Present status and future directions—Vital pulp treatment and pulp preservation strategies
Funding information
Open access funding provided by IReL. WOA Institution: The University of Dublin Trinity College Blended DEAL: IReL hybrid OA 2022
Abstract
Therapeutic strategies focussed on the pulp preservation, are important when managing vital teeth with deep caries and an exposed pulp. These vital pulp treatments (VPTs); however, are not new, with indirect and direct pulp capping procedures being described as a therapy for carious teeth for over a century. As a result of unpredictable outcomes, the traditional indications for VPT particularly when the pulp was exposed were limited to the treatment of immature teeth with incomplete root formation. Over the last 20 years, the advent of regenerative endodontics and the promotion of biologically based therapies aimed at reducing intervention have reinvigorated VPT with new waves of basic science and clinical research indicating a role for VPT not only in mature cariously affected teeth, but also in teeth with signs and symptoms indicative of irreversible pulpitis. Driven by new materials such as hydraulic calcium silicate cements, a better understanding of pulpal immunity and biology as well and improved tissue handling, VPT has been at the forefront of treatment recommendations made by global Cariology and Endodontic organizations. Care must be exercised, however, as key gaps in scientific knowledge remain alongside severe limitations in educational dissemination amongst dentists. Although research has highlighted that carious injury to the dentine–pulp complex stimulates a wide range of responses and that the interaction between infection, inflammation and repair will eventually impact on the outcome of pulpitis, our ability to accurately and objectively diagnose the true inflammatory state of the pulp remains poor. An overreliance on symptoms leaves clinicians with subjective, crude diagnostic tools by which to inform treatment planning and decision-making, which results in large variations in the treatments offered to patients. Not only is there an urgent need to develop preoperative and intraoperative diagnostic tools, but there is also a paucity of the high-quality comparative evidence required to answer the most important questions and justify treatment options. The aim of this review was to consider the current status of VPT and to discuss the principle problems that are hindering clinical acceptance of these techniques. Potential solutions and opportunities are offered to suggest ways that VPT may become a more consistently prescribed evidenced-based treatment in dental practice.
INTRODUCTION
Vital pulp treatment (VPT) and the promotion of pulp preservation techniques find themselves at the centre of somewhat of a renaissance (AAE, 2021; ESE, 2019). Encompassing a broad range of techniques that focus on minimal intervention and maintaining healthy pulp tissue, VPT is not a novel treatment modality, but rather old with reports of gold being placed over the injured pulp attributed to Pfaff in the 18th century (Dammaschke, 2008; Glass & Zander, 1949). It is important to consider the history of pulp preservation techniques alongside the renewed interest in the area, as VPT's popularity has experienced numerous ‘peaks and troughs’ in the intervening years, with the enduring comment of Rebel in 1922 that the ‘exposed pulp was a doomed organ’ resonating with some even to this day (Rebel, 1922). Although considered ‘doomed’ in 1922, it was not until the 1940s and 50s that systematic robust research investigating pulp healing and the response to direct pulp capping were carried out, which contributed enormously to our understanding of the pulp's response to injury and subsequent repair, whilst also highlighting an unpredictability in the outcome of direct pulp capping (Glass & Zander, 1949; Nyborg, 1955, 1958). These results perhaps fuelled the scepticism surrounding VPT as an alternative to more conventional therapies, such as root canal treatment (RCT) with success rates at that time reported in that period of 60%–70% for direct pulp capping compared with 80%–90% for RCT (Nyborg, 1955, 1958; Strindberg, 1956). Although subsequent studies demonstrated that comparable outcomes to RCT were possible with VPT (Baume & Holz, 1981; Haskell et al., 1978), shifts in dentist's attitudes were tempered by the continuing ‘stream’ of other reports highlighting poor outcomes particularly after long-term follow-up (Barthel et al., 2000; Bjørndal et al., 2010). Conversely, over the last 20 years, several advancements have profoundly changed our thinking and reinvigorated the VPT area including, the advent of bioactive hydraulic calcium silicate cements (HCSCs) (Nair et al., 2008; Pitt Ford et al., 1996), improvements in our biological understanding of pulp reparative processes (Duncan et al., 2019; Smith et al., 2016) as well technical and biological improvements in wound lavage and tissue handling (Ballal et al., 2021; Bjørndal et al., 2019). These advancements have translated to excellent clinical outputs for pulp capping and pulpotomy at least in single-arm studies carried out by well-trained individuals (Marques et al., 2015; Taha et al., 2017; reviewed in Cushley et al., 2021). Curiously, the term VPT was always used as pseudonym for direct pulp capping, but recent definitions of VPT have simplified and broadened this to include all; ‘Strategies aimed at maintaining the vitality of the pulp’ (ESE, 2019), which of course includes one- and two-step selective caries removal techniques and indirect pulp capping to avoid pulp exposure as well as direct pulp capping and pulpotomy procedures. This new definition has not only expanded interest in the area to include cariologists, paediatric dentists, general dentists, operative dentists and endodontists, but has also served to shift mindset from considering RCT as the only option for the management of deep caries and the exposed pulp.
The aim of this review was to summarize the current position of VPT within dental and endodontic practice in four key areas, as well as considering the likely future innovations, research, education and dissemination that is required to strengthen the evidence-base and drive the area forward.
REVIEW
- Lack of consensus in decision-making when managing deep caries and the inflamed pulp
- Diagnostic issues when assessing and treating the inflamed pulp
- Clinical outcome evaluation for VPT in relation to the inflamed pulp
- Importance of tissue handling, VPT materials and visual inspection after carious exposure
Lack of consensus in decision-making when managing deep caries and the inflamed pulp
Present status
Although the conservative management of deep caries and the exposed pulp remains at the heart of operative dentistry, clinical decision-making in VPT remains divisive, with several research groups (Ricucci et al., 2019; Schwendicke et al., 2021) and recent Endodontic position statements providing conflicting advice in the area (AAE, 2021; Duncan et al., 2021b; ESE, 2019). The ESE position statement concurred with recent consensus papers produced by global experts working predominantly in Cariology (Innes et al., 2016; Schwendicke et al., 2016), who were concerned about over invasive treatment, such as pulp exposure and RCT as well as being encouraged by positive 5-year results from randomized clinical trials investigating one- and two-stage selective caries removal techniques (Bjørndal et al., 2017; Maltz et al., 2018). The specific need for Endodontics to add to the discussion on this issue was evident, as the Cariology position statements did not address the management of the exposed pulp, which seems incongruous when discussing the management of deep caries that is in close proximity to the pulp. Within the ESE position statement, it was recommended that ‘selective carious-tissue removal (one-stage or two-stage stepwise technique) is advocated in teeth with reversible pulpitis, provided radiographic assessment indicates caries has progressed no deeper than the pulpal quarter with a zone of dentine separating the carious lesion from the pulp chamber’ (ESE, 2019). On the contrary, the AAE suggests that ‘complete caries removal is essential to eliminate infected tissues and visualize pulp tissue conditions under magnification when pulpal exposures occur. Residual caries compromises necessary observations of pulpal inflammation levels for a diagnosis of more severe pulpitis’ (AAE, 2021). The ESE recommendation is considered evidenced-based (Duncan et al., 2021b), being supported by a recent clinical histological study highlighting reduced pulpal inflammation in deep versus extremely deep caries (Demant et al., 2021), and by high preservation of pulp vitality in 5-year comparative trial data (Bjørndal et al., 2017; Maltz et al. 2018). For cases presenting with more severe pulpitis, the ESE recommended that ‘carious exposure with symptoms indicative of irreversible pulpitis should be treated aseptically with pulpectomy. Alternatively, full pulpotomy may be successful in cases where there is partial irreversible pulpitis in the coronal pulp; however, better long-term prospective randomized data are required’ (ESE, 2019). Interestingly, the AAE did not go so far, limiting their recommendations to ‘utilizing direct visualization of the pulp, it appears that even symptomatic pulps may be candidates for VPT’ (AAE, 2021). In defence of the conflicting guidance for the treatment of spontaneously symptomatic pulpitis, a lack of clarity at present can be explained by a paucity of robust comparative studies required to support decision-making and guideline development in this area (Duncan et al., 2021a; ESE, 2019).
A lack of consensus on the most appropriate manner in which to manage deep caries has been translated to practice with multiple questionnaire-based studies from various geographical regions, demonstrating an absence of standardized decision-making between dentists treating deep caries (Careddu et al., 2021; Crespo-Gallardo et al., 2018; Edwards et al., 2021a, 2021b; Schwendicke et al., 2017; Stangvaltaite et al., 2013, 2017). A recent large openly distributed questionnaire-based study in the UK, which included case-based vignettes, highlighted large divisions in deep caries management of dentists from a range of backgrounds with 41% of dental practitioners carrying out non-selective (complete) removal, whilst indirect selective techniques were carried out by 57% of dentists (Edwards et al., 2021a). Notably, within the study, rubber dam usage was low (29%) as was the use of HCSCs and GIs during indirect pulp capping (Edwards et al., 2021a), which may reflect the remuneration system in the UK, but are not in keeping with recommendations made in this area to maximize a sterile field (ESE, 2019). Similarly, a Spanish study demonstrated that 65% of respondents removed carious tissue until hard dentine, and that this was considered important even at the risk of pulpal exposure (Crespo-Gallardo et al., 2018). Symptoms and patient age influence the management decision for the patient with the presence of even mild symptoms leading to more invasive therapies such as RCT (Careddu et al., 2021; Crespo-Gallardo et al., 2018); this is despite it being known that pulpitis is often painless (Michaelson & Holland, 2002) and that age is not a convincing factor in the success of VPT (Asgary & Egbhal, 2013; Asgary et al., 2015; Kang et al., 2017).
Position statements in Cariology present views on deep caries management that are based on exposure of the pulp being considered a negative prognostic factor (Innes et al., 2016; Schwendicke et al., 2016). Not all pulp exposures are the same of course and those caused by trauma and treated by pulp capping or pulpotomy, traditionally have a more predictable response and outcomes similar to vital pulpectomy and RCT (Al-Hiyasat et al., 2006; Cvek, 1978), whilst carious exposure and the addition of infection and advanced inflammation has generally reduced the predictability of the pulp cap or pulpotomy procedure to below 50% at least in studies in which the operator was an undergraduate student (Barthel et al., 2000) or a general dentist (Bjørndal et al., 2017). Crucially, operator influence and the use of an enhanced protocol using magnification, sodium hypochlorite lavage and HCSC (Bjørndal et al., 2019; ESE, 2019) have resulted at least in single-arm intervention studies to have success over 80% when at least some of these enhancements are employed (Bogen et al., 2008; Kundzina et al., 2017; Marques et al., 2015; Mente et al., 2014). The lack of comparative studies in this area, however, creates problems both in terms of the level of evidence available to aid guidelines and recommendations, but perhaps also demonstrates the ethical and practical difficulties in designing a trial in which one arm exposes the pulp and the other does not.
When decision-making is analysed in relation to carious pulp exposure in the UK, calcium hydroxide was selected by 66% and HCSCs in 20% for the choice in pulp capping (Edwards et al., 2021b). A definitive pulpotomy for the management of teeth with signs and symptoms indicative of irreversible pulpitis was selected by only 10% of dentists with the principal barrier for the provision of definitive pulpotomies cited as a lack of training (Edwards et al., 2021b). Indeed, management of the exposed pulp has also been highlighted as an area of considerable stress and concern for undergraduate dental students, as the opinions of teachers can vary and preclinical teaching opportunities and effective models are limited (Chevalier et al., 2021). Analysis of members of two endodontic societies in Ireland and Italy revealed that HCSC materials were commonly selected for managing the exposed pulp in over 70% of respondents, although oddly younger members of the Italian society preferred calcium hydroxide materials (Careddu et al., 2021) perhaps reflecting recent educational directions or financial constraints in that country. Younger dentists in both societies prescribed less RCT than older age groups, which perhaps reinforces the importance of undergraduate education in decision-making in this area (Careddu et al., 2021).
In summary, at present despite the volume of recent research and publication of several position statements from opinion leaders (AAE, 2021; ESE, 2019), consensus in the best way to manage deep caries and the exposed pulp remains weak. In the future, ways to improve decision-making in this area are of paramount importance to improve the consistency and predictability of VPT for patients (Duncan et al., 2021b).
Future directions
The promotion of strategies to preserve the vitality of the pulp is not only aimed at limiting intervention and the influence of restorative cycle (Elderton, 1993), but also ultimately to retain teeth. In order to provide coherent and consistent evidenced-based information for all dentists encountering deep caries and the exposed pulp, undergraduate and postgraduate education as well as research must align. It is impossible to identify another area of dentistry where such stark differences in ‘gold-standard’ management are evident. In the interests of patients, members of the Cariology and Endodontic community across the globe, should meet to discuss best way to manage deep caries, with a view to producing clear, logical and evidenced-based recommendations in order to avoid the variety of treatment currently delivered in primary and secondary (Duncan et al., 2021b).
Diagnostic issues when assessing and treating the inflamed pulp
Present status
It is evident that the success of VPT (Al-Hiyasat et al., 2006) and clinical decision-making (Careddu et al., 2021) is linked to the inflammatory state of the pulp and preoperative diagnosis (Careddu & Duncan, 2021). Although inflammation of the pulp can occur in response to chemical, thermal and mechanical irritation; it is not until the pulp tissue is challenged by microbes that vitality is threatened (Kakehashi et al., 1965; Möller et al., 1981). The cells of the dentine–pulp complex respond to irritation via a complex immune response including first odontoblasts, as well as a coordinated interaction of local and recruited immune cells (Duncan & Cooper, 2020; Farges et al., 2015). In addition, to the immune response, tertiary dentine is formed under the tubules adjacent to the carious lesion or irritant stimulus with a range of sub-types of tertiary dentine previously described in the literature, including, irritation, reactive, replacement or defence dentines (Duncan et al., 2019). More recently, the terms reactionary or reparative have been accepted as they relate more closely to both the biological process involved and the severity of the injury, with reactionary dentine formed by an upregulation of existing odontoblasts and reparative dentine formed after destruction of the existing odontoblast layer and the formation of new odontoblast-like cells from a progenitor cell population (Lesot et al., 1993; Smith et al., 1995). When the dental caries process breaches enamel and affects the superficial dentine, initially a mild inflammation is evident in the pulp horn adjacent to the lesion; however, a combination of intratubular dentine deposition leading to tubular sclerosis and tertiary dentine formation occurs, and after a short interval, the pulp is likely be of normal histological appearance (Warfvinge & Bergenholtz, 1986). This dynamic balance between inflammation and repair (Cooper et al., 2014) is critical to the repair and maintenance of the vitality of the dentine–pulp complex as removal of the irritation and an adequate restoration can allow the pulp to repair (Mjör & Tronstad, 1974). If the balance tips towards inflammation and the carious lesion is allowed to progress in the direction of the pulp, demineralization of the sclerotic dentine will occur and the caries will eventually advance into the tertiary dentine. At this stage, the severity of inflammatory changes in the pulp will significantly increase, with localized abscess formation and necrosis ensuing (Bergenholtz et al., 1982).
Notably, if the depth of carious (and by extension the position of infection in the tooth) is considered, significant levels of inflammatory cells are not observed in the pulp until the caries has penetrated to within approximately 0.5 mm (Reeves & Stanley, 1966). Recently, the relationship between caries depth and pulp inflammation has been examined histologically (Demant et al., 2021), with reference to the definitions of deep and extremely deep caries (ESE, 2019) with deep caries defined as ‘caries reaching the inner quarter of dentine, but with a zone of hard or firm dentine between the caries and the pulp, which is radiographically detectable’ whilst in extremely deep caries defined as ‘caries penetrating the entire thickness of the dentine radiographically’. In a study of 68 untreated teeth separated into deep and extremely deep caries, it was demonstrated that deep lesions the bacteria were generally confined to the primary dentine, whilst in extremely deep carious lesions bacteria were often in contact with the pulpal tissue and associated with the presence of an inflammatory infiltrate and partial pulp necrosis (Demant et al., 2021). In support of the influence of caries depth on outcome, a one-year clinical partial pulpotomy study comparing the American Association of Endodontists (AAE, 2013) and Wolters et al. classification (2017), demonstrated that not only were extremely deep caries more likely to expose, but they were also linked to more severe symptoms and subsequent failure of the procedure at one-year follow-up (Careddu & Duncan, 2021).
In light of these research data, it is odd that caries depth and the position of infection in the tooth have been largely ignored in relation to pulp diagnostic systems (AAE, 2013; Wolters et al., 2017), which rely predominately on patient symptoms. Indeed, management with inflammation of the pulp is currently categorized as being either reversible or irreversible in nature (AAE, 2013). Traditionally, the correlation between symptoms and the histological appearance of the pulp was considered to be poor (Dummer et al., 1980); however, a recent study highlighted that reversible and irreversible pulpitis may correlate with observational histological data based on the presence of necrotic change in the coronal pulp tissue (Ricucci et al., 2014).
Even in light of Ricucci's study, the current AAE system is problematic for a number of reasons with a dichotomy of salvageable or non-salvageable not reflected by the reported success of partial (Taha & Khazali, 2017; Uesrichai et al., 2019) and complete pulpotomy (Taha & Abdulkhader, 2018) in cases with signs and symptoms indicative of irreversible pulpitis. A diagnosis of irreversible pulpitis is used to determine need for RCT treatment (Swedish Council on Health Technology Assessment, 2010), which could potentially indicate that dentists are electing to remove a number of pulps which could be salvaged by conservative treatment. Furthermore, as the patient's pain history is subjective in nature and irreversible pulpitis may be asymptomatic in up to 60% of cases (Michaelson & Holland, 2002; Seltzer et al., 1963), objective measures of pulpal inflammation such as carious lesion depth, as well as clinical indicators of activity including progression rate, colour, sensibility tests (ESE, 2019) and potentially pulpal inflammatory biomarkers (Ballal et al., 2021) should perhaps be used as the basis of a more functional classification moving forward akin to those used for facial pain (Pigg et al., 2021) or in Periodontology (Papapanou et al., 2018).
Future directions
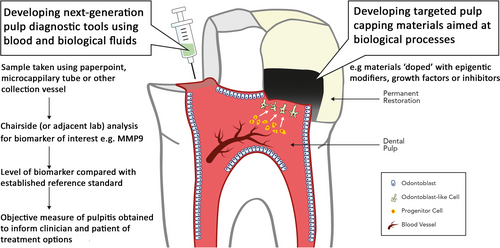
Global consensus indicates the need for a revised classification of infection-related pulp disease (AAE, 2021; ESE, 2019; Galicia & Peters, 2021; Rechenberg & Zehnder, 2020; Wolters et al., 2017). To this end, over the last few years, several groups have proposed novel, but yet unvalidated, nomenclatures as alternatives (Hashem et al., 2015; Rechenberg & Zehnder, 2020; Wolters et al., 2017). Although these new proposals represent a step in the right direction by removing the terms reversible and the ‘fatalistic’ irreversible, they also highlight the core problem in pulp diagnostic research, that is the absence of a reliable reference standard, as histological analysis is impossible in anything other than an extracted tooth. Unquestionably, the development of robust inflammatory (Ballal et al., 2021) or other biomarkers (Kearney et al., 2018; Rechenberg et al., 2016), which accurately reflect the level of inflammation in the pulp, offers hope of objective measures of pulp inflammation whilst preserving pulp vitality, maintaining the integrity of the tooth and directing treatment choice (Figure 1). This generally requires exposure of the pulp; however, as the volume of analyte retrieved from dentinal fluid in unexposed cavities is likely to be too small for robust analysis (Rechenberg et al., 2016; Zehnder et al., 2011). Furthermore, although attractive, biomarker analysis from pulpal blood is fraught with technical, practical and scientific challenges, which have been extensively reviewed elsewhere in this series (Zehnder & Belibasakis, 2021).
Clinical outcome evaluation for VPT in relation to the inflamed pulp
Present status
The recent European Society of Endodontology (ESE) initiative of systematically developing the highest-quality S3-level guidelines (Duncan et al., 2021a; Nothacker et al., 2014) for the treatment of pulpal and apical disease has revealed several key issues in the way outcome is currently assessed in Endodontics (Duncan et al., 2021c, 2021d). First, in the absence of a core outcome set (COS) for Endodontics (El-Karim et al., 2021; Williamson et al., 2012), the majority of outcome measures (OMs) currently employed to measure the success of Endodontic treatment are clinician-centred with comparatively few patient-centred OMs considered (Duncan et al., 2021c, 2021d). A focus on patient-centred OMs, with the addition of selected important clinician-centred OMs that can be clearly related to the patient, such as tooth survival, is at the core of the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) framework (Guyatt et al., 2011), which has recently been employed in S3-level treatment guidelines in Periodontology (Sanz et al., 2020). Within Endodontics, clinicians have long-relied on radiographic assessment of lesion size as a measure of treatment success (Ng et al., 2011), rather than retaining a functional and asymptomatic tooth and a feeling of well-being, which are important patient-centred outcomes.
Secondly, during the process of developing robust S3-level clinical guidelines, an initial systematic review of the literature is completed. It is of fundamental importance that the systematic analysis contains only comparative studies, including specifically randomized controlled trials, comparative non-randomized trials and longitudinal observational studies including comparative cohort and case–control studies (Sanz et al., 2020). These studies should be well-designed and adequately powered with a minimum follow-up of 1 year and ideally much longer up to 5 years (Duncan et al., 2020, 2021a). Unfortunately, at present, there is a paucity of comparative studies addressing many aspects of VPT, which undermines clinical development, consensus and ultimately the strength of recommendations contained in guidelines in this area. Furthermore, an often-ignored variable is the subject of meaningful comparison in randomized trials, a feature that was recently highlighted in a systematic review analysing the effect of wound lavage after carious exposure (Munir et al., 2020). Of the 27 eligible comparative trials investigating conservative treatment of the cariously exposed pulp, 24 randomized the pulp capping material (Munir et al., 2020) with many relatively small studies comparing two types of HCSCs (Hegde et al., 2017; Parinyaprom et al., 2018). Although these studies do provide value, it is likely that the biological and clinical properties of two HCSCs will be similar and a more relevant and interesting comparison could have been selected.
With regard specifically to management of deep caries, long-term trial evidence is available to support one- (Maltz et al., 2018) and two-stage (Bjørndal et al., 2017) selective caries removal in the permanent dentition as well as in studies with a mix of primary and permanent dentition (Orhan et al., 2010), albeit the published studies are from a limited number of research groups. Furthermore, in some of these studies, a reduction in the frequency of pulp exposure was a primary outcome measure in non-selective versus selective caries removal studies rather any change in outcome or survival (Khokhar & Tewari, 2018; Orhan et al., 2010). Pulp exposure is clearly a clinician-reported measure, and its true influence as a negative (or positive) prognostic factor remains unknown (Bjørndal et al., 2019). In summarizing available data, a recent Cochrane review including these papers (Bjørndal et al., 2017; Khokhar & Tewari, 2018; Maltz et al., 2018; Orhan et al., 2010) concluded after meta-analysis that for deep carious lesions, there was a greater probability of failure for non-selective (complete) carious removal compared with one-step and two-step selective removal (Schwendicke et al., 2021).
Notably, what is absent from the literature to date is any direct comparison of selective caries removal and treatment of pulp exposure (pulp capping and pulpotomy). There are trials comparing symptomatic pulpitis treated by RCT or pulpotomy, which show comparable results for postoperative pain and outcome (Eghbal et al., 2020; Galani et al., 2017), but not comparing selective removal and pulpotomy. There are several probable reasons for this, with ethical and methodological arguments prominent (Schwendicke et al., 2016), for example can caries be selectively removed in one group and non-selectively removed in the other with the higher risk of exposure in the latter? Furthermore, if the pulp remains unexposed in the non-selective group, is this tooth excluded from the study? If only the exposed samples remain in one arm of the study, they were more likely to be extremely deep carious lesions in which exposure was inevitable (ESE, 2019). This introduces bias as extremely deep lesions included in the exposed group will have greater levels pulpal inflammation and pathological change (Demant et al., 2021), which may make them more likely to fail than the selective caries group which will be a mix of deep and extremely deep caries. Previously, stepwise excavation versus pulp capping /partial pulpotomy was indirectly compared in Bjørndal et al., (2010), but the results are likely influenced by the variables discussed above. An alternative design would be to only include extremely deep lesions in the selective versus exposure trial; however, this creates other problems in that selective caries removal is not recommended for extremely deep caries only deep caries (ESE, 2019). This discussion highlights a challenging situation that outlines some of the challenges in designing trials to address the most important questions in Cariology, Endodontics and VPT.
If studies addressing the management of deep caries and the exposed pulp are considered, there are broadly speaking two types of study to consider generally based on patient symptoms. First, pulp preservation studies analysing management of the cariously exposed pulp with no or mild signs and symptoms (reversible pulpitis) and studies examining the exposed pulp with symptoms indicative of irreversible pulpitis. Addressing the first scenario, a recent systemic review investigated the question of pulp capping for carious exposure and a clinical diagnosis of no more than reversible pulpitis (Cushley et al., 2021). A general problem in primary VPT studies is that the preoperative diagnosis is not always specified, and often, a combination of symptomless, reversible and irreversible pulpitis is analysed together as carious exposure (Cushley et al., 2019, 2021). Within the Cushley et al. (2021) review, quality assessment highlighted a small number of fair to poor-quality non-randomized and five randomized trials with a high risk of bias (Awawdeh et al., 2018; Bjørndal et al., 2010; Kundzina et al., 2017; Parinyaprom et al., 2018; Suhag et al., 2019). From these pulp capping studies, pooled success for treatment with HCSCs was over 80% at 3 years, but calcium hydroxide was only 59%, and the authors concluded HCSCs to have a high level of success and predictably better than calcium hydroxide, but from a low quality of evidence (Cushley et al., 2021). Unfortunately, many of the studies investigating this issue are single-arm intervention studies or case-series (Bogen et al., 2008; Farsi et al., 2006; Kusumvalli et al., 2019), which although able to highlighted proof of principle and provide solid preliminary data, have a limited level of evidence. Recently, a pulp capping study with symptoms no more than reversible pulpitis compared NaOCl lavage with saline lavage in a randomized controlled trial of 1-year duration, with the results highlighting more painful failure in the saline group (Ballal et al., 2020) as well as improved outcome with 55% success for saline and 89% for NaOCl at 1 year (Ballal et al., 2021).
For the management of carious exposure with signs and symptoms indicative of irreversible pulpitis, a pulp cap is not generally considered to be the treatment of choice (Aguilar & Linsuwanont, 2011; ESE, 2019). As the caries process has progressed into the pulp and has bacterial infiltrate with accompanying pathological change (Demant et al., 2021; Ricucci et al., 2014), removal of pulp tissue either in a partial pulpotomy (Taha & Khazali, 2017) or full pulpotomy procedure is indicated (Simon et al., 2013). A recent systematic review analysed the effectiveness of coronal pulpotomy in teeth with signs and symptoms of irreversible pulpitis (Cushley et al., 2019). Again, it was noted that many studies did not accurately describe the preoperative diagnosis (Cushley et al., 2019) and the bulk of the evidence was in the form of single-arm studies (Qudeimat et al., 2017; Taha & Abdulkhader, 2018). Only one non-inferiority trial, that adequately described the diagnosis as indicative of irreversible pulpitis, compared RCT with pulpotomy in this case up to 5 years, and it reported the success of pulpotomy was 71% for pulpotomy and 66% for RCT (Asgary et al., 2015), The study, however, was described as having an unclear and high level of bias (Cushley et al., 2019), and the success rate of RCT for teeth with vital pulps was low compared with 83% reported previously in the literature (Kojima et al., 2004). Cushley et al. (2019) also highlighted a high rate of success clinical and radiographic success rate for coronal pulpotomy in teeth with signs and symptoms of irreversible pulpitis of 95% at 12 months, reduced to 88% at 36-months' follow-up. Although these are based on single-arm studies with no control group (Qudeimat et al., 2017; Taha & Abdulkhader, 2018; Taha et al., 2017), they do compare favourably with the outcome of RCT. In terms of patient-reported OMs, postoperative pain in the days and weeks after treatment was also shown to be equivalent between RCT and pulpotomy (Eghbal et al., 2020). Outcome analysis of failures of pulp capping after carious exposures have highlighted a high number of early painful failures (Ballal et al., 2020), which may not be evident in root canal treated teeth, implying different failure dynamics between the VPT and RCT. Partial pulpotomy can also be effective in teeth with signs and symptoms indicative of irreversible pulpitis with success rates of 83% demonstrated at 2 years with HCSCs (Taha & Khazali, 2017), although a recent study highlighted significantly reduced success with partial pulpotomy at 1 year in the severe pulpitis group if the Wolters classification was employed (Careddu & Duncan, 2021).
In summary, although evidence over the last 10 years has indicated good success for VPT procedures in teeth with signs and symptoms indicative of reversible and irreversible pulpitis, the level of evidence for these findings is low. From the research available, it would appear that VPT has the potential to be an effective alternative to RCT for the management of carious exposure; however, more comparative long-term data are required.
Future directions
It may be stating the obvious but VPT outcome studies in the future should focus on answering central questions relevant to the management of deep caries and the exposed pulp, which as yet remain uncertain or unaddressed. These include whether non-selective removal remains the gold standard for managing deep caries and whether pulp exposure is an evidenced-based negative prognostic factor. The temptation should be resisted to produce more single-arm studies and university-based studies using specialist operators as this pragmatic nature of the study is lost, and its generalizability becomes questionable. Multi-centre practice-based studies should become the focus of clinical trials in this area as they offer better external validity. Furthermore, the way outcome is measured has to evolve with the development of a COS in Endodontics, more attention on patient-centred outcomes and identifying which clinician-centred outcomes are actually evidenced-based as being critical for tooth survival and/or patient pain and swelling needs to be confirmed.
Importance of tissue handling, VPT materials and visual inspection after carious exposure
Present status
The use of HCSCs along with antimicrobial lavage and magnification has been recommended as part of an ‘enhanced protocol’ for conservative management of the exposed pulp (Bjørndal et al., 2019; ESE, 2019), as it was highlighted that studies not employing such a protocol (Bjørndal et al., 2010, 2017) demonstrated significantly poorer results compared with those that did (Bogen et al., 2008; Marques et al., 2015). Although these recommendations (antimicrobial lavage, HCSCs and magnification) appear scientifically sound, until recently, the basis for at least antimicrobial lavage and magnification relied on weak observational rather than randomized data. Magnification has been shown to increase the outcome of non-surgical RCT (Khalighinejad et al., 2017) and improves the operator's ability to inspect and manage the damaged pulp; however, it is also much more likely to be used by private or specialist practitioners (Edwards et al., 2021b), which biases the findings of non-randomized research investigating this variable. Notably, to date, the use of magnification has not been investigated as an independent variable in studies managing pulp exposure. Indeed, operator skill and experience as well as available equipment and the nature of the practice may all be important, but are as yet untested independent variables in the outcome of VPT (ESE, 2019); work clearly needs to be done in these areas.
With regards to the need for non-selective caries removal, much has been recently made of the importance of visual inspection the pulp tissue (AAE, 2021) to assess for health, necrosis and the nature and duration of pulpal bleeding (Ricucci et al., 2019), in order to contribute to an intraoperative working diagnosis (Taha et al., 2020). With the exception of necrosis or the presence of pus, which can be identified with an operating microscope (Okamoto et al., 2021), other measures including bleeding (Matsuo et al., 1996) or blood colour are less reliable indicators of treatment outcome with a recent outcome study concluding that bleeding time was not significantly linked to failure of partial; pulpotomy after 1 year (Careddu et al., 2021). Therefore, although visualization of the exposed pulp is cited as a reason to remove all caries and expose the pulp (AAE, 2021; ESE, 2019), it is not as yet supported by strong clinical evidence. The manner in which the clinician treats the wound management either by tissue removal or lavage is critical, although the question of rinsing the wound surface has been somewhat ignored. A recent systematic review analysing the types of lavage agents used during conservative treatment of the cariously exposed pulp highlighted that the lavage agent was only randomized in two out of 27 included studies (Munir et al., 2020). Interestingly, only 14 of the studies used sodium hypochlorite as an irrigating agent with 10 using saline or water; however, more recent publications correlated positively with the use of sodium hypochlorite lavage (Munir et al., 2020), with one randomized trial of immature molars comparing sodium hypochlorite to saline after 24 months reporting no difference between the irrigants (Ozgur et al., 2017). Recently, a randomized pulp capping trial of 96 patients with mild symptoms examined the short-term influence of sodium hypochlorite and saline in postoperative pain and early failure (Ballal et al., 2020) as well as longer-term clinical outcome after 1 year (Ballal et al., 2021). Lavage with 2.5% sodium hypochlorite significantly reduced postoperative pain and early painful failures, with 12 teeth in the saline group and only one in the sodium hypochlorite group reporting pain that required RCT within the first three months (Ballal et al., 2020). After 1 year, teeth that the carious exposure wound was washed with sodium hypochlorite were significantly associated with increased success of direct pulp caps (Ballal et al., 2021). It remains to be seen whether these results would be as significant if the exposure had been accompanied by tissue removal in the form of a partial of full pulpotomy; however, the work does highlight that chemical elimination of the infectious challenge with sodium hypochlorite can have a significant effect on clinical outcomes—similar to the effect that partial (Taha & Khazali, 2017) and full pulpotomies (Simon et al., 2013), have in reducing the microbial challenge at the wound surface.
The relevance of MMP9 as an objective measure of pulpitis has been highlighted before in pulpal blood (Mente et al., 2016); however, this was taken further by Ballal et al., (2021) who normalized MMP9 level by total protein demonstrating that MMP9 had a highly significant effect on pulp survival. Furthermore, the combination of saline wound lavage and high initial MMP9/TP values resulted in low pulp survival, and effect counteracted by NaOCl (Ballal et al., 2021). Although there remains much to be done, these results offer hope for the development of MMP9 or another biomarker as a chairside measure of inflammation or as a diagnostic aid to direct treatment.
Over the last two decades, HCSCs capping agents have replaced the traditional gold-standard material calcium hydroxide, by offering superior histological (Nair et al., 2008) and clinical outcomes (Cushley et al., 2021; Mente et al., 2014), although oddly despite this, the use of calcium hydroxide remains popular amongst dentists and recent graduates in certain jurisdictions (Careddu et al., 2021; Edwards et al., 2021b). To date, although the biological response to HCSCs creates thicker mineralized bridges of higher quality than calcium hydroxide (Nair et al., 2008), the response to both is reparative in nature with the hard scar-like tissue formed that is a tubular and not considered dentine (Dammaschke et al., 2019). This may be due to the relatively non-specific action of current materials (Parirokh et al., 2018; Sangwan et al., 2013) or because wound healing in the pulp cannot recapitulate the intricate nature if odontoblast formation and maturation evident in developmental processes (Duncan et al., 2020). The reparative action of calcium hydroxide (Graham et al., 2006), HCSCs (Tomson et al., 2007) and other agents (Duncan et al., 2017) has been attributed to both dental pulp cell interaction (Loison-Robert et al., 2018) and the material-induced release of bioactive dentine matrix components from the dentine matrix that contain a range of growth factors that have individually stimulated reparative events in dental pulp cell populations (Tomson et al., 2013, 2017). In light of the improved outcomes with HCSCs, it is worth considering whether the goal of stimulating dentine–pulp regeneration is actually important and whether there is a need to improve the biological qualities of the available materials. From a patient or clinical perspective, the benefits are not immediately clear as pulp capping materials that promote the deposition of thicker, higher quality tubular dentine may have little impact on treatment outcome. However, if VPT outcomes are considered in stages with respect to the desires of patients', clinicians' and finally scientists'; then, this type of regenerative tissue response become more relevant (Diogenes et al., 2016). A scientific outcome creates a translational pathway where regeneration of a physiological pulp tissue and tubular dentine formation remains an aspiration, but that currently reparative wound-healing responses provide acceptable clinical results (Duncan et al., 2019). It would certainly be unfortunate if dentists were to consider the development of next-generation biomaterials targeted at inflammatory or reparative processes (Figure 1) surplus to requirements, as it would place dentistry out of step with our medical colleagues who have developed numerous targeted therapies from immunotherapy in rheumatoid arthritis (Klimak et al., 2021) to epigenetic therapies in cancer (Sah et al., 2021) to improve results and optimize outcomes.
Future directions
Vital pulp treatments encompasses a range of techniques that encourage natural wound-healing responses in the pulp. Although the inflammatory state of the pulp is considered the biggest contributor to success of the VPT procedure (Al-Hiyasat et al., 2006), other factors under the control of the operator, such as antimicrobial wound lavage (Ballal et al., 2021), choice of capping material (Mente et al., 2014) and use of magnification (Bjørndal et al., 2019) can also affect treatment outcome. Unfortunately, current thinking remains largely technical rather than biological, and small shifts in current practice could encourage more biologically based practice. For example, it is known that dentine is a reservoir for an array of pro-reparative growth factors, cytokines, chemokines that can positively influence the repair process (Okamoto et al., 2018) when released by EDTA or other materials (Graham et al., 2006; Smith et al., 2016; Tomson et al., 2007). Strategies to optimize release of these bioactive molecules including rinsing the dentine with EDTA (Galler et al., 2016), ultrasonic (Widbiller et al., 2017) or direct application of extracted dentine matrix components (Okamoto et al., 2018) should be encouraged and further developed for therapeutic benefit.
Other translation developments to control pulpal inflammation to promote healing should be considered. Early inflammatory defence responses generally resolve as a result of sclerosis and reactionary dentine deposition and if the balance is shifted regenerative events can be promoted (Cooper et al., 2014). More prolonged, intense inflammation may lead to a shift in the balance of events away from regeneration, and therefore, mechanisms should be developed which target inflammatory processes in the pulp such as pharmacological inhibitors (Al-Natour et al., 2021) or immunotherapy (Arora et al., 2021). Finally, the capping material should evolve to target biological processes such as specific miRNA (Kearney et al., 2018), epigenetic processes (Duncan et al., 2016), anti-oxidants (Minamikawa et al., 2011) or by direct application of growth factors (Tziafas et al., 1998), which may result in the promotion of higher quality regenerative rather than reparative responses in the dentin–pulp complex, improving scientific outcomes in the short term and potentially patients' outcomes in the long term.
CONCLUSION
Recent developments in VPT have delivered clinical outcomes similar to conventional treatment for pulpitis such as RCT. This has resulted in educational curriculum changes, pulp preservation consensus recommendations and a shift to more VPT carried out in dental practice. If the exciting opportunities presented by the recent developments in VPT are to be further realized in dental practice, scientists and clinicians must build upon the work of the last 25 years. Although that period has evidenced a host of publications in the fields of Regenerative Endodontics, Pulp Biology and VPT, there remains a distinct lack of next-generation diagnostic tools, targeted biomaterials or indeed high-quality comparative evidence examining new treatment modalities such as revitalization and full pulpotomy for teeth with signs and symptoms of irreversible pulpits. Perhaps most worryingly, despite multiple recommendations, there remains no consensus on how best to manage everyday dental situations such as deep caries or an exposed pulp, which is clearly not in the best interests of patients. The future of VPT should focus on developing and refining novel biologically based wound-healing strategies including pulp tissue management, lavage and restoration, with the overall aim of targeting pulp regeneration processes to improve outcomes. In order to develop both new solutions and evidenced-based practice, an evolving scientific understanding of regenerative responses in the dentine–pulp complex is required in order to provide robust therapeutic targets and the prioritization of well-designed clinical trials with clinically meaningful comparison groups.
ACKNOWLEDGMENT
Open access funding enabled and organized by IRel.
CONFLICT OF INTEREST
The authors deny any conflicts of interest related to this study.
AUTHOR CONTRIBUTIONS
HD involved in the first draft and final approval of the manuscript.
ETHICAL STATEMENT
The study does not need ethical approval.