Delivering healthcare services to children with cerebral palsy and their families: a narrative review
Abstract
Children with cerebral palsy have complex healthcare needs and often require complex multidisciplinary care. It is important for clinicians to understand which approaches to healthcare service delivery for this population are supported in the literature and how these should be applied in clinical practice. This narrative review aims to identify and review the evidence for current approaches to healthcare service delivery for children with cerebral palsy. Databases were searched using key terms to identify relevant research articles and grey literature from December 2011 to September 2013. Search results were screened and sorted according to inclusion and exclusion criteria. Thirty-two documents were included for evaluation and their content was analysed thematically. Three current approaches to healthcare service delivery for children with cerebral palsy identified in this narrative review were family-centred care, the World Health Organisation's International Classification of Functioning, Disability and Health, and collaborative community-based primary care. However, healthcare services for children with cerebral palsy and their families are inconsistently delivered according to these approaches and the identified guidelines or standards of care for children with cerebral palsy have limited incorporation of these approaches. Future research is required to investigate how these approaches to healthcare service delivery can be integrated into clinical practices to enable clinicians to improve services for this population.
What is known about this topic
- Approaches to healthcare service delivery for children with cerebral palsy and their families have changed in recent decades.
- Dissatisfaction with care continues for parents of children with cerebral palsy.
- It is unclear which approaches to healthcare service delivery are supported by the literature, and how they are applied in clinical practice.
What this paper adds
- Approaches to healthcare service delivery for children with cerebral palsy supported in the literature are family-centred care, the World Health Organisation's International Classification of Functioning, Disability and Health, and collaborative community-based primary care.
- Clinical service delivery practices and guidelines and standards of care need improving to better reflect these approaches.
Background
Cerebral palsy is a complex neuro-developmental disorder that causes impairments of movement and posture and affects 2 in every 1000 children (Rosenbaum et al. 2006, Australian Cerebral Palsy Register 2009). In addition to movement difficulties, children with cerebral palsy may have an array of other difficulties that impact their mobility, independence in daily activities, cognition, bodily functions, behaviour, relationships and life participation (Rosenbaum, 2003). As a result, children with cerebral palsy and their families often require complex multidisciplinary care. Over the past two decades, healthcare service delivery practices for children with or at high risk of cerebral palsy have changed from a child-focused, professionally driven approach towards a family-focused, collaborative approach (Dirks & Hadders-Algra 2011). However, despite these changes, dissatisfaction with care is an ongoing problem for parents of children with cerebral palsy (McKay & Hensey 1990, Darrah et al. 2002, Irochu-Omare 2004, Reid et al. 2011). Parental dissatisfaction with care has been shown to be associated with organisational and interactive aspects of healthcare service delivery, rather than specific types of services or interventions (McKay & Hensey 1990, Darrah et al. 2002). Therefore, it is important for clinicians to understand which approaches to healthcare service delivery are supported in the literature. This narrative review aims to (i) identify and review the evidence for current approaches to healthcare service delivery for children with cerebral palsy and their families and (ii) identify current guidelines and standards of care for children with cerebral palsy that may be used in clinical practice, and evaluate these in terms of the current approaches to healthcare service delivery.
Methods
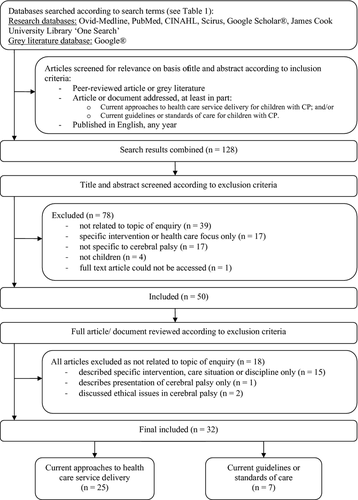
Figure 1 illustrates the literature search process. All searching, screening, assessment for eligibility and document analysis were conducted by the first author. Databases including Ovid-Medline, PubMed, CINAHL, Scirus, Google Scholar® and James Cook University Library ‘One Search’ were searched between December 2011 and September 2013 to identify literature related to approaches to healthcare service delivery for children with cerebral palsy. The Google® search engine was also used to identify guidelines or standards of care for children with cerebral palsy available as grey literature. Search terms were developed according to the PICO strategy (population, phenomenon of interest, comparison and outcome) and included ‘paediatric’, ‘pediatric’, ‘child’, ‘children’, ‘cerebral palsy’, ‘intervention’, ‘care’, ‘health care’, ‘services’, ‘health services’, ‘recommendation’, ‘standard’, ‘guideline’, ‘practice guideline’ (see Table 1). No year limits were applied to searches. Inclusion criteria (as listed in Figure 1) were used to assess articles and documents for inclusion from initial searches.
| Population | Phenomenon of interest | Comparison | Outcomes of interest |
|---|---|---|---|
| Children aged 0–16 with cerebral palsy | Different philosophies and approaches to healthcare service delivery | Comparison of philosophies and approaches to healthcare service delivery |
Parental views and experiences Professional perspectives Impacts on patient outcomes |
|
(a) ‘paediatric’ ‘pediatric’ ‘child’ ‘children’ (combined as ‘or’) AND (b) ‘cerebral palsy’ |
AND ‘intervention’ ‘care’ ‘health care’ ‘services’ ‘health services’ ‘recommendation’ ‘standard’ ‘guideline’ ‘practice guideline’ (combined as ‘or’) |
N/A | N/A |
- N/A, not applicable.
One hundred and twenty-eight articles or documents were identified through initial searching, and their abstracts were read and assessed according to exclusion criteria (as listed in Figure 1). Literature reporting only on care of adults or young people aged 16 or older was excluded from this review as adult services often use different approaches to healthcare service delivery. Literature describing healthcare approaches or practices for children with developmental disability or chronic health conditions but not specific to cerebral palsy (defined by less than 50% of the study population having cerebral palsy) was also excluded. For the guidelines and standards of care, only those that were specific to children with cerebral palsy were included for analysis.
Fifty documents were identified through abstract scanning and underwent a full-text review. During this full-text review, 18 documents were excluded as they were not related to the topic of enquiry, which was not previously apparent during abstract scanning. The final 32 included articles or documents were read in detail and reviewed in two stages. First, the content of each article relating to approaches to healthcare service delivery was critically reviewed in terms of the main focus of the article, the results or arguments made and the methodology and methods used. The content of included articles was then compared and contrasted. Recurrent themes, concepts and relationships between individual articles were identified and collated to critically summarise the evidence for approaches to healthcare service delivery for children with cerebral palsy. Secondly, the identified guidelines and standards of care for children with cerebral palsy were reviewed and analysed. The purpose, structure, content and methodology for development of each guideline were reviewed. The content was then critically reviewed in terms of the incorporation of the identified approaches to healthcare service delivery.
Results
Summary of articles and documents
Table S1 provides a summary of included articles and documents. Of the 32 articles and documents, 25 related to approaches to healthcare service delivery and 7 were guidelines or standards of care. Eleven articles related to community-based services, whereas only four articles related to care based at a hospital, with only one specifically related to inpatient care. Only 5 of the 32 documents could not be identified as peer-reviewed; these documents were guidelines of care for children with cerebral palsy (Ohio Department of Health 1995, Wilson & Cooley 2000, Koops et al. 2008, Berker & Yalçin 2010, Seattle Children's Hospital 2011).
The results of this narrative review are presented, according to the two aims, in sections below: (i) current approaches to healthcare service delivery and (ii) guidelines or standards of care for children with cerebral palsy.
Approaches to healthcare service delivery
Current approaches to healthcare service delivery for children with cerebral palsy identified in this review are (i) family-centred care, (ii) the World Health Organisation's International Classification of Functioning, Disability and Health (ICF) and (iii) collaborative community-based primary care.
Family-centred care
Family-centred care is a well-established approach to healthcare service delivery for children with cerebral palsy and their families (King et al. 2004). Numerous terms are used to describe family-centred care within the literature, including family-centred care, family-centred service and family-centred practice. This review will use the term family-centred care.
Philosophical principles: Family-centred care focuses on family strengths and promotes mutual respect and information sharing between families and healthcare providers (King et al. 2004). Family-centred care recognises and respects that parents know their child and their child's needs best, and parents hold primary responsibility for identification and prioritisation of their child's healthcare needs (King et al. 2004). Healthcare providers work in a collaborative partnership with families, involve the family in the development and evaluation of services for their child, and provide flexible services to meet the specific needs of each family (King et al. 2004). By delivering services in this way, family-centred care aims to enable and empower parents in the healthcare management of their child (King et al. 2004). Over the past two decades, principles of family-centred care have been incorporated into therapy programmes for children with or at high risk of cerebral palsy (Dirks & Hadders-Algra 2011).
Outcomes related to this approach: Delivery of care that is family-centred has been associated with positive outcomes for children with cerebral palsy and their parents and families in both hospital (Jeglinsky et al. 2011) and community-based care settings (Morgan & Tan 2010). For children, family-centred care has been associated with improved health and development and better psychosocial adjustment and functioning (King et al. 2004). For parents, family-centred care has been associated with improved emotional and psychological well-being and improved sense of personal confidence and competence (King et al. 1999, 2004). Parents who perceive that services are more family-centred are more likely to have higher satisfaction with services (King et al. 2004, Ziviani et al. 2011).
Evidence of application in clinical practice: Although the principles and benefits of family-centred care are well described, the literature reviewed also demonstrates that clinical practice does not always reflect these principles. Provision of information and education was rated poorly by parents of children with cerebral palsy when evaluating health services that aim to provide family-centred care (Jeglinsky et al. 2011). Providing information to parents can increase their hope and assist them to set realistic goals and expectations for their child with cerebral palsy (Lindstrand et al. 2002). Lack of information or knowledge causes parents to feel unprepared, vulnerable and stressed (Iversen et al. 2009).
Collaborative partnerships and shared decision-making are also demonstrated as lacking in healthcare service delivery for children with cerebral palsy. Variations between parents’ and therapists’ perceptions of the focus of therapy suggest that communication between therapists and parents may be inadequate (LaForme Fiss et al. 2012). Practitioners, parents and children have reported that they consider their role in making decisions about care as minimal, and that the other members of the partnership have greater responsibility for this task (Young et al. 2006). Children, in particular, have variable involvement in making decisions about their own healthcare and are often unequal participants in the doctor–parent–child relationship (Garth et al. 2009). In addition, programme guidelines that reflect the principles of family-centred care are lacking. Only 26 of 59 children's rehabilitation programmes in Alberta, Canada, had mission statements that reflect the principles of family-centred care and only 11 had parent representation on their advisory boards (Darrah et al. 2010). In a similar evaluation of five rehabilitation programmes in the Netherlands, no practical guidelines or protocols were available to assist rehabilitation professionals to implement family-centred care (Nijhuis et al. 2007).
Evaluation of research methodologies: Both qualitative and quantitative methods were used in the literature to investigate family-centred care. Quantitative data collection methods used included questionnaires (King et al. 1999, Karande et al. 2008, Ziviani et al. 2011, LaForme Fiss et al. 2012) and two variations of the tool, the Measure of Process of Care (MPOC); one for parents and families (MPOC-20) and the other for service providers (MPOC-SP) (King et al. 1999, Darrah et al. 2010, Jeglinsky et al. 2011, Ziviani et al. 2011). The MPOC is an evaluation tool designed to measure the extent to which a service or health professional demonstrates behaviours that are family-centred (Jeglinsky et al. 2011). Questionnaires and the MPOC allow quantification and comparison of parent and service provider's perceptions of family-centred care. However, these tools use predetermined criteria based on the theoretical principles of family-centred care to evaluate this approach to care, and therefore provide limited opportunity for exploration of relationships between different aspects of care and how that impacts parents’ experiences. One study identified in this review explored the relationships between different aspects of family-centred care and the well-being of parents of children with cerebral palsy (King et al. 1999). However, this study used predetermined parameters, so other issues not considered by the researchers could not be explored. In comparison, qualitative studies identified in this review provided more opportunity for exploration of perceptions of family-centred care using focus groups of individual interviews with children, parents or service providers. Although the perceptions of family-centred care in clinical practice were frequently investigated in the literature identified, no studies investigated how the principles of family-centred care should be implemented in clinical practice. This lack of research into best practice implementation of family-centred care makes it difficult for healthcare providers to know which behaviours or strategies ensure that the care delivered is perceived as family-centred.
International Classification of Functioning, Disability and Health
The World Health Organisation's ICF is the second approach to healthcare service delivery for children with cerebral palsy identified in the literature.
Philosophical principles: The ICF is a framework that considers the multidimensional interactions between an individual's health, functioning, participation and the social and environmental context of their life (World Health Organisation 2001). The ICF can be utilised to guide healthcare service delivery for children with cerebral palsy, supporting health professionals to provide services at any level of the ICF, all of which may be beneficial to their patients or clients (Msall & Park 2008, dos Santos et al. 2012). For example, services for a school-aged child with cerebral palsy who is having difficulty walking may be directed towards changing the impairment (e.g. muscle strength), the task or activity (e.g. using a walking aid), the child's participation (e.g. providing alternative inclusive activities for a physical education programme) or the environment (e.g. organising suitable environmental access at school), depending on how that problem is impacting the child's life. Each of these interventions has merit and can positively influence the child's well-being and functional ability.
Outcomes related to this approach: Delivery of care following the ICF framework has demonstrated benefits for children with cerebral palsy and their families. Use of the ICF to guide clinical assessment and treatment of a 12-year-old boy with cerebral palsy enabled his healthcare team to deliver interventions that were specific to the child's needs and resulted in meaningful improvements for the child and his family (Trabacca et al. 2012). Furthermore, a recent randomised controlled trial has demonstrated that therapy aimed at changing only the activity or environment was equally as effective as therapy that aimed to improve the child's impairments and performance of tasks (Law et al. 2011). Therapists have reported challenges when providing therapy in this way as it contrasts with the focus of their professional training (Darrah et al. 2011). However, this trial provides evidence to support the delivery of healthcare interventions for children with cerebral palsy and their families, which are directed only at the activity and environment level of the ICF.
Evidence of application in clinical practice: Although the ICF has been promoted as an approach to healthcare service delivery for people with disabilities, it appears that clinicians still tend to adopt a biomedical approach when working with children with cerebral palsy and their families. A study reviewing occupational therapy and physiotherapy practices for young children with cerebral palsy in Canada demonstrated that the majority of interventions described by therapists were aimed at impairment and activity, and few focused on aspects of participation such as play and socialisation (Saleh et al. 2008). In another similar study, goals identified by occupational therapists and physiotherapists for case scenarios of children with cerebral palsy focused primarily on improving activity (61%) and impairment (24%), which was in contrast to the children's parents whose goals for their child were predominantly related to social participation (Darrah et al. 2010). In other studies, parents have rated activities and participation for their child as their highest need (Buran et al. 2009, LaForme Fiss et al. 2012) and specifically commented on the importance of participation and the social environment (Reid et al. 2011).
Evaluation of research methodologies: The ICF framework was published in 2001 – before any of the included articles relating to the ICF were published. As a result, six of the ten articles relating to this approach used the ICF as a predetermined framework to evaluate clinical practices (Msall & Park 2008, Saleh et al. 2008, Darrah et al. 2010, Law et al. 2011, dos Santos et al. 2012, Trabacca et al. 2012). Only two articles did not have the ICF framework as part of the original research design (Buran et al. 2009, Reid et al. 2011). The limited research using inductive methods to support this approach to healthcare service delivery for children with cerebral palsy and their families could result in false assumptions about the applicability of this approach for this population. However, a number of included articles supported the use of the ICF as a framework for healthcare service delivery for children with cerebral palsy and their families (Buran et al. 2009, Darrah et al. 2010, LaForme Fiss et al. 2012, Trabacca et al. 2012), including one randomised controlled trial (Law et al. 2011).
Lacking in the literature identified in this review is how the ICF should be implemented in clinical practice. Although a number of articles evaluated clinicians’ performance of healthcare tasks such as goal setting (Saleh et al. 2008, Darrah et al. 2010, LaForme Fiss et al. 2012), only one article described how the ICF could be implemented in clinical practice (Darrah et al. 2011). The lack of evidence about how to apply the ICF in clinical practice might be part of the reason why implementation in clinical practices remains poor.
Collaborative, community-based primary care
Although only four articles were identified from our literature search, collaborative community-based primary care is the third approach to healthcare service delivery for children with cerebral palsy identified in this review (Cooley 2004, Lipson Aisen et al. 2011, Liptak et al. 2011, Reid et al. 2011).
Philosophical principles: Collaborative, community-based primary care is also described in the literature as the ‘medical home’ and, to some extent, aligns with the principles of family-centred care (Liptak et al. 2011). The community-based primary care approach advocates for all primary and preventative healthcare services for the child and their family to be delivered in the community by a general or specialist physician in collaboration with other health service providers (Cooley 2004, Liptak et al. 2011). All services are co-ordinated and aim to meet the needs of the child and the family.
Outcomes related to this approach: Parents of children with cerebral palsy have identified that collaborative care provided in the community contributes to more positive experiences with healthcare services and helps parents to cope (Reid et al. 2011).
Evaluation of research methodologies: The lack of research investigating collaborative community-based primary care limits the strength of evidence for this approach to healthcare service delivery for children with cerebral palsy. Of the included articles relating to collaborative community-based primary care, only one was empirical research; the other three articles were clinical reports. Further research investigating the impact of collaborative community-based primary care on children with cerebral palsy and their families is required.
Guidelines or standards of care for children with cerebral palsy
Seven guidelines or standards of care for children with cerebral palsy and their families were identified from the literature search (Ohio Department of Health 1995, Nickel & Desch 2000, Wilson & Cooley 2000, Bakheit et al. 2001, Koops et al. 2008, Berker & Yalçin 2010, Seattle Children's Hospital 2011). These consisted of three guidelines or standards developed by an individual hospital or state department of health in the USA (Ohio Department of Health 1995, Koops et al. 2008, Seattle Children's Hospital 2011), one guide published by a humanitarian organisation (Berker & Yalçin 2010), two reference documents published within physician reference books (Nickel & Desch 2000, Wilson & Cooley 2000) and one peer-reviewed journal article (Bakheit et al. 2001). Each guideline or standard of care provides both general and specific information for the care of children with cerebral palsy, with the information organised by age group (Nickel & Desch 2000, Wilson & Cooley 2000, Seattle Children's Hospital 2011), body system (Koops et al. 2008) or potential presenting problems (Ohio Department of Health 1995, Bakheit et al. 2001, Berker & Yalçin 2010).
Reflection of current approaches to healthcare service delivery
The content of the guidelines or standards of care identified in this review generally reflected a biomedical focus, with only some incorporation of the current approaches to healthcare service delivery. The healthcare considerations and interventions outlined in each of these documents primarily focus on the child's physiological impairments and functional achievements, with less focus on participation needs. Three of the guidelines or standards of care do promote participation in life situations for adolescents and young adults, such as involvement in social, recreational and leisure activities (Ohio Department of Health 1995, Nickel & Desch 2000, Seattle Children's Hospital 2011), but none considers this need for the younger child. Only two guidelines or standards of care recommended a community-based primary care approach (Ohio Department of Health 1995, Seattle Children's Hospital 2011). The needs of the family are considered in each of the guidelines or standards of care, but the extent to which the family is incorporated into the child's care varies greatly. Five of the guidelines or standards of care provided descriptions or checklists of the potential needs of the family (Ohio Department of Health 1995, Nickel & Desch 2000, Wilson & Cooley 2000, Berker & Yalçin 2010, Seattle Children's Hospital 2011). However, only three made specific mention of family participation in decision-making and development of treatment plans (Ohio Department of Health 1995, Bakheit et al. 2001, Seattle Children's Hospital 2011). As far as can be identified, only one guideline or standard of care consulted with parents during its development (Seattle Children's Hospital 2011). No other guideline or standard of care included parents or children in their development, which is in contrast to the principles of family-centred care.
Evaluation of methodologies
The methodological processes followed for the development of the guidelines and standards of care were difficult to evaluate. Only one document described the process of developing standards of care by a multidisciplinary group of practitioners based on clinical experience and published scientific evidence (Bakheit et al. 2011) was not provided. However, the extent and level of scientific evidence used to justify each of the recommendations were not provided in this published version of the document. Three of the seven guidelines and standards of care were identified as peer-reviewed, being published in reference books or a scientific journal (Nickel & Desch 2000, Wilson & Cooley 2000, Bakheit et al. 2001). However, few references, if any, are listed for each of the documents. Four of the guidelines and standards appear to have been developed or reviewed by panels of medical or multidisciplinary experts (Ohio Department of Health 1995, Koops et al. 2008, Berker & Yalçin 2010, Seattle Children's Hospital 2011). However, the processes of development of these guidelines or standards of care are not clearly described. The lack of information regarding process of development and level of scientific evidence limits the clinicians’ understanding of the relevance of each guideline or standard to their clinical practice.
Discussion
The current approaches to healthcare service delivery for children with cerebral palsy and their families identified in this narrative review are family-centred care, care delivered according to the World Health Organisation's ICF and collaborative community-based primary care. These approaches have demonstrated benefits for children with cerebral palsy, and their parents and families. However, when compared with the evidence on current clinical practices and parents’ experiences, this review demonstrates that care inconsistently reflects these approaches and inconsistently meets the needs of children with cerebral palsy and their families. Despite the emergence of these approaches as central tenets for healthcare of children with disabilities globally, their influence on changing clinical practices appears to be slower and improvements to healthcare service delivery practices for children with cerebral palsy and their families are still required. Areas for improvement include provision of information to parents; working in a collaborative partnership; and providing healthcare services across all levels of the ICF, particularly for participation and the social environment. Interestingly, these issues with healthcare service delivery are the same issues that contribute to parents’ dissatisfaction with their child's care as identified in previous research (see McKay & Hensey 1990, Darrah et al. 2002, Irochu-Omare 2004, Reid et al. 2011).
One potential contributor to the gap between theory and practice is the limited research on how these approaches to healthcare service delivery should be applied in clinical practice. This lack of research may also explain why the guidelines and standards of care for children with cerebral palsy and their families identified in this review have limited incorporation of the approaches to healthcare service delivery and limited description of how services should be delivered. Other discipline-specific treatment guidelines for children with cerebral palsy that did not fit the focus of this review also lack guidance on the approach to healthcare service delivery to be used when applying these guidelines in clinical practice (see e.g. Pennington et al. 2011, Andrew et al. 2012). This would suggest that the theoretical approaches to healthcare service delivery are not filtering down into clinical practices for children with cerebral palsy and their families. Previous literature demonstrates that parents’ dissatisfaction with healthcare services is associated with the way in which healthcare services are delivered, rather than what services are provided (see McKay & Hensey 1990, Darrah et al. 2002, Irochu-Omare 2004, Reid et al. 2011). The lack of guidance about how services should be delivered is a notable omission within the available guidelines or standards of cares. In addition, almost all the guidelines and standards of care identified in this review appear to have been developed by healthcare professionals without consultation or collaboration with children with cerebral palsy and their parents, which contrasts the principles of family-centred care. Parents’ perceptions of their child's healthcare needs may differ from those of health professionals. Furthermore, children's perceptions of their own healthcare needs may also differ from that of their parents and of health professionals. Without the input of children with cerebral palsy and their parents, the current guidelines or standards of care may not adequately reflect the actual needs of this population. If the existing guidelines or standards of care for children with cerebral palsy do not describe how to deliver healthcare services according to the current approaches and do not reflect the needs of the child and family due to the lack of child and parental input, then this may be part of the reason why parents of children with cerebral palsy continue to be dissatisfied with their child's healthcare.
Limitations
The limitations of this narrative review need to be taken into consideration when interpreting the results. First, the authors acknowledge that the literature searching process, particularly with regard to the guidelines and standards of care, was not exhaustive. For example, leading researchers, practitioners or healthcare organisations were not contacted for information available outside the search databases. In addition, this review does not identify whether there is any additional literature or guidelines or standards of care available in languages other than English, causing a potential language bias. However, despite these limitations, the literature-searching process for this narrative review enabled the collation of a comprehensive data set relating to the review topic that the authors felt reflected current understandings and was sufficient for the purposes of this review. Secondly, although the quality of the included evidence was examined and outlined, the quality of the evidence did not preclude inclusion for review and was not evaluated using formal criteria as would occur in a systematic review. This may impact the robustness of the interpretation of the evidence presented. Finally, the assumption of what constitutes a ‘family’ is somewhat stereotypical within the context of this review, which may limit the applicability of the results across alternative family configurations.
Implications for future research
This narrative review has provided understanding of healthcare service delivery approaches and practices for children with cerebral palsy and their families and can be used to inform future research. Over half of the literature identified in this review regarding approaches to healthcare service delivery related to family-centred care (15 articles), with less evidence being available on the ICF (10 articles) and collaborative community-based primary care (4 articles). Further research is required to strengthen the evidence base for these two approaches for children with cerebral palsy and their families. Additionally, only one article specifically described approaches for acute inpatient healthcare situations (Iversen et al. 2009). Although services for children with cerebral palsy and their families are often based in the community, many children with cerebral palsy will require admission to hospital and inpatient care for issues such as respiratory infections, orthopaedic procedures or acute seizure management (Jones et al. 2007). These hospital admissions can be highly stressful for children with cerebral palsy and their parents (Phua et al. 2005). Further research into approaches to care for acute healthcare situations is required. In addition, future reviews of the literature could examine approaches to healthcare service delivery and generic guidelines and standards of care for children across a number of developmental disabilities and chronic illnesses, as many conditions may share common needs. Finally, this narrative review has identified a limited integration of current approaches to healthcare service delivery for children with cerebral palsy into clinical practices and available guidelines and standards of care. Future research, potentially using a knowledge to action framework, needs to bring together evidence on (i) the effectiveness of specific health interventions; (ii) the different approaches to care; (iii) the experiences of children with cerebral palsy and their families; and (iv) the barriers and facilitators to implementation of the different approaches to care. Exploration of these interrelationships will provide knowledge and understanding to deliver improvements in healthcare experiences for children with cerebral palsy and their families.
Conclusion
Current approaches to healthcare service delivery for children with cerebral palsy in the literature are family-centred care, collaborative community-based primary care and the World Health Organisation's ICF. However, healthcare services for children with cerebral palsy and their families are not always delivered according to these approaches, and currently available guidelines or standards of care for children with cerebral palsy do not reflect these approaches. Future research is required to investigate how the different approaches to healthcare service delivery can be integrated into clinical practice to enable better delivery of healthcare services according to the principles of these approaches. In addition, guidelines or standards of care need to reflect not only what services to provide to children with cerebral palsy and their families, but importantly, how these services should be delivered. Improved delivery of healthcare services according to the current approaches to care, and the development of guidelines or standards of care in collaboration with children with cerebral palsy and their parents that reflects the current approaches, may contribute to improved healthcare experiences and, therefore, satisfaction with care within this population.
Acknowledgement
Thanks to the Mackay Health Service District for their support and research upskilling funding, which contributed to the successful completion of this narrative review.
Conflict of interest
None.