The Bowel Cancer Screening Programme Expert Board: an analysis of activity during 2017–2020
Abstract
Aims
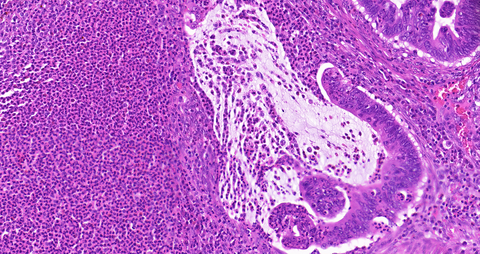
The inception of the National Health Service Bowel Cancer Screening Programme in England in 2006 highlighted the fact that the differential diagnosis between the presence of epithelial misplacement and adenocarcinoma occurring in colorectal adenomas is problematic. The pathology Expert Board (EB) was created to facilitate the review of difficult cases by a panel of three experienced gastrointestinal pathologists. This article describes a review of the work of the EB over a 4-year period (2017–2020).
Methods and results
Four hundred and thirty polyps were referred to the EB from 193 pathologists and 76 hospitals during this time. The EB diagnosis was benign for 67%, malignant for 28%, and equivocal for 2% (with no consensus in the remainder). The most common diagnosis change made by the EB was from malignant to benign—made in 50% of polyps referred with an initially malignant diagnosis. The level of agreement between the individual EB members was ‘good’ (kappa score of 0.619) but that between the EB and the referring diagnosis was ‘poor’ (kappa score of 0.149). Data from one EB member indicated that the presence of lamina propria, features of torsion and cytological similarity between the superficial and deep glands were predictors of a benign diagnosis, whereas the presence of irregular neoplastic glands, a desmoplastic reaction and lymphovascular invasion were commonly observed features in polyps with a malignant diagnosis.
Conclusion
Diagnostic agreement between EB members is better than that between the EB and referring pathologists. There was a consistent trend for the EB to change diagnoses from malignant to benign.
Graphical Abstract
Conflicts of interest
The authors declare that there are no conflicts of interest.