary to prepare the canal for instrument loosening since the fractured instrument outside the canal is already loose given that it lies just in the apical extent of the intracanal space without any walls holding it. In this condition, if the extracanal space is closed similarly to the root canal space, the fractured instrument can be simply irrigated out of the canal with saline using ultrasonic irrigation devices, including ProUltra PiezoFlow (Dentsply) and GentleWave (Sonendo, Inc).
Instrument retrieval protocol using ultrasonics
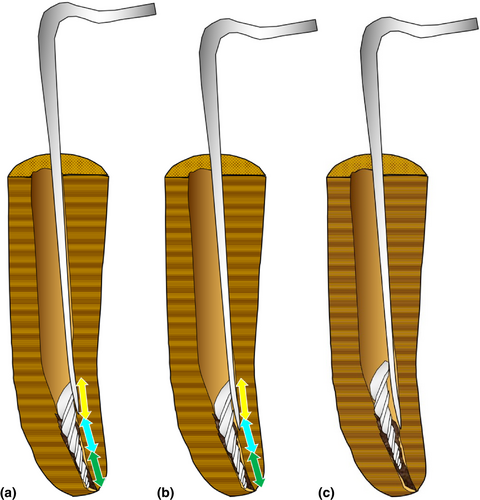
After completion of the preparation phase, it is important to confirm that the outer canal wall is smooth until the coronal extent with no overhangs blocking the fractured instrument from retrieval. In case there is an overhang on the outer wall, it should be removed using either a flexible NiTi rotary file or an ultrasonic tip. Before attempting to retrieve the fractured instrument with ultrasonics, the canal is dried using air from the Stropko irrigator (DCI International), which can lead to ejection of the fractured instrument. This is because the fractured instrument is already disengaged from the canal walls during the preparation phase and the blown air that bounces back from the bottom can cause the loosened fractured instrument to float from the canal walls and exit from the root canal.
First, the canal is filled with soybean oil or EDTA when the canal curvature is >30° or <30°, respectively, to facilitate instrument retrieval with ultrasonics. Most fractured instruments (94%) <4.6 mm can be removed solely with ultrasonics within 10 s in the retrieval phase (Terauchi et al., 2021).
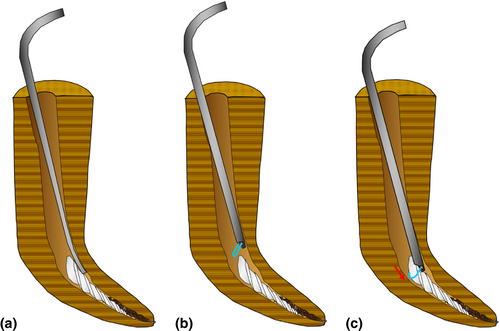
Subsequently, instrument retrieval attempts are performed in wet conditions by filling the canal with an appropriate fluid, including EDTA and soybean oil, until the cavosurface (at least to half the pulp chamber level and ‘not just in the root canal’) in order to take advantage of cavitation and acoustic streaming in facilitating instrument removal using ultrasonics. If only the root canal is filled with fluid, the fractured instrument may not exit from the canal; instead, it may float within the root canal space during ultrasonic activation. Next, the ultrasonic tip is placed in the space and is continuously activated at a power setting 10%–20% higher than that used in the preparation phase, with short up-and-down strokes being performed on the inner curve until the fractured instrument is removed, which is usually achieved in 10 s (Terauchi et al., 2021; Figure 7). For ultrasonic removal attempts, the power setting can be safely increased since the ultrasonic tip is more resistant to fracture in wet conditions than in dry conditions. Moreover, the depth of ultrasonic-activated fluid increases proportionally to the applied power setting for removing debris apical to the ultrasonic tip in the canal (Malki et al., 2012). Moreover, the ultrasonic tip should be placed and activated on the inner wall as far away as possible from the fractured instrument, which provides space for ejection through the canal opening. Four reasons could contribute to unsuccessful instrument retrieval using ultrasonics within >10 s. The most typical reason is that the dancing fractured instrument might be stuck between the outer canal wall and the vibrating ultrasonic tip with a progressive taper or a large diameter (Figure 8). The second reason could be the space between the outer wall and ultrasonic tip being smaller than the fractured instrument diameter, which leads to no open space for the fractured instrument to escape (Figure 9). The third reason could be that the fractured instrument might relocate into a more radicular direction after being pushed by the vibrating ultrasonic tip from the top or outer wall (Figure 10). Finally, the fourth possible reason is the amount of fluid filled in the canal space being insufficient to create acoustic streaming and cavitation for removing the fractured instrument from the canal.
In case the fractured instrument is not retrieved within 10 s using the aforementioned protocols or it is initially longer than 5.7 mm, other retrieval techniques using the loop device or XP Shaper (XPS) rotary instrument (FKG Dentaire SA) should be attempted since it is difficult or time-consuming to keep using ultrasonics (Terauchi et al., 2021).
Fluid types used for ultrasonic instrument retrieval
The ability of a fluid to lubricate the fractured instrument in the root canal space and flush it away with the aid of ultrasonic-generated acoustic streaming and cavitation generated is mainly dependent on the fluid characteristics, including lubricity, viscosity and surface tension. Viscosity is defined as a fluid's resistance to flow and shear. The hydrodynamic force in high-viscosity fluids necessitates a high ultrasonic power setting to generate high pressure for dynamic impact on the fractured instrument since high-viscosity fluids absorb weak oscillatory shockwaves. In addition, aggressive oscillatory shockwaves generated by the high ultrasonic activation with high-viscosity fluids can create more powerful hydrodynamic pressure for pushing the fractured instrument compared with those with low-viscosity fluids. However, ultrasonic activation at a high power setting can cause ultrasonic tip breakage. Generally, fluids with high viscosity and surface tension reduce both acoustic streaming and cavitation, but increase lubricity, and vice versa. Water is a low-viscosity fluid with high surface tension (72 mN/m at 20°C), vegetable oil (e.g., soybean or olive oil) is a medium-viscosity fluid with low surface tension (23–32 mN/m at 20°C), syrup is a high-viscosity fluid with high surface tension, and ethanol is a low-viscosity fluid with low surface tension. Corn or soybean oil has a lower viscosity than olive oil (Sahasrabudhe et al., 2017). Generally, the fluid temperature is negatively correlated with the surface tension. Taking these factors into consideration, fluid with medium viscosity and low surface tension, including soybean/corn oil, may be ideal for use with a high ultrasonic power setting for fractured instrument retrieval, especially for canal curvature >30°; contrastingly, EDTA can be used with a medium power setting for canal curvature <30°. Additionally, the size of ultrasonic tips is negatively correlated with the generated acoustic streaming, with the resulting velocity being positively correlated with the power setting (Ahmad et al., 1987). Cavitation refers to the formation of ultrasonic-generated vapor-containing bubbles within a fluid. Forced bubble collapse causes implosions that cause an impact on surfaces, which produce shear forces that can dislodge the fractured instrument from the canal. Fluids with low surface tension result in more ultrasonic-generated oscillatory shockwaves on the fractured instrument, which make it more vulnerable to dislodgement and ejection by the continuous pressure waves of acoustic streaming and cavitation from the trapped space.
Accordingly, EDTA, which has a low surface tension, is expected to facilitate immediate instrument removal from a straight canal given that it also removes hard-tissue debris produced during ultrasonic activation to clear out the way. Contrastingly, the loosened fractured instrument may not be ejected from a severe curve (>30°) in the presence of low-viscous EDTA, which may insufficiently lubricate the fractured instrument. The use of soybean oil, which has medium viscosity and low surface tension, for instrument removal from a severe curve using ultrasonics could enhance lubrication. However, compared with EDTA, soybean oil results in slower instrument removal from a curve <30° given its medium viscosity. Nonetheless, both fluid types can allow cavitation and acoustic streaming as well as decrease friction generated between the fractured instrument and the canal wall to facilitate instrument retrieval. Therefore, using a mixture of EDTA and soybean oil may be an alternative for instrument removal from a moderate curve (30°–20°).
Instrument retrieval protocol using the loop system
The XPS should be used to retrieve fractured instruments leaning against the outer wall with no space for loop placement over the fractured instrument. Otherwise, the loop is used to remove fractured instruments >4.5 mm or in case of unsuccessful instrument retrieval using ultrasonics within >10 s. Unlike ultrasonics and the XP-Endo Shaper, which are used in wet conditions, the loop is used in dry conditions since it should be visualized throughout the retrieval procedure. Additionally, loop systems, including EndoCowboy (Köhrer Medical Engineering), BTR Pen (CERKAMED) and Yoshi Loop (DELabs), can be used to engage and remove long loosened fractured instruments through forces directed more coronally.
Loop placement in the canal requires a space with a diameter ≥0.4 mm; moreover, the coronal portion of the fractured instrument should be peripherally exposed by a depth ≥0.7 mm deep for grasping by the loop system. A #40 plugger is placed into the same space to measure the area created adjacent to the fractured instrument. This allows the introduction of the loop, which has a slightly smaller diameter than the #40 plugger, into the canal for engagement. Next, the loop size should be adjusted to fit the coronal diameter of the fractured instrument using an endodontic explorer, including a DG16 endodontic explorer (Hu-Friedy). Specifically, the tip of the DG16 endodontic explorer is placed in the loop, followed by tightening the loop around it. The apical portion of the DG16 is used to decrease and increase the loop size and coronal portion, respectively. Next, the loop is bent to 45° instead of 90° to facilitate loop placement over the fractured instrument since it occupies more room. Subsequently, the loop is inserted into the canal and pushed back to 90° upon the fractured instrument. The loop is then tightened around the loosened fractured instrument and pulled to smoothly retrieve it from the canal. In case any resistance is felt, the loop is slowly and gently pulled in different directions with a swaying motion until it is lifted from the canal. It should never be forced in a vertical direction to prevent breakage since the instrument retrieval is solely dependent on the pulling direction.
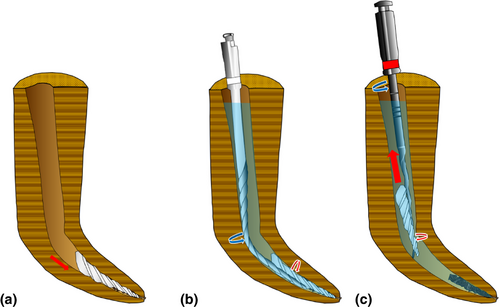
Instrument retrieval protocol using the XP-endo Shaper
The XP-endo Shaper (FKG) is a unique rotary system made of a novel heat-treated MaxWire alloy with a size 15 booster tip that allows expansion of its core from size 27/.01 to a larger taper of ≥30/.04 at body temperature (Azim et al., 2017). The XP-endo Shaper allows instrument retrieval given the expandability of the file whilst being rotated clockwise inside the canal. It is straight in the martensitic phase at room temperature and expands to a snake-like shape with a taper of ≥.04 upon exposure to intracanal (body) temperature due to transformation to the austenitic phase. This allows the instrument to extensively touch and scrape the canal walls or possibly scratch and spin the loosened fractured instrument if there is a thin space along the fractured instrument inside the root canal. Clockwise rotation of the XP-endo Shaper in a swirling motion on the side of the disengaged fractured instrument causes counterclockwise rotation of the fractured instrument. This could eventually facilitate an unscrewing movement of the fractured instrument in the coronal direction (Figure 11). This movement can be facilitated by using vegetable or silicone oil as a lubricant, which also prevents breakage of the XP-endo Shaper. A limitation of the XP-endo Shaper is its low resistance to torsional fatigue failure compared with conventional NiTi rotary instruments due to its smaller taper (Silva et al., 2018). Accordingly, the XP-endo Shaper should be rotated at a relatively high speed (>2000 rpm) with 3–5 mm up/down strokes along the fractured instrument to mitigate torsional and cyclic fatigue. Moreover, the short up/down strokes yield vertical movement to facilitate instrument retrieval. Recent studies on the effect of rotational speed have demonstrated that the XP-endo Shaper allows more efficient and safer advancement of the instrumentation within the small canal space when rotated at 3000 rpm than when rotated at 1000 rpm, where it follows the small root canal space around the curve into the space created between the fractured instrument and the inner wall without major adverse effects (Azim et al., 2018; Webber et al., 2020). Taken together, the XP-endo Shaper can be used for instrument removal with rotation at a high speed in the presence of an appropriate oil, especially for >5.7 mm fractured instruments leaning against the outer canal wall without space for loop placement.
Instrument retrieval protocol using the XP-endo Finisher
The XP-endo Finisher (FKG Dentaire) is a size #25 nontapered instrument that does not damage or alter the original root canal anatomy. It is mainly used to clean the root canal by scraping irregularities on the canal walls given its high flexibility as well as its ability to expand up to a 6-mm diameter and adapt to the root canal three-dimensionally (Azim et al., 2016; Leoni et al., 2017). This is facilitated by its change to a spoon shape after exposure to intracanal temperature following transformation to the austenitic phase, as previously described for the XP-endo Shaper. The XP-endo Finisher can effectively remove accumulated hard tissue debris and the smear layer from the root canal system (Elnaghy et al., 2017; Leoni et al., 2017). Moreover, a recent study demonstrated the efficacy of the XP file in removing calcium hydroxide paste from artificial grooves within the apical third of a root canal system (Wigler et al., 2017).
Therefore, the XP-endo Finisher can be used at a high-speed clockwise rotation speed to remove a loosened fractured instrument from a wider canal, especially when the instrument is extruded beyond the large apical foramen into the apical tissues, by braiding it and creating a swirling fluid flow in the coronal direction (Figures 12 and 13). Additionally, the braiding technique can be performed using a Hedström or K-type file to retrieve fractured instruments located deep in the canal that cannot be observed on a DOM. However, successful retrieval using these files is solely dependent on tactile sensation, which makes them unpredictable for instrument retrieval (Shen et al., 2004; Suter et al., 2005). Moreover, braided Hedström files or K-files often detach during removal attempts (Ahmad et al., 1987).
SUMMARY OF INSTRUMENT RETRIEVAL TECHNIQUES
Taken together, only three instrument retrieval techniques are recommended for cases with various conditions. Table 2 summarizes the recommended instrument retrieval techniques with respect to instrument length, instrument size, curvature, and visibility.
| Length of the fractured instrument | Visibility | Curvature | Technique |
|---|---|---|---|
| <3.1 mm | Visible | Any curvature | US |
| 4.4 mm ≦ BF ≧3.1 mm | Visible | <30° | US |
| 4.4 mm ≦ BF ≧ 3.1 mm | Visible | >30° | Loop/RF |
| ≧4.5 mm | Visible | Any curvature | Loop/RF |
| ≧3.5 mm ≧ size #80 | Non-/visible | Any curvature | Loop/US/RF |
| <3.1 mm | Nonvisible | Any curvature | US/RF |
| 4.4 mm ≦ BF ≧ 3.1 mm | Nonvisible | <30° | US/RF |
| 4.4 mm ≦ BF ≧ 3.1 mm | Nonvisible | >30° | RF |
| ≧4.5 mm | Nonvisible | Any curvature | RF |
Note
- US, ultrasonics; RF, rotary files such as the XP-endo shaper/Finisher.
Prognosis of the retained fractured instrument
The presence of fractured instruments in the root canal before completing the cleaning and shaping procedures negatively affects the prognosis since it hinders the cleaning of the canal space apical to the fractured instrument. Moreover, aggressive attempts to remove a fractured instrument from a curved canal without proper diagnosis may cause complications, including excessive dentine sacrifice, secondary instrument fracture, root perforation, or even root fracture (Hashem, 2007; Saunders et al., 2004; Souter & Messer, 2005; Spili et al., 2005). The fractured instrument within or outside the root canal does not necessarily induce postoperative disease. Instead, postoperative conditions result from an increase in the number of surviving bacteria, which become virulent due to favourable environmental changes to promote postoperative periapical disease (Moller et al., 2004). The closer the root canal preparation is to the terminus upon instrument fracture, the better the outcome (Torabinejad & Lemon, 2002). Instrument fracture that occurs in the later stage of canal instrumentation, especially if it is within the apex, has the best prognosis since the canal can be well debrided and is relatively free from microbes (Torabinejad & Lemon, 2002). In case there is no preoperative periapical lesion associated with the root, the fractured instrument does not affect prognosis (Crump & Natkin, 1970) and can be incorporated into the root canal filling materials (Figure 14). If the fractured file can be predictably removed without excessive dentine sacrifice, the prognosis should not be reduced. Taken together, the treatment prognosis is more dependent on removing the microbes rather than the fractured instrument itself. Failure to clean the space apical to the fractured instrument may negatively affect the prognosis similarly to endodontically treated cases with missed canals or ledge formation blocking the debridement of the root canal space apical to the ledge (Cohen & Burns, 2002; Cohen & Hargreaves, 2006; Gutmann & Lovdahl, 2010; Harty et al., 1970; Kapalas & Lambrianidis, 2000; Namazikhah et al., 2000; Nevares et al., 2012; Roig-Greene, 1983). Although cases with a retained instrument in the canal could have a poor prognosis, a systematic review found a favourable prognosis in most cases involving fractured instruments (Panitvisai et al., 2010). The most important prognostic factor for teeth with retained fractured instruments is the presence of preoperative periapical lesion. Specifically, endodontically retreated teeth with preoperative lesions have a poor prognosis when the fractured instruments are retained (Panitvisai et al., 2010; Spili et al., 2005).
Future directions in the removal of fractured instruments
Currently, using a DOM in combination with ultrasonic instruments is highly effective for removing fractured instruments (Cujé et al., 2010; Fu et al., 2011; Nagai et al., 1986; Nehme, 1999; Terauchi et al., 2021; Ward et al., 2003; Wu et al., 2011). However, the use of loops is only effective when the fractured instrument is visible under the DOM. Nonvisible fractured instruments can only be removed if a thin ultrasonic tip can be placed in the space between the inner wall and the nonvisible fractured instrument (length: <4.6 mm). The preparation phase is the most important factor for successful instrument removal since most fractured instruments (94%) shorter than 4.6 mm can be removed using only ultrasonics within 10 s during the retrieval phase after the preparation phase (Terauchi et al., 2021). Nonvisible fractured instruments that are longer than 4.5 mm can be removed using rotary instruments such as the XP-endo Shaper only if it is possible to create a thin space between the canal wall and the fractured instrument using ultrasonics or bypass the fractured instrument. Additionally, a longer fractured instrument requires a longer preparation time, with extensive dentin removal along the inner canal wall for loosening (Terauchi et al., 2021). Moreover, Suter reported that the duration of the retrieval procedure was negatively correlated with the success rate of instrument retrieval (Suter et al., 2005).
Two future directions for instrument removal might mitigate the challenge of removing nonvisible fractured instruments longer than 4.5 mm that are beyond the curve. First, instrument fractures within the root canal might be eliminated due to significant changes in the root canal preparation technique. This may render rotary instruments unnecessary since future irrigation systems, including the GentleWave System (Sonendo, Inc), may play more crucial roles in root canal preparation than conventional instrumentation techniques. The GentleWave System is a multisonic irrigation technology that uses advanced fluid dynamics, acoustic energy and tissue dissolution chemistry to facilitate the cleaning of minimally instrumented canals or those without instruments (Haapasalo et al., 2014). Studies have extensively described this innovative technology and its mechanism of action (Haapasalo et al., 2014; Molina et al., 2015); moreover, it has shown initial treatment success rates as high as 97% at 6- and 12-month follow-ups (Sigurdsson et al., 2018). However, in retreatment, none of the commercially available efficient irrigation techniques, including the GentleWave System, has been shown to completely remove debris and residual obturation materials from the canals; furthermore, there were no significant differences in debridement between the GentleWave System and other irrigation techniques (Wright et al., 2019). Therefore, even the novel systems have a higher debridement efficacy, and further improvements are required until no instrumentation is necessary.
The second possibility is the future development of a novel instrument-removal file system comprised of several rotary files for canal preparation and removal of all types of fractured instruments, including nonvisible long instruments beyond the curve. The initial files could be used for canal preparation to create a small space for fractured instrument removal whilst the secondary files could be introduced into the created small space to actually remove the fractured instrument with clockwise rotation of the instrument-removal file. Ultimately, fractured instrument removal may become as easy as conventional root canal instrumentation, regardless of the visibility. The development of such instrument-removal files may render the use of the DOM and ultrasonics unnecessary. A fractured instrument in a straight root canal is easier to remove than one in a curved curve, which is consistent with the fact that a straight root canal is easier to prepare using rotary instruments than a curved root canal. Nonetheless, ultrasonic may remain necessary for some cases to facilitate the creation of a thin space along the fractured instrument to prevent ledge formation or canal transportation; additionally, they may be used in combination with rotary instruments to remove nonvisible long fractured instruments beyond a severe curve (Figure 15).
AUTHORS CONTRIBUTION
Yoshi Terauchi designed the project, Abielhassan MM and Ali WT acquired the data, all authors analyzed and interpreted the data, Abielhassan MM and Ali WT interpreted the previous evidence related to the same topic, all authors wrote the paper and contributed in writing the manuscript.
CONFLICT OF INTEREST
Authors deny any conflict of interest.
ETHICAL APPROVAL
The article is a narrative review that did not involve any procedures that needs pre ethical approvals.
Open Research
DATA AVAILABILITY STATEMENT
All data and cases presented are available with authors.