Limited sinonasal Rosai–Dorfman disease presenting as chronic sinusitis
Abstract
Aims
The sinonasal tract is a common extranodal site for Rosai–Dorfman disease (RDD). Recently, histiocytes with features of RDD were identified in the clinical setting of chronic sinusitis. This study evaluates whether this phenomenon should be considered part of the RDD spectrum or classified separately as RDD-like histiocytes.
Methods and results
We prospectively collected 13 cases showing histological features of RDD in chronic sinusitis patients and identified 14 with similar findings (3.5%) via retrospective review of 403 sinus contents over 2 years. All 27 cases displayed nodular aggregates of eosinophilic histiocytes with intermixed lymphoplasmacytic inflammation, prominent eosinophils and emperipolesis. The histiocytes were positive for S100 protein and cyclin D1 and negative for CD1a and CD207. All patients presented with severe chronic sinusitis without tumour formation or systemic symptoms. Twelve patients with follow-up (55%) required repeat sinus surgery compared with just 43 other sinusitis patients evaluated (11%); features of RDD were present in their additional specimens. Two cases that underwent targeted next-generation sequencing (20%) had oncogenic mutations in NF1 and KEAP1.
Conclusions
Overall, these findings confirm diagnostic histological and immunohistochemical features of RDD in a subset of chronic sinusitis specimens. While patients uniformly lack systemic involvement or tumefactive growth, they have a high risk of recurrent sinus disease. Although the relatively subtle nature of the findings raises consideration of separate classification, the presence of occasional oncogenic mutations and evidence of consistent MAPK/ERK pathway activation via cyclin D1 positivity suggests that this phenomenon represents a unique limited manifestation of RDD.
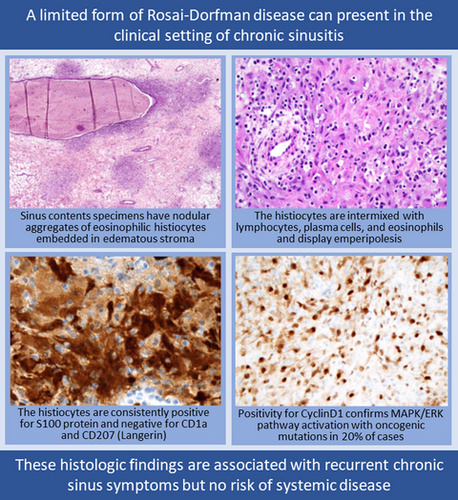
Graphical Abstract
Introduction
Rosai–Dorfman disease (RDD), also known as sinus histiocytosis with massive lymphadenopathy, is an R-group non-Langerhans cell histiocytosis with diverse clinical presentations.1, 2 While it was originally described in cervical lymph nodes, it can involve numerous nodal and extranodal sites, including viscera, skin and soft tissue.3-5 It can also present as either self-limited localised disease curable with excision or an aggressive multisite process necessitating systemic chemotherapy. Similarly, putative aetiologies of RDD are markedly heterogeneous. Recently, mitogen-activated protein kinase/extracellular signal-regulated kinase (MAPK/ERK) pathway mutations, commonly affecting MAP2K1 and KRAS, were detected in up to half of RDD, indicative of a neoplastic process.6-10 However, other cases are polyclonal and can be associated with malignancy, infections and autoimmune conditions.11, 12 Regardless of mutation status, RDD shows consistent expression of p-ERK and cyclin D1, leading to emerging consensus that it results from MAPK/ERK pathway activation via a variety of mechanisms.13-15
The sinonasal tract is one of the most common sites for extranodal RDD. Sinonasal involvement is present in 11% of RDD patients, of whom 70% also have multisite disease.16-19 Sinonasal involvement does not drive overall prognosis, although it can be associated with aggressive behaviour in systemic disease.16-18, 20 However, localised RDD also can arise in the sinonasal tract and generally has excellent outcomes after surgical excision alone.16-22 Recently, understanding of sinonasal RDD became more complicated with description of RDD-like histiocytes – a phenomenon defined by the presence of histiocyte aggregates with histological features of RDD in patients with chronic sinusitis symptoms.23 It is currently unclear whether these histiocytes truly represent a separate process or a localised manifestation of RDD. In this study, we aimed to further characterise the clinicopathological and molecular features of this phenomenon to clarify its prevalence, classification and clinical implications.
Materials and methods
PROSPECTIVE CASE SELECTION
With institutional review board approval (IRB) (Johns Hopkins Medicine IRB 00176183 and UT Southwestern IRB 112017–073), we prospectively identified 13 sinus contents specimens with histological features of RDD from the authors’ consultation files. All cases were taken from patients who presented for management of chronic sinusitis. Although nasal polyposis was allowable, patients with discrete mass lesions or infiltrative processes were excluded. As per consensus Histiocyte Society guidelines, histological features of RDD were defined by the presence of aggregates of histiocytes that (1) had abundant, glassy eosinophilic cytoplasm and (2) were positive for S100 protein and negative for CD1a.1 All available clinical and demographic information was tabulated for these cases.
RETROSPECTIVE CASE REVIEW
We also retrospectively evaluated for RDD among all sinus contents specimens removed either (1) during functional endoscopic sinus surgery for chronic sinusitis or (2) for access during endoscopic endonasal pituitary surgery over 2 years at the Johns Hopkins Hospital. Cases of malignancy, papilloma and invasive fungal sinusitis were excluded. All available histological sections were reviewed for all cases, and histological features of RDD or any other prominent histiocyte proliferation were noted. We selected a total of 25 cases with prominent histiocytes from the retrospective sinus content cohort for immunohistochemistry, including 14 with histological features of RDD and 11 with histiocyte proliferations in other patterns such as granulomas. Clinical history and demographic information were obtained from the electronic medical record for all chronic sinusitis patients. All previous or subsequent sinus specimens from these patients were also re-reviewed.
IMMUNOHISTOCHEMISTRY
Immunohistochemistry was performed using mouse monoclonal antibodies for S100 protein (clone 4C4.9; prediluted; Ventana Medical Systems, Tucson, AZ, USA) in all 27 cases with histological features of RDD from the prospective and retrospective cohort as well as 11 other cases with prominent histiocytes from the retrospective cohort. Stains for CD1a (clone MS/220; 1:50 dilution; Leica Biosystems, Buffalo Grove, IL, USA), CD207 (Langerin; clone 12D6; 1:200 dilution; LSBio, Seattle, WA, USA) and cyclin D1 (clone SP4; prediluted; CellMarque/Sigma-Aldrich, St Louis, MO, USA) were also performed on most cases with histological features of RDD based on tissue availability. Staining was performed using Ventana BenchMark Ultra autostainers (Ventana Medical Systems), and signals were visualised using ultraView polymer detection kits (Ventana Medical Systems).
MOLECULAR TESTING
We performed targeted next-generation sequencing as described in detail elsewhere24 on 10 cases, including seven identified prospectively and three identified retrospectively. Cases with the most abundant non-decalcified tissue were selected for molecular analysis. Briefly, DNA was isolated using Qiagen AllPrep kits (Qiagen, Germantown, MD, USA), an enriched library containing all exons from > 1425 cancer-related genes was created using custom NimbleGen probes (Roche, Indianapolis, IN, USA), and sequencing was performed using a NextSeq 550 (Illumina, San Diego, CA, USA) with a median 900× target exon coverage. Variants were reviewed using the Integrated Genomics Viewer (Broad Institute, Cambridge, MA, USA) and annotated using gnomAD and dbSNP databases.
Results
CLINICAL INFORMATION
Overall, we identified 27 cases with histological features of RDD, including 13 diagnosed prospectively and 14 identified retrospectively. The 14 retrospective cases represented 3.5% of 403 sinus contents specimens removed for chronic sinusitis over 2 years. All retrospective cases were signed out as chronic or allergic sinusitis with variable description of inflammatory components, but RDD was not mentioned in any original diagnoses. All 68 sinus contents specimens from asymptomatic patients during access for endoscopic pituitary surgery had no histological evidence of RDD. As summarised in Table 1, patients with histological features of RDD included 15 women and 12 men, median age 49 years (range = 18–81 years). All patients had severe chronic pan-sinusitis refractory to medical management, including polyposis, congestion, pressure, drainage and hyposmia. Despite the presence of polyps common to chronic sinusitis, no patients demonstrated expansile or infiltrative mass lesions. Additionally, no patients displayed systemic symptoms. Among 20 patients with detailed medical history available, 10 (50%) also had asthma and five (25%) displayed Samter's triad of chronic sinusitis, asthma and aspirin sensitivity.
| Case | Age | Sex | Cohort | S100 | Additional pathological findings | Cyclin D1 | CD1a | CD207 | Mutations (VAF) | Follow-up (months) | Repeat sinus surgery |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 58 | M | Pro | Pos | None | Pos | Neg | Neg | VUS | NA | NA |
| 2 | 49 | F | Pro | Pos | None | Pos | ND | ND | ND | 6 | No |
| 3 | 35 | M | Pro | Pos | None | Pos | Neg | Neg | ND | NA | NA |
| 4 | 39 | M | Pro | Pos | None | ND | Neg | Neg | ND | 23 | Yes |
| 5 | 61 | F | Pro | Pos | None | ND | Neg | Neg | ND | NA | NA |
| 6 | 53 | M | Pro | Pos | None | ND | Neg | Neg | ND | NA | NA |
| 7 | 70 | F | Pro | Pos | None | Pos | Neg | Neg | ND | 41 | Yes |
| 8 | 57 | M | Pro | Pos | None | Pos | Neg | Neg | None | 64 | Yes |
| 9 | 75 | M | Pro | Pos | None | Pos | Neg | ND | None | 13 | No |
| 10 | 27 | M | Pro | Pos | Allergic fungal sinusitis | Pos | Neg | ND | VUS | 22 | No |
| 11 | 81 | M | Pro | Pos | None | Pos | Neg | ND | VUS | 6 | No |
| 12 | 23 | F | Pro | Pos | Allergic fungal sinusitis | Pos | ND | ND | VUS | 19 | No |
| 13 | 18 | F | Pro | Pos | Antrochoanal polyp | ND | Neg | ND | None | NA | NA |
| 14 | 22 | F | Retro | Pos | Mycetoma | Pos | Neg | Neg | ND | 60 | Yes |
| 15 | 42 | M | Retro | Pos | None | Pos | Neg | Neg | ND | 193 | Yes |
| 16 | 24 | F | Retro | Pos | None | Pos | Neg | Neg | NF1 p.R416* (19%) | 88 | No |
| 17 | 63 | M | Retro | Pos | None | Pos | Neg | Neg | ND | 303 | Yes |
| 18 | 50 | M | Retro | Pos | None | Pos | Neg | Neg | None | 77 | Yes |
| 19 | 56 | F | Retro | Pos | None | Pos | Neg | Neg | ND | 155 | Yes |
| 20 | 59 | F | Retro | Pos | None | Pos | Neg | Neg | ND | 113 | No |
| 21 | 26 | F | Retro | Pos | Allergic fungal sinusitis | Pos | Neg | Neg | ND | 146 | Yes |
| 22 | 43 | F | Retro | Pos | None | Pos | Neg | Neg | ND | 12 | No |
| 23 | 45 | F | Retro | Pos | None | Pos | Neg | Neg | ND | 4 | No |
| 24 | 50 | F | Retro | Pos | None | Pos | Neg | Neg | ND | 32 | No |
| 25 | 38 | F | Retro | Pos | None | Pos | Neg | Neg | ND | 149 | Yes |
| 26 | 36 | F | Retro | Pos | None | Pos | Neg | Neg |
KEAP1 p.R470C (5%) FBXW7 p.R399Q (10%) TP53 p. T125M (6%) |
68 | Yes |
| 27 | 58 | M | Retro | Pos | None | Pos | Neg | Neg | ND | 186 | Yes |
- NA, not available; Neg, negative; ND, not done; pos, positive; pro, prospective; Retro, retrospective; VAF, variant allele fraction; VUS, variants of uncertain significance.
HISTOLOGICAL FINDINGS
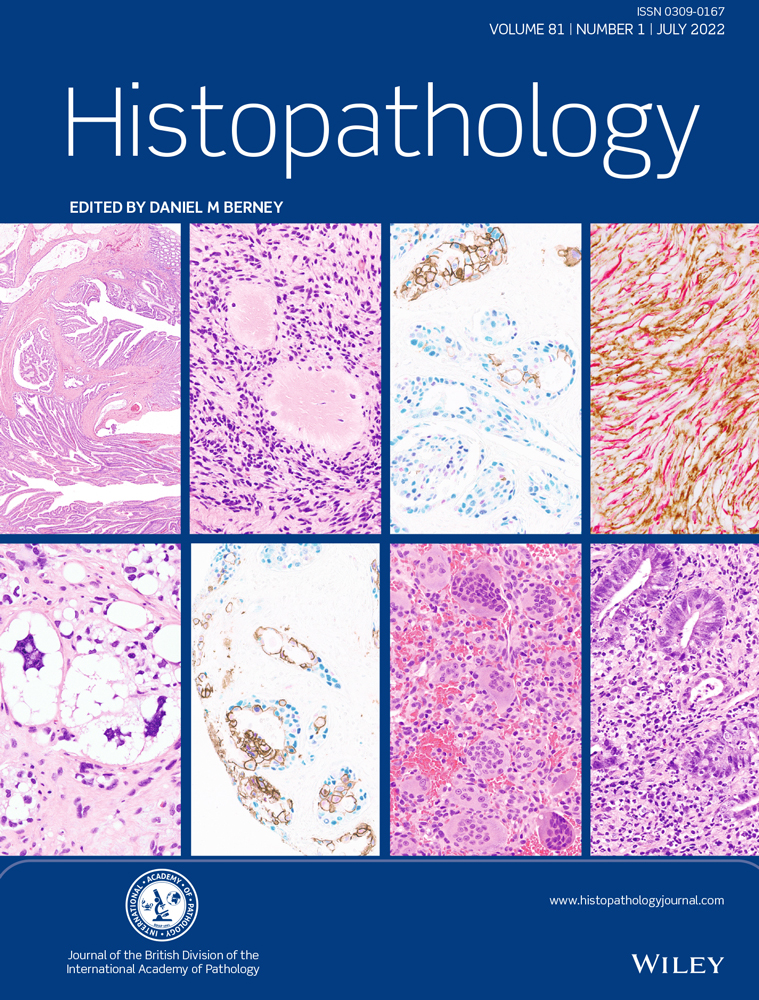
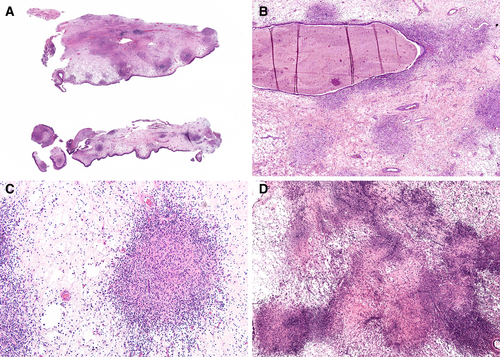
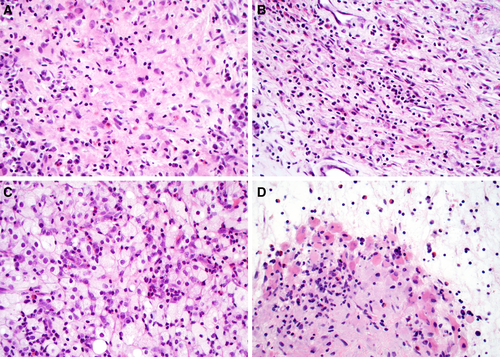
The 27 cases with histological features of RDD displayed intact sinonasal mucosa with variable polyp formation (Figure 1A). Prominent aggregates of histiocytes and lymphocytes conferred a checkerboard pattern at low power (Figure 1B). The histiocyte aggregates were largely nodular and compact with a granuloma-like appearance (Figure 1C); confluent growth was rare (Figure 1D). There was abundant oedematous stroma with scattered inflammatory cells between the histiocyte aggregates. While most histiocyte aggregates were dispersed irregularly (Figure 2A), a subset were perivascular (Figure 2B). However, no overt vasculitis or angiodestruction was seen. Other aggregates surrounded seromucinous glands (Figure 2C) or surface epithelium (Figure 2D). Histiocytes were large and epithelioid (Figure 3A), spindled (Figure 3B) or occasionally foamy (Figure 3C), with abundant eosinophilic cytoplasm and round to oval nuclei without grooves or indentations (Figure 3D). They were consistently intermixed with dense lymphocytes and plasma cells (Figure 4A). Emperipolesis was evident on haematoxylin and eosin (H&E) in most cases (Figure 4B). Most cases also showed prominent intermixed eosinophils (Figure 4C) with occasional eosinophilic emperipolesis (Figure 4D). While histiocytes themselves occupied a low volume of the tissue, numerous aggregates were scattered throughout all specimens, comprising the most notable pathological feature of these cases. Five cases had additional histological findings, including allergic fungal sinusitis in three (11%), mycetoma in one (4%) and antrochoanal polyp in one (4%).

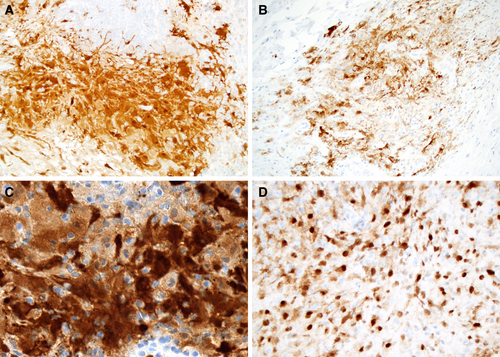
IMMUNOHISTOCHEMICAL FINDINGS
Immunohistochemical findings are summarised in Table 1. All 27 cases with histological features of RDD displayed nuclear and cytoplasmic positivity for S100 protein (100%), with diffuse (Figure 5A) to patchy staining (Figure 5B). S100 protein highlighted emperipolesis in all cases where it was not evident on H&E (Figure 5C), such that 100% ultimately had emperipolesis. All 23 cases tested were positive for cyclin D1 (100%) within histiocyte aggregates (Figure 5D). All 25 cases tested were negative for CD1a (0%) and all 21 tested were negative for CD207 (0%). The 11 cases that had prominent histiocytes but lacked histological features of RDD were negative for S100 protein expression (0%).
MOLECULAR FINDINGS
Molecular findings are summarised in Table 1. Targeted next-generation sequencing identified two cases with probably oncogenic mutations, including NF1 p.R416* in one case and KEAP1 p.R470C, FBXW7 p.R399Q and TP53 p.T125M in one case. These mutations were present at relatively low variant allele fractions of 5–19%, concordant with the low proportion of histiocytes compared to inflammatory and epithelial cells in the specimen. The two cases with oncogenic mutations were histologically indistinguishable from other specimens with features of RDD. The remaining eight cases that underwent molecular analysis had only variants of uncertain significance or no mutations identified.
FOLLOW-UP INFORMATION
Follow-up data are summarised in Table 1. Among patients with follow up available, 12 patients (55%) with histological features of RDD had recurrent sinusitis necessitating repeat surgery compared to 43 chronic sinusitis patients (11%) without histological features of RDD. Upon re-review, all available previous and subsequent sinus specimens from the 12 patients with RDD features also showed histiocyte aggregates similar to the index cases, including one patient with these findings in five consecutive specimens. However, no patients with histological features of RDD developed multifocal or systemic RDD in a median 101 months’ follow-up (range = 4–303 months). Recurrent disease was seen in one patient who also had mycetoma and one patient with allergic fungal sinusitis; both additional specimens had histological features of RDD and lacked fungal organisms. Neither patient with oncogenic mutations experienced recurrent disease in 68 or 88 months’ follow-up. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Discussion
In this study, we confirm the presence of features of RDD in a subset of chronic sinusitis patients. These cases meet criteria for histological classification as RDD, including epithelioid histiocytes with abundant eosinophilic cytoplasm and dense lymphoplasmacytic inflammation. They also display essential immunohistochemical findings of RDD, with uniform S100 protein and cyclin D1 positivity and CD1a and CD207 negativity. All cases also show emperipolesis highlighted by S100 protein. A few additional histological features were notable in this case cohort. Abnormal histiocytes were arranged in discrete aggregates with a granuloma-like appearance. Most aggregates were centred in oedematous stroma, although some showed vasculocentric growth without overt vasculitis or the vasculopathy that has been described in RDD at other sites. 25, 26 Prominent intermixed eosinophils were also identified in the majority of cases with eosinophilic emperipolesis. These findings appear virtually identical to cases previously reported as RDD-like histiocytes.23
Our findings also validate the clinical significance of this histological pattern. Patients with histological features of RDD demonstrated severe pan-sinusitis symptoms and had a substantially higher need for repeat surgery compared to chronic sinusitis patients without these findings. Moreover, all previous or subsequent sinus contents specimens from these patients displayed identical histological features, suggesting that the histiocytic proliferation was instrumental to the clinical phenotype. However, there was no locally destructive, multifocal or systemic disease in any chronic sinusitis patients with features of RDD, indicating that this pattern is associated with isolated sinonasal disease. These clinical features also parallel cases reported as RDD-like histiocytes.23 Notably, these findings were seen in 3.5% of all sinus contents specimens over 2 years, suggesting that this is an uncommon but recurrent phenomenon. This histological pattern also appears to be under-recognised, as all cases identified retrospectively were originally signed out as variations on chronic or allergic sinusitis.
This unique clinical and pathological profile raises questions as to whether these cases are true RDD or a separate phenomenon. A group of nearly identical cases were previously described as RDD-like histiocytes because the overall clinicopathological picture was of chronic sinusitis, rather than RDD.23 Indeed, several features noted in this series also support separate classification. First, the abnormal histiocytes are quantitatively and qualitatively limited. Some authors have suggested that a diagnosis of RDD should only be made if pathological findings comprise more than 10% of a specimen1 – a relatively arbitrary percentage that is not yet widely accepted. The lesional histiocytes themselves do not meet this threshold in any cases in our cohort, although surrounding inflammatory milieu and oedema exceed this volume if quantified. Additionally, the histiocyte architecture is more discrete than in conventional RDD, with a nodular, granuloma-like pattern and intervening oedematous stroma rather than diffuse sheets. Furthermore, multiple features point toward a localised and reactive aetiology. These histiocytic proliferations were identified in patients with symptoms restricted to the sinonasal tract. Despite association with recurrent sinusitis, all cases showed benign behaviour with no systemic disease in long-term follow-up. A subset even demonstrated concomitant findings including allergic fungal sinusitis, mycetoma and antrochoanal polyp, similarly pointing to a reactive aetiology. These findings all suggest that pathogenesis of these limited sinonasal cases is different than conventional RDD.
Nevertheless, other findings suggest this phenomenon should be part of the RDD spectrum despite its unique manifestations. Despite the relatively limited volume of histiocytes compared to conventional RDD, they were a prominent feature throughout all cases that starkly differentiated them from other chronic sinusitis specimens. As this impression differed from the previous report of RDD-like histiocytes, which also were seen at higher prevalence,23 it is possible that we selected more florid cases. Moreover, although no cases had MAP2K1 or KRAS mutations characteristic of conventional RDD, two harboured oncogenic alterations in NF1 and KEAP1. NF1 mutations have been reported in other non-Langerhans histiocytosis, including juvenile xanthogranuloma and Erdheim–Chester disease, and also activate the MAPK/ERK pathway via RAS signalling.27, 28 The significance of KEAP1 mutation is less clear, as this gene functions in separate pathways and has not been implicated in histiocytosis.29 Regardless, the presence of oncogenic mutations in cases histologically indistinguishable from the remainder of the cohort suggests that these histiocytic proliferations are not uniformly reactive. Additionally, all cases tested expressed cyclin D1 in the abnormal histiocytes. Cyclin D1 positivity, which is absent in reactive histiocytes, has previously supported MAPK/ERK pathway activation in RDD.13 As such, this finding indicates unity with other RDD cases regardless of mutation status. Other authors have proposed that abnormal cytokines produced by lymphoma might drive MAPK/ERK pathway activation in non-neoplastic histiocytes, leading to malignancy-associated RDD.14, 30 It is conceivable that the altered cytokine milieu in chronic sinusitis31, 32 could spark a similar phenomenon. With diagnostic histological features, MAPK/ERK pathway activation and occasional oncogenic mutations, these histiocytes seem to fit within the RDD spectrum.
Ultimately, given similarities and differences from conventional RDD, we think it prudent at this point to regard this phenomenon as a limited form of RDD that carries minimal risk of systemic disease but high likelihood of recurrent sinus symptoms. While the term RDD-like histiocytes may be appropriate for very focal manifestations, we believe that cases with prominent histiocytes throughout the specimen merit recognition on the RDD spectrum. We currently sign these cases out with a top-line of ‘Limited sinonasal Rosai–Dorfman disease’ and a note indicating that these findings carry an increased risk of recurrent chronic sinusitis but are not associated with systemic disease. In some ways, this localised indolent presentation is analogous to limited histiocytoses in other epithelial sites, such as gastrointestinal Langerhans cell histiocytosis in adults, which has mild localised symptoms but no systemic involvement.33 It is also analogous to special-site considerations for other haematopoietic lesions such as duodenal-type follicular lymphoma, which is extremely indolent.34 Further research to define the minimum boundaries of RDD may help to address this phenomenon as well as other reactive or secondary RDD manifestations, leaving the door open for more nuanced classification in the future. Regardless of terminology, disproportionately high recurrent sinusitis in patients with these findings suggests that recognition of this phenomenon is clinically relevant for the management of sinus disease.
Acknowledgements
This study was funded in part by the Jane B. and Edwin P. Jenevein MD Endowment for Pathology at UT Southwestern Medical Center. No external funding was obtained for this study.
Conflicts of interest
All authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethics approval statement
All procedures performed in this retrospective data analysis involving human participants were in accordance with the ethical standards of the institutional review board (IRB) (Johns Hopkins Medicine IRB 00176183 and UT Southwestern IRB 112017–073), which did not require informed consent.
Open Research
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.