Diabetes mellitus and the healing of periapical lesions in root filled teeth: a systematic review and meta-analysis
Abstract
Background
Diabetes mellitus (DM) may affect the healing and survival of root filled teeth with periapical lesions.
Aim
To systematically analyse the available clinical literature to evaluate the association between DM and the prevalence of radiolucent periapical lesions in root filled teeth. The review question was ‘Is there a difference between the root canal treatment healing outcome (in terms of presence or absence of radiolucent periapical lesions) in diabetic and non-diabetic patients?’.
Data sources
A systematic review of cross-sectional studies and prospective clinical trials was conducted according to the PRISMA checklist. The review involved a search of the electronic databases of PubMed, Scopus and EBSCO host.
Study eligibility criteria, participants and interventions
The research protocol was previously registered in the International Prospective Register of Ongoing Systematic Reviews (CRD42019130954) and included defined inclusion/exclusion criteria. The included studies were related to the root canal treatment outcome in diabetic patients in terms of periapical radiolucent lesions associated with root filled teeth.
Study appraisal and synthesis
The selected studies were critically analysed by two evaluators using the Joanna Briggs Institute Critical Appraisal tool. The pooled odds ratio (OR) was recognized as the primary outcome variable and measure of the effect for the occurrence of periapical lesions associated with root filled teeth of control and diabetic patients. The random-effects Mantel–Haenszel method was used, at a 95% confidence interval, to calculate the pooled OR. A funnel plot was created to evaluate possible sources of heterogeneity.
Results
Ten studies published between 1989 and March 2019 were selected after thorough analysis and exclusion according to the strict criteria. Seven cross-sectional studies, 1 longitudinal and 2 prospective clinical studies were included. The pooled OR was calculated by comparing 773 diabetic subjects and 1133 control subjects. The pooled OR for the observational studies and clinical studies were 1.42 and 6.36, respectively. This value signified a high prevalence of periapical lesions in root filled teeth in diabetic subjects.
Limitations
There are limited prospective clinical trials on this topic. The majority of the included studies are observational.
Conclusions and implications of key findings
The data suggest a strong connection between the presence of periapical radiolucency on root filled teeth amongst diabetics as determined by the pooled OR.
Introduction
Apical periodontitis (AP) is an inflammatory disease of pulpal origin, which affects the tissues around the root apex. Radiographically, AP is seen as a radiolucent periapical lesion associated with the root-end (Figdor 2002, Segura-Egea et al. 2012). The first line of treatment for teeth with AP is root canal treatment. When AP persists in a root filled tooth, it appears as a radiolucent periapical lesion and is categorized as a root filled tooth associated with a radiolucent periapical lesion.
Various parameters used to evaluate the success of root canal treatment outcomes include complete resolution of periapical pathosis and clinical symptoms (Vire 1997, Lazarski et al. 2001, Ng et al. 2011, Fouad & Burleson 2003). However, the presence of systemic diseases may interfere with the healing of endodontic disease (Aminoshriae et al. 2017). One of the most common systemic diseases affecting the root canal treatment outcomes is diabetes mellitus (DM). DM is broadly categorized into Type 1 (Insulin-dependent) and Type 2 (Non-Insulin-Dependent; Rees 1994, Williams & Pickup 1999). The main feature of DM is hyperglycaemia. It leads to impaired immunity by affecting the cellular functions of leucocytes, monocytes, macrophages and other systemic inflammatory markers. This predisposes to increased susceptibility towards infection, development of chronic inflammation, progressive breakdown of tissues and compromised ability for tissue repair (Delamaire et al. 1997, Iacopino 2001, Fouad & Huang 2015). The ill-effects of DM are also evident in pulpal tissues. Diabetic patients often exhibit pulp tissue with limited dental collateral circulation and diminished immune response (Lima et al. 2013). It has been reported that DM negatively affects the healing outcome of root filled teeth (Mindiola et al. 2006, Arya et al. 2017). Uncontrolled glucose levels in a patient with DM acts as potential modulators of endodontic disease and can be linked with an increased prevalence of periapical lesions even after root canal treatment Fouad & Burleson (2003).
In poorly controlled diabetics, there is diminished function of PMNs and delayed wound healing leading to an increased number of periapical lesions than normally expected (Fouad & Burleson 2003, Segura-Egea et al. 2012, Nagendrababu et al. 2020). Bender et al. (1963) studied the effect of DM on periapical health of root filled teeth in a series of 33 patients. This was followed by Cheraskin & Ringsdorf (1968) who found that patients with lower blood sugar levels had a greater reduction in AP size than the high blood sugar level group over 30 weeks follow-up. Previously published literature suggests that there appears to be biological evidence suggesting a relation between DM and the occurrence of periapical lesions in root canal treated teeth (Segura-Egea et al. 2005, Marotta et al. 2012, Marques-Ferreira et al. 2014).
The healing of periapical tissue is a time-dependent continuous process that is difficult to evaluate through a cross-sectional study. In the past, two systematic reviews have evaluated the effect of DM on the root canal treatment outcome (Segura-Egea et al. 2016, Aminoshriae et al. 2017). These reviews were based on observational cohort and cross-sectional studies. As stated before, a good method for evaluating the healing of tissues is to conduct prospective randomized clinical trials. Since the publication of the systematic reviews (Segura-Egea et al. 2016, Aminoshriae et al. 2017), two prospective clinical trials have been reported (Rudranaik et al. 2016, Arya et al. 2017), which further strengthen the analysis of the effect of diabetes on periapical healing. The present review takes into account all the recent research on the possible correlation between DM and root canal treatment outcome and aimed to conduct a systematic review and meta-analysis of prospective clinical studies along with an evaluation of data from cross-sectional studies to evaluate the impact of DM on root canal treatment outcome, assessed by the prevalence or absence of radiolucent periapical lesions.
Materials and Methods
The protocol of the systemic review was framed using the established PRISMA checklist (Moher et al. 2009). The protocol was registered on PROSPERO (CRD42019130954). The review question was formulated using the PICO framework of systematic review defining the population, intervention, comparison and outcome. The formulated PICO was ‘is there a difference between the root canal treatment healing outcome (in terms of presence or absence of radiolucent periapical lesions) in diabetic and non-diabetic patients?’
Literature search strategy
The literature search was based on the following databases. A MEDLINE/PubMed, Scopus, EBSCO host search was performed. The systematic search was performed separately by three examiners (A.G., V.A., N.M.) in March 2019. MeSH (Medical Subject Headings – https://www.ncbi.nml.nih.gov/mesh) terms were used together with the Boolean operators ‘AND’ and ‘OR’ to build a search string of keywords (Table 1). The collected data were manually searched for the identification and exclusion of duplicate.
| Database | Search strategy (March 2019) | n |
|---|---|---|
| PubMed | (‘Diabetes Mellitus’ [MeSH Terms] OR ‘Diabetes Mellitus’ [All fields] OR ‘Hyperglycemia’ [All fields]) AND ‘Root Canal Treatment’ [All fields] OR ‘Endodontics’ [All fields] OR ‘Periapical diseases’ [All fields] OR ‘Periradicular diseases’ [All fields] OR ‘Endodontic Treatment’ [All fields] OR ‘Endodontic Treatment Outcome’ [All Fields]) | 1791 |
| SCOPUS | (‘Diabetes Mellitus’ [MeSH Terms] OR (‘Diabetes Mellitus’ [All fields] OR ‘Hyperglycemia’ [All fields]) AND ‘Root Canal Treatment’ [All fields] OR ‘Endodontics’ [All fields] OR ‘Periapical diseases’ [All fields] OR ‘Periradicular diseases’ [All fields] OR ‘Endodontic Treatment’ [All fields] OR ‘Endodontic Treatment Outcome’ [All Fields]) | 298 |
| EBSCOHost | (‘Diabetes Mellitus’ [MeSH Terms] OR ‘Diabetes Mellitus’ [All fields] OR ‘Hyperglycemia’ [All fields]) AND ‘Root Canal Treatment’ [All fields] OR ‘Endodontics’ [All fields] OR ‘Periapical diseases’ [All fields] OR ‘Periradicular diseases’ [All fields] OR ‘Endodontic Treatment’ [All fields] OR ‘Endodontic Treatment Outcome’ [All Fields]) | 563 |
Inclusion criteria
- all studies published from 1960 to March 2019
- clinical trials, case–control, cross-sectional, cohort, longitudinal published in the English language
- studies involving adult human diabetic and non-diabetic patients
- studies including root filled teeth
- studies in which the periapical status of root filled teeth was radiographically assessed
Exclusion criteria
- nature of the study: case series, culture laboratory studies, animal studies
- studies without a control group
- studies without radiographic assessment
- studies on patients below 14 years of age
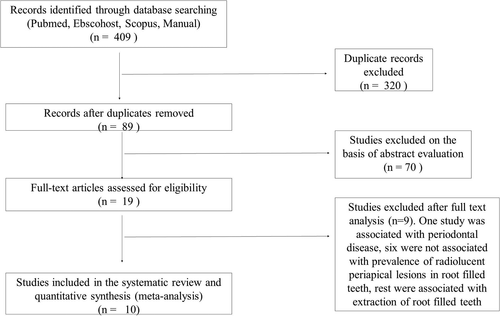
From the database search, the relevant articles were hand-searched by two authors (A.G., N.M.). The bibliography of relevant papers and review articles were also screened to extract relevant data. Finally, the data were framed in the form of PRISMA Flow chart presented as Fig. 1.
Quality assessment and data extraction
Two examiners (A.G. and V.A.) extracted the data and analysed each study for the following parameters: author (year)/country, journal, language, age group, design of the study, sample size, diagnostic criteria, root canal treatment outcome, risk of bias and the evidence level determined according to the guidelines given by National Services Scotland (Harbour & Miller 2001). Any disagreements between the two authors (A.G., V.A.) were solved by the third author (N.M). The risk of bias assessment was undertaken using the checklist given by Joanna Briggs institute critical appraisal checklist (The Joanna Briggs Institute 2014). For applying risk of bias, seven criteria were used for observational/cross-sectional studies and 10 criteria were used for prospective clinical trials. Two evaluators (V.A., A.G.) independently applied the risk of bias for all the studies, followed by a discussion of each point. Any disagreement was solved by the third examiner (N.M.) to reach a final consensus.
Outcome variable and statistical analysis
The pooled odds ratio (OR) was recognized as the primary outcome variable and measure of the effect for the occurrence of the radiolucent periapical lesion in root filled teeth of control and diabetic patients. The random-effects Mantel–Haenszel method was used, at a 95% confidence interval, to calculate the pooled OR, and is illustrated by forest plots. To test for the statistical heterogeneity amongst the individual studies, τ2 values along with chi-square and the I2 test were evaluated. It should be noted that statistical heterogeneity should not be confused with clinical heterogeneity. Since all the studies were conducted at different centres, clinical heterogeneity was assumed, and accordingly, the random-effects model was employed. Funnel plots were generated to assess the publication bias. A P-value of less than 5% was considered significant, and the meta-analysis was carried out with the RevMan 5.3 software (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration 2014).
Results
The search strategy is described in Fig. 1. A total of 409 relevant articles were identified via the search of electronic databases and manual searches. Duplicate articles were excluded. After the exclusion of duplicates, 89 articles were screened for abstract evaluation. Ten articles, fulfilling the inclusion criteria, were included in the systematic review and meta-analysis. In the excluded articles dealing with DM and healing, one article was associated with periodontal disease (Mohamed et al. 2012), five articles were not associated with the prevalence of root filled teeth associated with a radiolucent periapical lesion (Ueta et al. 1997, Doyle et al. 2007, Ilgüy et al. 2007, Iqbal & Kim 2008, Lin et al. 2014), and three were related with the extraction of root filled teeth in diabetic and non-diabetic patients (Mindiola et al. 2006, Ng et al. 2011, Wang et al. 2011).
Study characteristics
In the final analysis, ten studies were involved. All studies related to the root canal treatment outcome in diabetic patients in terms of radiolucent periapical lesions associated with root filled teeth (Table 2; Falk et al. 1989, Fouad & Burleson 2003, Britto et al. 2003, Segura-Egea et al. 2005, López-López et al. 2011, Marotta et al. 2012, Marques-Ferreira et al. 2014, Rudranaik et al. 2016, Arya et al. 2017, Smadi 2017).
| Authors | Year and journal of publication | Design of the study | No. of subjects and group-wise division | Diagnostic criteria | Statistical significance of root filled tooth * radiolucent periapical lesion association | P-value |
|---|---|---|---|---|---|---|
| Falk et al. |
1989, Scand J Dent Res |
Cross-sectional study |
N = 159 Control = 77 Diabetics = 82 |
Periapical Radiograph |
Statistically non-significant overall (however, diabetic women has a significant association) |
P = 0.20 (overall) P < 0.01 |
| Fouad & Burleson. |
2003 Jada |
Retrospective longitudinal |
N = 531 Control = 459 Diabetics = 72 |
Periapical radiograph (follow-up period >2 years) |
Overall no significant association of radiolucent periapical lesion * root filled tooth of diabetics (however significant association between pre-operative radiolucent periapical lesion and diabetics) |
P = 0.42 (overall) P = 0.073 |
| Britto et al. |
2003 Oral Surg Oral Med Oral Pathol Oral Radiol Endod |
Cross-sectional study |
N = 53 Control = 23 Diabetics = 30(type 1dm = 11 Type 2dm = 19) |
Periapical radiograph Strindberg criteria [strindberg lz 1956] |
Overall no significant association (however, men with type 2dm showed statistically significant association) |
P = 0.82 (overall) P < 0.5 |
| Segura-Egea et al. |
2005 Int Endod J |
Cross-sectional study |
N = 70 Control = 38 Type2dm = 32 |
Periapical radiograph Pai score[Ørstavik et al. 1986] |
No significant association | P = 0.17 |
| Lopez |
2011 J endod |
Cross-sectional study |
N = 100 Control = 50 Diabeti = 50 |
Digital panoramic radiograph Pai score[the jbi reviewer’s manual. 2014] |
No significant association | P = 0.09 |
| Marott A et al. |
2012 J Endod |
Cross-sectional study |
N = 90 Control = 60 Diabetics = 30 |
Periapical and panoramic radiograph Strindberg criteria [strindberg lz 1956] |
No significant association | P = 0.21 |
| Marques-ferreira |
2014 Act med portuguesa |
Cross-sectional study |
N = 46 Control = 23 Diabetics = 23 |
Periapical and panoramic radiograph Pai score [Ørstavik et al. 1986] |
No significant association | P = 0.06 |
| Rudranaik |
2016 J clin exp dent |
Prospective clinical study |
N = 80 Control = 40 Diabetics = 40 |
Periapical radiograph Strindberg criteria [Strindberg 1956] |
Significant association present | P = 0.0026 |
| Suman Arya et al. |
2017 J Endod |
Prospective clinical study |
N = 60 Control = 30 Diabetic = 30 |
Periapical radiograph PAI score [Ørstavik et al. 1986] |
Significant association present | P < 0.05 |
| Smadi |
2017 J cont dent prac |
Cross-sectional study |
N = 291 Control = 146 Diabetics = 145 |
Panoramic radiograph Pai score [Ørstavik et al. 1986] |
Significant association present | P = 0.02 |
- root filled tooth * radiolucent periapical lesion root filled teeth with radiolucent periapical lesion.
Meta-analysis
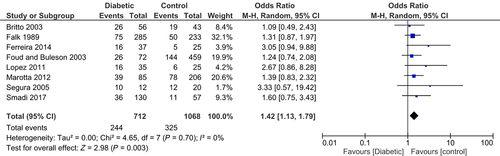
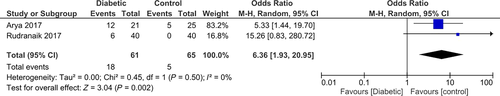
For each included study, pooled OR were calculated using the random-effect Mantel–Haenszel method (Table 3). The forest plot illustrates the ORs for each study and the overall OR calculated from the meta-analysis (Figs 2 and 3). This method provided a pooled OR = 1.42 (95% CI = 1.13 to 1.79; P < 0.05) in favour of the non-diabetic group in the observational studies. The pooled OR for prospective clinical trials was 6.36 (95% CI = 1.93 to 20.95; P < 0.05) in the favour of non-diabetic patients. Both observational (τ2 = 0, χ2 = 4.65; df = 7, P = 0.70, I2 value = 0%) and prospective studies (τ2 = 0, χ2 = 0.45; df = 1, P = 0.50, I2 = 0%) had low statistical heterogeneity, which can be attributed to the comparable confidence intervals of the included studies. Funnel plots for both observational and prospective studies were plotted to assess any publication bias. Studies with higher power and lower standard error are plotted towards the top and low powered studies are placed near the bottom (Figs 4 and 5). The funnel plots were visually symmetrical, suggesting the lack of publication bias.
| Authors | Year of publication | Diabetic subjects | Non-diabetic control subjects | Odds ratio (m-h, random, 95% CI) |
|---|---|---|---|---|
| Falk et al. | 1989 |
Events = 75 Total = 285 |
Events = 50 Total = 233 |
1.31 (0.87,1.97) |
| Britto et al. | 2003 |
Events = 26 Total = 56 |
Events = 19 Total = 43 |
1.09 (0.49,2.43) |
| Fouad & Burleson | 2003 |
Events = 26 Total = 72 |
Events = 144 Total = 459 |
1.24 (0.74,2.08) |
| Segura et al. | 2005 |
Events = 10 Total = 12 |
Events = 12 Total = 20 |
3.33 (0.57,19.42) |
| Lopez et al. | 2011 |
Events = 16 Total = 35 |
Events = 6 Total = 25 |
2.67 (0.86,8.28) |
| Marotta et al. | 2012 |
Events = 39 Total = 85 |
Events = 78 Total = 206 |
1.39 (0.83,2.32) |
| Rudranaik et al. | 2016 |
Events = 6 Total = 40 |
Events = 0 Total = 40 |
15.26 (0.83, 280.72) |
| Smadi et a. | 2017 |
Events = 36 Total = 130 |
Events = 11 Total = 57 |
1.60 (0.75,3.43) |
| Suman Arya et al. | 2017 |
Events = 12 Total = 21 |
Events = 5 Total = 25 |
5.33 (1.44,19.70) |
| Total (95% CI) | Diabetic subjects = 773 | Control subjects = 1133 |
Odds ratio 1.56(1.25,1.95) |
- OR, Odds Ratio.
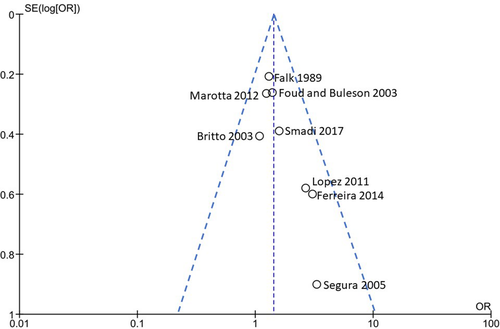
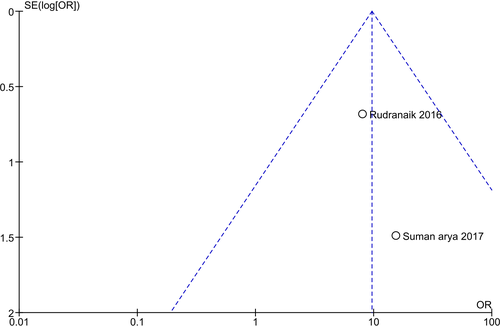
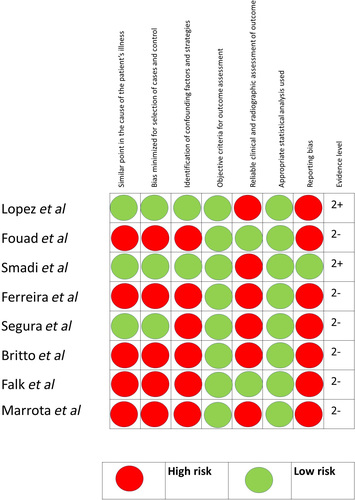
Risk of bias
Out of the ten studies, only three have a low risk of bias (Rudranaik et al. 2016, Arya et al. 2017, Smadi 2017), one study has moderate (López-López et al. 2011), and the remaining six studies had a high risk of bias (Fouad & Burleson 2003, Segura-Egea et al. 2005, Marotta et al. 2012, Marques-Ferreira et al. 2014, Figs 6 and 7). For each study, the evidence level was determined by following the guidelines given by National Services Scotland (Harbour & Miller 2001; Figs 6 and 7). Four studies had evidence level of 2+ (López-López et al. 2011, Rudranaik et al. 2016, Arya et al. 2017, Smadi 2017), and the remaining six studies had evidence level of 2- (Falk 1989, Harbour & Miller 2001, Britto et al. 2003, Fouad & Burleson 2003, Segura-Egea et al. 2005, Marotta et al. 2012, Marques-Ferreira et al. 2014).

Interpretation of individual studies
Arya et al. (2017) compared root canal treatment healing in Type 2 diabetics and non-diabetics in their prospective clinical study that included 46 teeth with a 12-month follow-up period. The diabetic group was associated with a lower rate of healing (12 out of 21 were healed) as compared to non-diabetic group (20 out of 25 were healed; OR = 5.33, 95% CI = 1.44 to 19.70).
A similar perspective clinical study was reported by Rudranaik et al. (2016) involving 80 patients divided into two groups: control and patients with Type 2 DM. The pre-operative assessment revealed more acute lesions with pain in the control and more chronic lesions with the presence of sinus tract and apical tenderness in the diabetic group. Single visit root canal treatment was provided, and post-operative healing was evaluated after 1, 2 weeks, 1, 2, 6 months and 1 year. Six patients out of 40 in the diabetic group were reported as ‘failed’ compared to zero ‘failed’ cases out of 40 in the control group (OR = 15.26, 95% CI = 0.83 to 30.13). Since the number of events/failure was ‘zero’ in the non-diabetic group, a value of 0.5 was added in each group to achieve meaningful results (Deeks et al. 2011).
Smadi (2017) conducted a cross-sectional study evaluating the periapical status in patients with DM and non-diabetic patients. Diabetic patients had a higher prevalence of apical periodontitis than non-diabetics (OR = 1.60, 95% CI = 0.75–3.43, P = 0.02). Moreover, the diabetic group had more root filled teeth as compared to the non-diabetic group.
Fouad & Burleson (2003), in a retrospective longitudinal study, found a disparity in the number of radiolucent periapical lesions in patients with diabetes and non-diabetics. It should be noted that the difference was not statistically significant (OR = 1.24, 95% CI = 0.74–2.08, P = 0.42). However, when diabetic patients with pre-operative lesions were compared to controls, there was a significant difference in the occurrence of the radiolucent periapical lesion in root filled teeth (P = 0.0073).
Falk (1989) studied the frequency of root filled tooth with radiolucent periapical lesions and found that chronic diabetics had a greater frequency of such lesions as compared to non-diabetic patients. The OR were not statistically significant (OR = 1.31, 95% CI = 0.87–1.97, P = 0.20). However, the frequency of root filled teeth with radiolucent periapical lesions in women suffering from diabetes was significantly more than women in the control group (P < 0.01).
Britto et al. (2003) studied the periapical condition in diabetic vs. control patients. There was no significant difference found in the percentage of root filled teeth with radiolucent periapical lesions between controls and diabetics (OR = 1.09, 95% CL = 0.49–2.43, P = 0.82). Furthermore, men with type 2 DM had significantly more chances of residual radiolucent periapical lesions in their root filled teeth (P < 0.05). This investigation revealed a greater occurrence of radiolucent periapical lesions, with radiolucent periapical lesions present in one or more teeth in 97% of diabetics and 87% of control subjects.
Segura-Egea et al. (2005) studied the periapical condition of 70 subjects out of which 38 were in the control group and 32 were diabetics. The number of root filled teeth in the diabetic and control group was 12 and 20, respectively. Amongst the diabetic group 10 out of 12 (83%) patients had radiolucent periapical lesions as compared to 12 out of 20 (60%) in the control group (OR = 3.33, 95% CI = 0.57–19.42, P = 0.17).
López-López et al. (2011) investigated the prevalence of root filled teeth with radiolucent periapical lesions in well-controlled diabetics and compared it with control subjects. 46% of diabetics had root filled teeth with radiolucent periapical lesions compared to only 24% in the control group; however, the difference was not statistically significant (P = 0.09; OR = 2.67, 95% CI = 0.86, 8.28).
A cross-sectional study by Marotta et al. (2012) reported that radiolucent periapical lesions occurred more commonly in untreated teeth in diabetic patients (10%) than in non-diabetics (7%) (OR = 1.39, 95% CL = 0.83–2.32). However, the difference in the prevalence of radiolucent periapical lesion associated with root filled teeth in diabetics (46%) and control subjects (38%) was not significant (P = 0.21).
Finally, Marques-Ferreira et al. (2014) studied the success rate of root filled teeth in 46 patients divided equally into two groups, healthy control subjects and diabetic subjects. No significant differences between both groups in the prevalence of root filled teeth with radiolucent periapical lesions were demonstrated (OR = 3.05, 95% CI = 0.94–9.88, P = 0.06).
On the evaluation of an individual observational study, the ORs were statistically insignificant. However, when the data were combined, the statistical power was increased to give a significant final OR in favour of non-diabetic patients.
Discussion
Various systemic diseases, such as DM, have been reported to be associated with root canal treatment outcomes. The association between diabetic and periodontal diseases is well established (Borgnakke et al. 2013, Wang et al. 2014). However, data linked to the relationship between DM and root filled tooth * radiolucent periapical lesion are less common and are unclear. Hence, the objective of this systematic review and meta-analysis was to highlight the prevalence of periapical radiolucencies in root canal treated teeth amongst diabetic and non-diabetics patients. The present review includes ten studies, out of which seven are cross-sectional studies (Falk 1989, Britto et al. 2003, Segura-Egea et al. 2005, López-López et al. 2011, Marotta et al. 2012, Marques-Ferreira et al. 2014, Smadi 2017), one is a retrospective longitudinal study (Fouad & Burleson 2003) and two are prospective randomized clinical trials (Rudranaik et al. 2016, Arya et al. 2017).
The six cross-sectional studies (Falk 1989, Britto et al. 2003, Segura-Egea et al. 2005, López-López et al. 2011, Marotta et al. 2012, Marques-Ferreira et al. 2014) and the retrospective study (Fouad & Burleson 2003) reflect the differences in the occurrence of persistent apical periodontitis. On the other hand, one cross-sectional (Smadi 2017) and two prospective clinical studies (Rudranaik et al. 2016, Arya et al. 2017) reported the disparity between diabetics and control subjects concerning the presence of periapical pathosis. All the cross-sectional studies reported a greater percentage of root filled teeth associated with a radiolucent periapical lesion in the diabetic group but none of the studies confirmed significant difference for the prevalence of root filled tooth with periapical lesions between diabetics and control subjects (P > 0.05) except one study (Smadi 2017; P < 0.05). Furthermore, all of them possess a high to moderate risk of bias except one (Smadi 2017) that had a low risk of bias.
A similar systematic review by Segura-Egea et al. (2016) included only cross-sectional studies with an evidence level of C and D (Critical Appraisal for therapy articles 2005) without applying any risk of bias. The calculated pooled OR in their review (OR = 1.42; 95% CL = 1.11–1.80; P = 0.0058) indicated that diabetic patients have a higher prevalence of root filled teeth with radiolucent periapical lesions than controls. In the present review, pooled OR and the P-value was calculated separately for observational studies (OR = 1.42; P = 0.003) and for clinical studies (OR = 6.36; P = 0.002), and these values signified a high prevalence of periapical lesions in root filled teeth in diabetic subjects. Furthermore, the inclusion of calculating both the evidence level and risk of bias (regardless of the nature of the study) highlights the prevalence of root filled teeth associated with a radiolucent periapical lesion in diabetics more clearly that strengthens the findings of the current review. Aminoshriae et al. (2017) conducted a similar review and quoted the same cross-sectional studies with high to moderate risk of bias applied without evidence level. However, that article utilized fewer criteria for applying the risk of bias as compared to the present review. According to their review, the available scientific evidence was inconclusive to establish an association between diabetes and endodontic outcomes. In the current review, full criteria were followed to apply the risk of bias for the included studies.
With the calculation of both the risk of bias and evidence level, the additional studies included in the current review, as compared to Segura-Egea et al. (2016) and Aminoshriae et al. (2017), proved to be more reliable with dependable results that showcased increased frequency of root filled tooth * radiolucent periapical lesion in diabetic subjects. The prospective clinical studies (Rudranaik et al. 2016, Arya et al. 2017) concluded that a considerable statistical difference in the prevalence of root filled teeth with periapical lesions existed amongst diabetic and control subjects. Both studies have a low risk of bias along with a better evidence level of 2+ (Harbour & Miller 2001) and provide important data to establish the association of diabetes with the root filled tooth * radiolucent periapical lesion.
Another systematic review and meta-analysis by Cabanillas-Balsera et al. (2019) highlighted the outcome of secondary root canal treatment of patients with DM with the help of three relevant studies (Mindiola et al. 2006, Ng et al. 2011, Wang et al. 2011) through which they concluded that the presence of DM in patients increases the frequency of unretained root filled tooth.
The strength of the connection between the endodontic outcome in terms of root filled tooth * radiolucent periapical lesion and diabetes is determined by pooled OR. Pooled OR > 1 indicates a greater occurrence of root filled tooth * radiolucent periapical lesion in diabetic patients than control subjects. Pooled OR = 1 shows no association between the two variables and lastly pooled OR < 1 shows a lower prevalence of root filled teeth associated with a radiolucent periapical lesion in diabetics than control (Bland & Altman 2000). The results of the meta-analysis indicate an association between diabetics and root filled tooth associated with a radiolucent periapical lesion indicated by pooled OR significantly greater than 1. If the observational studies are evaluated individually, the OR is insignificant. However, the pooled ratio gave a significant result on the negative association between diabetes and periapical healing following root canal treatment. Since the amount of data was increased in the meta-analysis, as compared with each individual study, the statistical power of the analysis was increased leading to improved precision and validity of the estimates. Forest plot and funnel plot diagrams were used to assess the heterogeneity and publication bias of the included studies. The amount of statistical heterogeneity amongst the included study was low (I2 = 0). It should be noted that I2 is a measure of statistical heterogeneity amongst the studies. The clinical heterogeneity was high since all the studies were conducted at different centres. Accordingly, a random-effect model was chosen for the statistical analysis.
It is a proven fact that diabetes reduces tissue repair capacity due to the accumulation of advanced glycation end products (AGE'S). These products lead to a greater inflammatory response which further progresses bone resorption. Reactivation of intercellular pathways leads to an increase in pro-inflammatory cytokines (Vlassara 1997, Tanaka et al. 2013). Therefore in diabetics, the immune response and the tissue repair capacity are compromised in relation to the periapical status of root filled teeth. With increased upregulation of pro-inflammatory chemical mediators, the bone turnover rate becomes compromised leading to delayed wound healing (Delamaire et al. 1997, Fouad & Burleson 2003). Diabetes not only predisposes to chronic inflammation, but it also increases the pathogenic microflora including Fusobacterium nucleatum, Peptostreptococcus micro, and streptococcus sp. (Fouad & Burleson 2003). All the factors together contribute towards the development of AP in root filled teeth amongst diabetics. The results of a clinical study can be affected by the confounding variables. The periodontal conditions and presence of other systemic diseases can affect the healing process. Some of the included studies have taken measures to control the confounding variables. However, some important information regarding glycemic control and the presence of other systemic diseases was not available in all the studies. The majority of the included studies were cross-sectional. As stated before, the healing of bone is a continuous process. The results of cross-sectional studies should be evaluated with care. Moreover, the high risk of bias amongst most of the observational studies reduces the validity of the results. Few studies were longitudinal and prospective randomized trials (Rudranaik et al. 2016, Arya et al. 2017, Smadi 2017). These studies can provide an accurate estimate of the effect of a risk factor on healing. These studies are initial benchmarks, and more documentation is required for a conclusive statement in this regard. Taking into consideration that diabetes is the one of the most prevalent medical condition, and its presence may or may not affect the treatment outcomes, the future direction for the current review is to encourage more properly planned and designed clinical studies to further determine the contribution of diabetes, to the healing outcome of root canal treatment.
Conclusions
The meta-analysis data suggest a connection between the endodontic outcome in terms of the presence of periapical radiolucency in root filled teeth in diabetics as determined by the pooled OR. However, with the help of only two clinical studies, the conclusive statement regarding the endodontic outcome in terms of root filled teeth associated with a radiolucent periapical lesion amongst diabetics and non-diabetics cannot be made. These studies are only initial benchmarks and more documentation is required for a conclusive statement in this regard.
Conflict of interest
The authors have stated explicitly that there are no conflicts of interest in connection with this article.