Inequity in cardiovascular care in the English National Health Service (NHS): a scoping review of the literature
Abstract
There is a general understanding that socioeconomically disadvantaged people are also disadvantaged with respect to their access to NHS care. Insofar as considerable NHS funding has been targeted at deprived areas, it is important to better understand whether and why socioeconomic variations in access and utilisation exist. Exploring this question with reference to cardiovascular care, our aims were to synthesise and evaluate evidence relating to access to and/or use of English NHS services around (i) different points on the care pathway (i.e. presentation, primary management and specialist management) and (ii) different dimensions of inequality (socioeconomic, age- and gender-related, ethnic or geographical). Restricting our search period from 2004 to 2016, we were concerned to examine whether, compared to earlier research, there has been a change in the focus of research examining inequalities in cardiac care and whether the pro-rich bias reported in the late 1990s and early 2000s still applies today. We conducted a scoping study drawing on Arksey & O'Malley's framework. A total of 174 studies were included in the review and appraised for methodological quality. Although, in the past decade, there has been a shift in research focus away from gender and age inequalities in access/use and towards socioeconomic status and ethnicity, evidence that deprived people are less likely to access and use cardiovascular care is very contradictory. Patterns of use appear to vary by ethnicity; South Asian populations enjoying higher access, black populations lower. By contrast, female gender and older age are consistently associated with inequity in cardiovascular care. The degree of geographical variation in access/use is also striking. Finally, evidence of inequality increases with stage on the care pathway, which may indicate that barriers to access arise from the way in which health professionals are adjudicating health needs rather than a failure to seek help in the first place.
What is known about this topic
- Evidence from the late 1990s and early 2000s suggested that access to and use of cardiovascular care in the UK was subject to a pro-rich bias.
What this paper adds
- Socioeconomic status may no longer be the most consistent determinant of inequity. Female gender, older age and black ethnicity are associated with lower than expected rates of access to and use of cardiovascular care.
- There appears to be greater inequality in access to/use of specialist cardiac services than in the primary management of cardiac disease. Help-seeking behaviour is less subject to variation.
Introduction
The inverse care law states that the availability of good medical care varies inversely with need in the population served (Tudor Hart 1971). Although the idea was first proposed over 40 years, it has proved remarkably durable. Excluding letters, viewpoints and website entries, Google Scholar reveals 15 papers published since 2010 in research journals using the term ‘inverse care law’ in the title alone. While Tudor Hart's thesis was that working-class areas were under-doctored with respect to general practitioners (GPs), the term is now applied beyond primary care. Moreover, most accounts of inverse care no longer focus solely on issues of service availability but, rather, on a broader agenda covering utilisation, quality and outcomes. The central assumption remains, however, that inverse care links to socioeconomic disadvantage, threatening the core UK NHS principle of healthcare equity. This scoping review considers whether the existing evidence base supports the socioeconomic underpinning of inverse care. We ask whether and why Tudor Hart's ‘law’ continues to be seen as defining feature of the NHS, focusing in particular on access to and use of services for cardiovascular disease (heart and stroke).
The rationale for our review is twofold. First, relatively few reviews examining variations in access to specifically NHS care have been published in the past decade (Dixon et al. 2007, Goddard 2008, Quatromoni & Jones 2008, Appleby et al. 2011, Boeckxstaens et al. 2011) and none in recent years. Second, considerable policy effort and financial resource have been targeted at addressing socioeconomic inequity in health and access to healthcare (Asthana et al. 2012). Care commissioners and providers serving deprived populations have received and spent significantly higher NHS allocations than their more advantaged counterparts. This raises the question of whether the NHS has become more equitable.
Background
Variations in access by clinical condition
Inverse care has been shown to characterise some conditions, but not others. This may reflect differences in the distribution of clinical need. For example, while the crude prevalence of degenerative physical diseases such as cancer and coronary heart disease (CHD) tends to be higher in older populations (which, in England, tend to be more affluent), mental health problems are strongly associated with low socioeconomic status (SES) and co-morbidity with physical health problems (Barnett et al., 2012; Lawson et al. 2013, Mujica-Mota et al. 2015). The UK Royal College of General Practitioners (RCGP) has been very vocal about the challenges of working at the ‘deep end’ where patients suffering from physical, emotional, psychological, financial and social problems, including problems related to substance misuse, present additional demands on primary care (RCGP Scotland, 2010; RCGP, 2013). Given the level of demand, it is argued that there is a mismatch between need and resource, GPs having insufficient time to get to the bottom of their patients’ problems. Thus, the suggestion is that, notwithstanding a positive targeting of resources, highly deprived populations have complex and demanding health service needs which are not being met by available resources.
Analysis using condition-specific Quality and Outcomes Framework (QOF) data to establish the relationship between use and need suggests that, for some conditions, such as chronic obstructive pulmonary disease and mental health, GPs in deprived areas do indeed manage much higher workloads than in affluent areas (Asthana & Gibson 2008). However, for other conditions, including cardiovascular disease and asthma, no significant differences were found, while with respect to cancer, the pattern appeared to be reversed. Acknowledging concerns that there may be socioeconomic variations in the rates at which GPs diagnose and record true levels of disease (Guthrie et al. 2006), it remains the case that casemix varies between general practices and that this will have a bearing on the relationship between need and access.
Against this background, we focus our review on care for cardiovascular diseases. This has been a particular focus for researchers seeking to investigate whether there is a pro-rich bias in the NHS. It thus lends itself to the more detailed thematic analysis that is required to throw light on the factors that give rise to variations in access and use relative to need. It is, moreover, a specialty that has provided the strongest evidence base of inverse care (Goddard and Smith, 1998; Dixon et al. 2007). In the late 1990s and early 2000s, a series of studies investigated whether rates of invasive coronary procedures (ICPs) were lower than expected among patients in socioeconomically deprived groups (Black et al. 1996, Payne & Saul 1997, MacLeod et al. 1999, Manson-Siddle & Robinson 1998, 1999, Pell et al., 2000; Hippisley-Cox & Pringle 2000, Langham et al. 2003, Jones et al. 2004, Britton et al. 2004). A review of these and some later studies concluded that British patients in low socioeconomic groups faced significant inequity in waiting times for and access to ICPs (Quatromoni & Jones 2008). Given the strong targeting of NHS resources towards deprived areas in the past decade or so, it is pertinent to ask whether evidence suggests that such inequity has since reduced.
Candidacy and adjudication
Several authors propose that a model of candidacy and adjudication should be used to conceptualise access to healthcare at different points (Dixon-Woods et al. 2005, Kovandžić et al. 2011). These concepts, which are similar to those of Bradshaw's seminal analysis of need (Bradshaw 1972), capture the idea that people must first recognise their eligibility as candidates for healthcare, then have their candidacy assessed and acted upon (adjudicated). The decision to seek help in the first place may be influenced by individual patients’ knowledge, information, their evaluation of the seriousness of their problem, their judgement of the ability of the health service to respond, psychological factors such as embarrassment or fear, and practical issues such as the need to rely on public transport or arrange childcare/time off work. These are problems that can be addressed through sensitive and targeted health service interventions (such as awareness campaigns and support for transport). However, they cannot be simply attributed to inequalities in health service availability.
Once patients have gained entry to the system, the categorisation and disposal of their health needs depend to some extent on their ability to present in ways that health professionals find credible and legitimate. In turn, the way in which health professionals categorise health needs may be affected by their perceptions of patient preferences, technical eligibility and moral or social ‘deservingness’ (Dixon-Woods et al. 2005). Capacity factors (such as length of time available for consultations, availability of tests and perceptions and/or experience of poor local capacity) may also play an important role in shaping clinicians’ decisions to open up the pathway to treatment. These are important issues of concern from a policy perspective insofar as practitioner attitudes and health service capacity are within the remit of those deciding matters relating to professional practice, resource allocation and so on.
It is important to understand where on the care pathway (e.g. at presentation, diagnosis, primary management, referral, hospital management and post-discharge care) inequities in access arise, but it is also necessary to appreciate the ways in which differences in the relative mix of care may explain and indeed legitimise variation. For example, lower than expected rates of specialist interventions such as coronary artery bypass grafts (CABGs) and percutaneous transluminal coronary angioplasties (PTCAs) are usually interpreted as being indicative of poor access to appropriate care. However, an alternative explanation is that the health of populations exhibiting lower than expected rates of secondary care is being adequately managed in primary and community settings (Gibson et al. 2002). In line with this reasoning, we structure our review to identify the way in which variations in access/use occur and interact at different levels of the healthcare system.
Problems of research bias and statistical artefact
There have been suggestions that the inverse care law has come to operate as a ‘meta-narrative’ (Dixon-Woods et al. 2005). In other words, the dominant story-line about healthcare inequity is less a reflection of reality than of taken-for-granted assumptions about the consequences of socioeconomic disadvantage. These assumptions may have shaped the ways in which questions are posed, studies designed, results interpreted and papers peer reviewed (Greenhalgh et al. 2005, Wong et al. 2013). For example, due to an ‘ongoing concern to demonstrate that socioeconomically disadvantaged people are disadvantaged in their access to healthcare’ (Dixon-Woods et al. 2005, p. 88), other dimensions of inequity such as older age, childhood, gender and ethnicity may have been overlooked.
Whether this was actually the case in the years leading up to Dixon-Woods et al.'s assertion seems doubtful. In 2003, the Centre for Reviews and Dissemination published a scoping review of studies produced since 1995 that examined variations in access to cardiac services. This summarised studies with respect to the type of service, type of disease and nature of the inequality examined (CRD, 2003). The CRD review found that a larger number of studies had explored inequity with respect to age (28%) and gender (27%) than SES (23%), geography (14%) and ethnicity (8%) (our analysis). Since this period, however, there has been considerable academic and policy interest in socioeconomic disadvantage with respect to health (e.g. Graham 2004, Asthana & Halliday 2006, Marmot et al. 2010). Thus, there is a case for examining more recent publications for evidence of a rebalancing of research effort concerning inequity in health care.
It is also important to consider the methodological quality of publications because of long-standing problems quantifying the gap between needs and access to care in deprived areas. In order to examine whether levels of access or use are lower or higher than ‘expected’, it is essential to establish some measure of health service ‘need’. Some of the proxies used to model ‘need’ may have introduced socioeconomic bias, raising the question of whether reported evidence of inequity in access has been real or a matter of statistical artefact.
To date, Quatromoni and Jones (2008) offer the only review-level assessment of inequities in access to cardiovascular care (in this case invasive procedures for CHD) in the NHS that reports on the direction of inequity. Their review did not explicitly assess the methodological quality of included papers. It included several studies that, by comparing crude rates of use with age standardised measures of need, are likely to have been subject to statistical artefact by, at least partially, controlling-out age-related inequity. Furthermore, they omitted studies published during the same period that did not find strong evidence that deprived populations were significantly less likely to receive ICPs in relation to need (Ben-Shlomo & Chaturvedi 1995, Black et al. 1995, Gatrell et al. 2002, Majeed et al. 2002, Reid et al. 2002). We believe that there is a case for reviews to more explicitly acknowledge problems of research design in included studies and, more specifically the possibility of statistical artefact.
Methods
Reflecting these themes, in undertaking our review we have drawn upon the methodological framework proposed by Arksey and O'Malley (2005) and further developed by Levac et al. (2010). Our decision to undertake a scoping as opposed to systematic review reflected concerns that the stringent criteria applied to what does and does not constitute ‘high-quality’ evidence are more difficult to apply to health services research than clinical studies. We have nevertheless given explicit attention to methodological issues in the studies we review.
We focus on cardiovascular care (heart and stroke), defined as prevention, management and treatment of diseases of the heart and circulation including CHD, angina, heart attack, stroke and cardiomyopathy. We seek to investigate whether inequities in access and use differ at different stages of the pathway to care by structuring the review findings around presentation, primary management and specialist management. We also examine how recent research has approached different dimensions of inequity (age- and gender-related, socioeconomic, ethnic or geographical).
Search strategy
The search period was restricted to 2004–2016. We have not sought to examine older evidence, in part in acknowledgement of key policy changes in the NHS, not least with respect to the distribution of funding. The more recent focus also reflected our assessment, on initial scoping, of significant methodological progress in research over the past decade or so, in particular with respect to the comparison of measures of access/use and need.
Notwithstanding the onus on systematic reviewers to search international evidence, the health-system factors (including interactions between supply and demand) that give rise to variations in access are likely to be context-specific. Thus, healthcare equity is one issue that arguably lends itself to national as opposed to international analysis. Put simply, should evidence of inverse care from, e.g. the United States guide policy initiatives in the NHS, a very different healthcare system? Moreover, devolution of the NHS has resulted in significant differences in the health systems of the home countries of the UK (NAO, 2012). We have thus excluded evidence that focuses exclusively on Scotland, Wales or Northern Ireland, admitting studies on England and, when they incorporate evidence on England, on the UK as a whole.
We retrieved articles or reports that provided quantitative evidence of variations in access to and/or use of cardiovascular care. The initial sweep used the following databases: Medline, ProQuest (including Health Management, Nursing & Allied Health, Psychology Journals, Public Health) and PubMed. We found that the use of Medical Subject Headings (MESH) terms identified a limited number of studies and, moreover, omitted articles that we knew to be relevant. The decision was thus made to use free-text searching, the final list of keywords relating to setting, type of disease, access, type of service and nature of inequity (see Appendix S1). This was supplemented by backwards and forward citation tracking and hand searching of key journals. Additional databases were screened, including Applied Social Sciences Index & Abstracts (ASSIA) and Social Sciences Citation Index (Web of Science). Websites, such as the King's Fund, the York Research Database, NIHR (ETS), the Health and Social Care Information Centre (HSCIC), NHS Right Care, National Audit Office, Nuffield Trust and the Health Foundation were also searched for grey literature.
The database searches yielded 6458 published papers (see Figure 1), most of which were excluded on the basis of the title alone. Several terms were not particularly discriminative, yielding both relevant and irrelevant material. For example, references to inequality, inequity or variation apply to literature on both healthcare and health outcomes; the term ‘access’ retrieves articles on, e.g. surgical technique; while searching for literature on drugs such as beta-blockers, angiotensin converting enzyme inhibitors (ACE inhibitors) and angiotensin receptor blockers (ARBs) drugs produces research relating to circulatory and non-circulatory conditions.
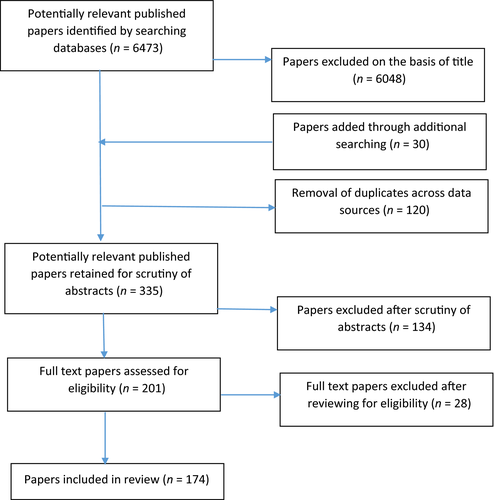
We identified 335 publications of potential interest. Of these, 134 were considered irrelevant on further screening of their abstracts. The full text of the remaining 201 studies was reviewed and a further 28 excluded on eligibility grounds. Thus, 174 studies were retained. Of these studies, all of which are included in the online appendices (Appendices S2–S4), 15 raised questions about methodological quality. With growing acknowledgement of the difficulties of establishing a baseline of expected use against which actual use can be compared (Goddard & Smith 2001, Gibson et al. 2002, Oliver & Mossialos 2004), there has been distinct improvement in the methodological quality of research in this field. However, several studies used administrative data on use (e.g. QOF recorded prevalence or admission rates) to establish denominators of need. Some, including members of our own team, strongly believe that, because all activity data will be influenced by biases in supply and demand, need estimates should be derived independently of such data (Twigg & Moon 2002, Soljak et al. 2011). Given these opinions, we have flagged rather than excluded studies (n = 15) where we had concerns about methodology quality and given the rationale for our concerns in the online tables.
Results
Overview of studies
Figure 2 summarises the results of the search by the three different stages on the care pathway (presentation, primary and specialist management) and the dimension of inequity (SES, age, gender, ethnicity and geography). ‘Inequity’ has been highlighted for studies finding lower than expected levels of access/use for people of lower SES, older people, women and non-white patients. We have included evidence on help-seeking behaviour, uptake of health checks and reported versus estimated prevalence under the heading of ‘presentation’, although recorded (QOF) detection could also be classed as evidence of primary management. We found that studies on patients accessing emergency services tended to focus on whether there was a relationship between rates of elective and unplanned admissions and quality of primary care. We have thus classed these as primary management studies. Furthermore, we have included studies on cardiovascular rehabilitation within the group on specialist management. On this basis, 25% of total studies in our review related to presentation of cardiovascular disease, 41% to primary management and 34% to specialist management.
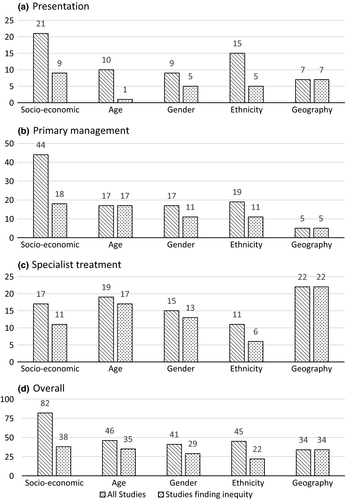
The total number of counts in the table (n = 248) is higher than the number of studies (n = 174) because some studies examined more than one dimension of inequity. 82 (33%) studies examined socioeconomic inequalities; a higher proportion than examined age (n = 46; 19%), gender (n = 41; 17%), ethnicity (n = 45; 18%) or geography (n = 34; 14%). Thus, there does appear to have been a rebalancing of research focus away from gender and age and towards SES and ethnicity relative to those studies reviewed by CRD (2003). There was no evidence of changing trends in either research effort or evidence of inequity over time.
Within the reviewed studies, older age and gender appear to be more consistently associated with poor access to and/or use of cardiovascular care; 76% and 70% of studies that had investigated age and gender variations found that older people had poorer access than younger people and women had poorer access than men. About 49% of studies examining ethnic variations found poorer access among non-white groups and 46% of studies examining variations according to SES reported evidence of poorer access among low SES groups. All of the studies that considered geography found evidence of unwarranted or unexplained variation.
Variations across the care pathway
Worryingly, the percentage of studies reporting inequity increased with stage on the care pathway; 44%, 61% and 82% of studies on presentation, primary management and specialist management respectively finding inequity in access or use. The extent to which decisions not to treat reflect clinical factors relating to capacity to benefit as opposed to inequity is not known. Taken at face-value, however, the results suggest that difficulties in recognising candidacy are less significant to inequity than processes of adjudication, which should be of policy concern.
Presentation of cardiovascular disease
We found that 21 studies focused on socioeconomic variations in the presentation of cardiovascular disease and nine of these found evidence of inverse care. The sample is small, the results contradictory and given questions about the methodological quality of some of the studies, the direction (if any) of socioeconomic inequity in presentation of CVD remains unclear. For example, using 2005–2006 QOF data, Dixon et al. (2012a,b) found that the gap between estimated [Association of Public Health Observatories (APHO)] and reported prevalence of CHD and hypertension increased with population deprivation and was higher among practices in more deprived areas. By contrast, Soljak et al. (2011) found that the pattern of observed to expected (APHO) prevalence of CHD and hypertension is less one of deprivation than of geography; observed prevalence being significantly lower than expected in London and the South East, reaching unity in the North. There is also disagreement between studies with respect to socioeconomic differences in accessing preventative checks. A comparison of NHS Health Check coverage (2011–2012) against expected (APHO) cardiovascular health need found that coverage was significantly higher in PCTs in the most deprived areas compared with the least deprived (Artac et al. 2013). Some studies (Donyai & Van den Berg 2009, Labeit et al. 2013) agree that people from less advantaged communities are more likely to access CHD risk screening programmes, while others disagree (Horgan et al. 2010, Gidlow et al. 2015, Chang et al. 2015, Cook et al. 2016).
With respect to age, youth also appears to be a factor lowering rates of presentation and uptake of health checks (Adamson et al. 2008, Dalton et al. 2011, Cook et al. 2016, Robson et al. 2016). Given the significant prevalence of overweight, obesity and associated cardiovascular risk among 45- to 64-year olds in England, the reviewed evidence suggests that preventive action could be more positively targeted at this age group.
Evidence of gender variations in presentation was mixed; five of nine studies found presentation to be poorer for women. There have been concerns about delayed help-seeking, possibly because women experience more atypical symptoms of, e.g. CHD (Albarran et al., 2007; MacInnes, 2006). However, a recent study (Brown et al. 2016) found that, after adjustment for risk, the trend towards longer symptom-to-door-times in women presenting to acute hospital care disappeared.
Several studies suggest high levels of presentation among South Asian patients (Horgan et al. 2010, Dalton et al. 2011), perhaps because of awareness about increased risk and different cultural attitudes towards masculinity and help-seeking behaviour (Galdas et al. 2007). Other studies find no ethnic differences in presentation (Patel et al. 2006, Labeit et al. 2013, Brown et al. 2016), while others find higher delays between the onset of symptoms of acute ST-elevation myocardial infarction and arrival time at hospital among South Asians (Kendall et al. 2013). Evidence of variations in presentation by black Caribbean populations is also contradictory (Horgan et al. 2010, Chang et al. 2015, Cook et al. 2016).
Primary management of cardiovascular disease
More studies (n = 44) focused on socioeconomic variations in the primary management of cardiovascular disease than any other category; 18 found evidence of inverse care (41%). Several studies note small but significant residual differences in the quality of primary care after the introduction of QOF, favouring less deprived groups (Ashworth et al. 2007, 2008, 2011, Saxena et al. 2007, Dixon et al. 2012a,b), although others suggest that socioeconomic differences have significantly narrowed over time (Doran et al. 2008, Crawley et al. 2009, and, in an evidence review, Dixon & Khachatryan 2010). Studies that have focused on prescribing (e.g. of lipid-lowering drugs or prescribing for heart failure) reported mixed results; some found no difference in prescribing rates (Patel et al. 2006, Forde et al. 2011, Mathur et al. 2011a, Hawkins et al. 2012); some found slightly higher rates in more deprived groups (Hawkins et al. 2013); and others reported lower rates (Gill et al. 2004, Shah et al. 2008, Dalton et al. 2011, Fleetcroft et al. 2014, Steel et al. 2014). While these studies vary with respect to setting, there is no obvious methodological explanation of why their results are so inconsistent. Several studies have also looked at emergency admissions for cardiovascular disease and proposed that the lack of association between quality scores and admission rates suggests that the quality of primary care is not a significant factor behind higher rates of admission among the socially deprived (Downing et al. 2007, Bottle et al. 2008, Purdy et al. 2011, Brettell et al. 2013), although there is some evidence that small practice size may play a role in variation (Wiseman & Baker 2014).
About 65% (11/17) of studies examining gender variations in primary management of CVD found that women were disadvantaged. Some studies suggest that men are significantly more likely than women to undergo detailed risk factor assessment for cardiovascular disease (Bartys et al. 2005, Crilly et al. 2007), even when doctors are presented with identical symptoms (Arber et al. 2006, Adams et al. 2008, Bönte et al. 2008), although Laverty et al. (2011) noted that men are less likely than women to receive blood pressure monitoring, a gender gap that seems to be increasing over time. Several studies suggest that prescribing rates for cardiovascular disease are consistently lower for women (de Lusignan et al. 2006, Crilly et al. 2007, Shah et al. 2008, Raine et al., 2009, Hardoon et al. 2011, Mathur et al. 2011a,b). However, others find no differences by sex (Patel et al. 2006, DeWilde et al. 2008, Sheppard et al. 2012).
More than half (58%) of studies of primary management by ethnicity also report evidence of inequity. Two studies in Wandsworth noted ethnic variations in blood pressure control (Laverty et al. 2011, Lee et al. 2011). By contrast, studies based in Lambeth find that blood pressure monitoring and prescribing is as good, if not better, for black patients compared to white patients (Schofield et al. 2011, Barrera et al. 2014). Across England as a whole, Ashworth et al. (2008) found that practices performing less well in terms of blood pressure monitoring were those with higher proportions of black residents or black British residents in the local population. Mathur et al. (2011a,b) similarly noted lower levels of prescribing among black African/Caribbean patients. Against this, several studies suggest that the quality of cardiovascular care is higher among South Asian than white populations (Britton et al. 2004, Millet et al. 2008, Mathur et al. 2011a,b), suggesting the need for research studies to distinguish between ethnic groups.
There is consistent evidence that older people are treated differently to those under 65 years. In addition to several studies suggesting that prescribing levels are lower than expected (Lawlor et al. 2004, Gill et al. 2004, Ramsay et al. 2005, 2007, de Lusignan et al. 2006, Patel et al. 2006, Harries et al., 2007; Shah et al. 2008, Mathur et al. 2011a,b, Sheppard et al. 2012, Fleetcroft et al. 2014), there is some evidence that this group are less likely to be given diagnostic tests and to be referred to a cardiologist (Hippisley-Cox et al. 2005; Harries et al., 2007).
Specialist management of cardiovascular disease
Overall, 69 of the 84 studies examining variations in access to and/or use of specialist care reported evidence of inequity (82%). A number of studies confirmed review evidence (Quatromoni & Jones 2008) that deprived patients face significant inequalities in waiting times for and access to cardiac procedures (Morris et al. 2005, Sekhri et al. 2008, 2012, West et al. 2011, Vallejo-Torres & Morris 2013), although others find no evidence that low social position is associated with lower use (Britton et al. 2004, Jones et al. 2004, McComb et al. 2009, Cookson et al. 2012). Evidence of socioeconomic inequity with respect to access to acute stroke care was more consistent (Addo et al. 2011, Lazzarino et al., 2011; Chen et al., 2014).
Evidence of gender and age variations in specialist management is strong and consistent. Women are significantly less likely to receive CABGs and PCTAs (Shaw et al. 2004, Quaas et al. 2004, Weisz et al. 2004, Daly et al. 2006, Sekhri et al. 2008, Zaman et al. 2008); have longer door-to-balloon times for primary percutaneous coronary intervention (West et al. 2011); and incur lower costs compared to men with stable coronary artery disease (Walker et al. 2016). Gender disparities have also been noted in interventions for acute coronary syndromes (Jibran et al. 2010) and heart failure (Nicol et al. 2008). Use of cardiovascular rehabilitation has been found to be higher among men than women (Beswick et al. 2004, Raine et al. 2004, Harrison & Wardle 2005). Older patients are also found to have lower rates of access to/use of revascularisation (Shaw et al. 2004, Quaas et al. 2004, Morris et al. 2005, Collinson et al., 2005; Harries et al., 2007; Sekhri et al. 2008, West et al. 2011, Gale et al. 2012, Zaman et al. 2014, Hall et al. 2016); cardiovascular rehabilitation (Beswick et al. 2004, Harrison & Wardle 2005); and stroke care (Rudd et al. 2007, Kee et al. 2009, Addo et al. 2011; Lazzarino et al., 2011).
With some exceptions (Zaman et al. 2008, Chauhan, 2010), most studies suggest that South Asians have high levels of access to specialist cardiac care (Britton et al. 2004, Jones et al. 2004, 2012, Ben-Shlomo et al. 2008, Sekhri et al. 2012). Evidence on access for black patients is more mixed, some studies suggested lower than expected rates of specialist use than expected (Mindell et al. 2008a); others higher (Addo et al. 2011).
Discussion
Over the past decade, there appears to have been a shift in research focus away from gender and demographic variations in access and use and towards SES-related variations. This is in spite of the evidence that female sex and older age are more consistently associated with healthcare inequity than SES. Women were found to delay help-seeking for longer than men and to be less likely to undergo detailed risk factor assessment for cardiovascular disease, even when doctors were presented with identical symptoms. While evidence of gender differences in prescribing is more mixed, evidence of gender inequity in specialist interventions was strong and consistent. These findings suggest the need to improve access and quality of care for women at all levels of the healthcare system. Even with recent improvements in diagnostic techniques (Shah et al. 2015), inequities for women with heart disease are unlikely to be addressed without changes in the way that decisions are made with respect to disease management and treatment.
Similarly, older people are reported to have had poorer access to cardiovascular care than younger people. In this case, there is little evidence that variations in initial presentation play a significant role in differential treatment. The results are discouraging because while some of the non-clinical influences on clinical decision-making (such as patients’ frailty, co-morbidity and own preferences) may provide legitimate reasons for non-intervention, the development of less invasive cardiovascular procedures has transformed quality of life outcomes for the oldest old (Alexander et al. 2007, Dodson & Maurer 2011). Against this background, clearer guidelines could be made available (for both clinicians and patients) about optimal treatment strategies for older age groups.
The reviewed evidence on socioeconomic and ethnic inequities is more mixed. The strongest evidence of ‘inverse care’ relates to specialist management, whereas the results are inconsistent for primary management and presentation. With respect to ethnicity, the reviewed evidence suggests that patterns of use vary between South Asian and black populations. The former appears to have higher levels of presentation and better access to primary and secondary management than other ethnic groups, including white groups, while black populations have lower rates of use than expected. The results of this research suggest the need for a more nuanced approach in which ‘non-white’ groups are differentiated. Further investigation into whether differences the clinical management of disease between different ethnic groups reflect cultural, economic or health service factors.
Finally, we note that inequity varies by stage on the care pathway, being highest with respect to specialist treatment (82% of studies). This is of particular concern because it suggests that an important source of inequity arises from the way in which health professionals are adjudicating health needs rather than a failure to seek help in the first place.
Conclusion
This scoping review suggests that, in the case of cardiovascular care, the meta-narrative of inverse care – that inequity of access is largely a problem for socioeconomically disadvantaged populations – masks the real complexity in patterns of access and use. We found consistent evidence that female sex and older age are associated with lower levels of use relative to need; and there appear to be continuing ethnic differentials. We do of course acknowledge that age, sex and ethnicity can and do interact with socioeconomic disadvantage.
We also note that the percentage of studies reporting inequity increased with stage on the care pathway. Care should be taken in interpreting these results, first because significantly fewer studies have looked at presentation than primary and specialist management, second because it is difficult to distinguish between legitimate variation (where patients with ostensibly similar diagnoses require different levels of treatment) and inappropriate processes of adjudication by clinical professionals. It is also important to note that evidence on access to and use of cardiovascular care cannot be generalised to the NHS as a whole. The possibility that inequity is greater within more specialised parts of the health service is nevertheless intriguing.