In-situ follicular neoplasia: a clinicopathological spectrum
Gurdip S Tamber
Department of Pathology, McGill University, Alma, Quebec, Canada
Search for more papers by this authorMyriam Chévarie-Davis
Department of Pathology, Hôpital Maisonneuve-Rosemont, Alma, Quebec, Canada
Search for more papers by this authorMargaret Warner
Division of Hematology, Department of Medicine, McGill University Health Centre, Alma, Quebec, Canada
Search for more papers by this authorChantal Séguin
Division of Hematology, Department of Medicine, McGill University Health Centre, Alma, Quebec, Canada
Search for more papers by this authorCarole Caron
Department of Pathology, Hôtel Dieu D’Alma, Alma, Quebec, Canada
Search for more papers by this authorCorresponding Author
René P Michel
Department of Pathology, McGill University, Alma, Quebec, Canada
Address for correspondence: Dr René P. Michel, Department of Pathology, McGill University, 1001 Décarie Blvd, Room E04-1456, Montreal, QC, H3A 3J1, Canada. e-mail: [email protected]
Search for more papers by this authorGurdip S Tamber
Department of Pathology, McGill University, Alma, Quebec, Canada
Search for more papers by this authorMyriam Chévarie-Davis
Department of Pathology, Hôpital Maisonneuve-Rosemont, Alma, Quebec, Canada
Search for more papers by this authorMargaret Warner
Division of Hematology, Department of Medicine, McGill University Health Centre, Alma, Quebec, Canada
Search for more papers by this authorChantal Séguin
Division of Hematology, Department of Medicine, McGill University Health Centre, Alma, Quebec, Canada
Search for more papers by this authorCarole Caron
Department of Pathology, Hôtel Dieu D’Alma, Alma, Quebec, Canada
Search for more papers by this authorCorresponding Author
René P Michel
Department of Pathology, McGill University, Alma, Quebec, Canada
Address for correspondence: Dr René P. Michel, Department of Pathology, McGill University, 1001 Décarie Blvd, Room E04-1456, Montreal, QC, H3A 3J1, Canada. e-mail: [email protected]
Search for more papers by this authorAbstract
Aims
In-situ follicular neoplasia (ISFN) occurs in approximately 2–3% of reactive lymph nodes, and is currently set apart from ‘partial involvement by follicular lymphoma’ (PFL). ISFN can progress to overt lymphoma, but precise parameters with which to assess this risk and its association with related diseases remain incompletely understood. The aim of this study was to explore these parameters.
Methods and results
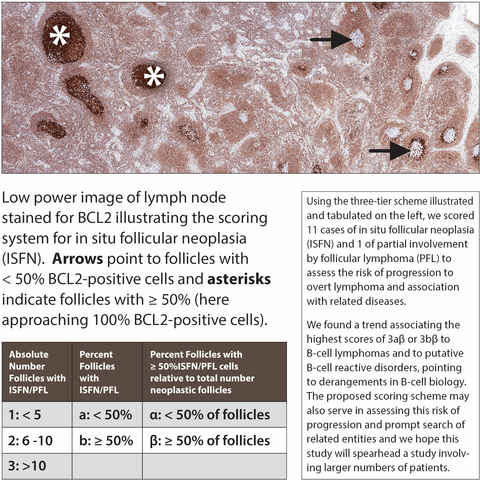
We reviewed 11 cases of ISFN and one of PFL between 2003 and 2018. Ten patients had ISFN in the lymph nodes, and one had ISFN in the spleen. Haematoxylin and eosin and immunohistochemical stains were reviewed. Involvement of follicles by ISFN was scored with a three-tier scheme. Of five patients with low ISFN scores, one had chronic myelomonocytic leukaemia, one had mycosis fungoides, and three were free of haematopoietic disease. Among them, four are alive and one was lost to follow-up. Of the six ISFN patients with high scores, two had concurrent marginal zone lymphomas, one had concurrent diffuse large B-cell lymphoma (DLBCL), one had Castleman-like disease, one had progressive transformation of germinal centres with IgG4-related disease, and one had no haematopoietic disease; all are alive except for one who died of concurrent DLBCL. The patient with PFL developed DLBCL 7 years after diagnosis.
Conclusions
On the basis of this limited series, we conclude that only cases with high scores are associated with an overt lymphoma or an abnormal lymphoid process, and that scoring may be a useful parameter with which to assess the risk of associated lymphoma, and deserves further study. We also performed a comprehensive review of the literature.
Graphical Abstract
Conflicts of interest
All of the authors have no conflicts of interest to declare.
References
- 1Williams J. Cancer of the uterus: Harveian lectures for 1886. London: H. K. Lewis, 1888; 119.
- 2Pruneri G, Mazzarol G, Manzotti M, Viale G. Monoclonal proliferation of germinal center cells (incipient follicular lymphoma) in an axillary lymph node of a melanoma patient. Hum. Pathol. 2001; 32; 1410–1413.
- 3Su W, Spencer J, Wotherspoon AC. Relative distribution of tumour cells and reactive cells in follicular lymphoma. J. Pathol. 2001; 193; 498–504.
- 4Jaffe ES, Harris NL, Swerdlow SH et al. Follicular lymphoma. In SH Swerdlow, E Campo, NL Harris et al. eds. World Health Organization classification of tumours of haematopoietic and lymphoid tissues, revised 4th ed. Lyon: IARC Press, 2017; 266–277.
- 5Cong P, Raffeld M, Teruya-Feldstein J, Sorbara L, Pittaluga S, Jaffe ES. In situ localization of follicular lymphoma: description and analysis by laser capture microdissection. Blood 2002; 99; 3376–3382.
- 6Jegalian AG, Eberle FC, Pack SD et al. Follicular lymphoma in situ: clinical implications and comparisons with partial involvement by follicular lymphoma. Blood 2011; 118; 2976–2984.
- 7Henopp T, Quintanilla-Martinez L, Fend F, Adam P. Prevalence of follicular lymphoma in situ in consecutively analysed reactive lymph nodes. Histopathology 2011; 59; 139–142.
- 8Bermudez G, Gonzalez de Villambrosia S, Martinez-Lopez A et al. Incidental and isolated follicular lymphoma in situ and mantle cell lymphoma in situ lack clinical significance. Am. J. Surg. Pathol. 2016; 40; 943–949.
- 9Pillai RK, Surti U, Swerdlow SH. Follicular lymphoma-like B cells of uncertain significance (in situ follicular lymphoma) may infrequently progress, but precedes follicular lymphoma, is associated with other overt lymphomas and mimics follicular lymphoma in flow cytometric studies. Haematologica 2013; 98; 1571–1580.
- 10Schmidt J, Salaverria I, Haake A et al. Increasing genomic and epigenomic complexity in the clonal evolution from in situ to manifest t(14;18)-positive follicular lymphoma. Leukemia 2014; 28; 1103–1112.
- 11Schmidt J, Ramis-Zaldivar JE, Bonzheim I et al. CREBBP gene mutations are frequently detected in in situ follicular neoplasia. Blood 2018; 132; 2687–2690.
- 12van Dongen JJM, Langerak AW, Brüggemann M et al. Design and standardization of PCR primers and protocols for detection of clonal immunoglobulin and T-cell receptor gene recombinations in suspect lymphoproliferations: report of the BIOMED-2 Concerted Action BMH4-CT98-3936. Leukemia 2003; 17; 2257–2317.
- 13Swerdlow SH, Campo E, Harris NL et al. eds. World Health Organization classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon: IARC Press, 2008.
- 14Swerdlow SH, Campo E, Harris NL et al. eds. World Health Organization classification of tumours of haematopoietic and lymphoid tissues. revised 4th ed. Lyon: IARC Press, 2017.
- 15Quintanilla-Martinez L, Adam P, Fend F. In situ lymphoma and other early stage malignant non-Hodgkin lymphomas. Pathologe 2013; 34; 244–253.
- 16Carbone A, Gloghini A. ‘Intrafollicular neoplasia’ of nodular lymphocyte predominant Hodgkin lymphoma: description of a hypothetic early step of the disease. Hum. Pathol. 2012; 43; 619–628.
- 17A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin’s lymphoma. the Non-Hodgkin’s Lymphoma Classification Project. Blood. 1997; 89; 3909–3918.
- 18Roullet MR, Martinez D, Ma L et al. Coexisting follicular and mantle cell lymphoma with each having an in situ component: a novel, curious, and complex consultation case of coincidental, composite, colonizing lymphoma. Am. J. Clin. Pathol. 2010; 133; 584–591.
- 19Wang H, Su T, Kang L, Yang L, Wang S. Diffuse large B cell lymphoma in a preceding IgG4-related disease with kidney restricted lambda light chain expression: case report and literature review. BMC Nephrol, 2020; 21; 315.
- 20Bledsoe JR, Wallace ZS, Stone JH, Deshpande V, Ferry JA. Lymphomas in IgG4-related disease: clinicopathologic features in a western population. Virchows Arch. 2018; 472; 839–852.
- 21Hsi ED, Schnitzer B. Reactive lymphadenopathies. In ES Jaffe, DA Arber, E Campo, NL Harris, L Quintanilla-Martinez eds. Hematopathology. Philadelphia, PA: Elsevier, 2017; 153–177.
- 22Mamessier E, Broussais-Guillaumot F, Chetaille B et al. Nature and importance of follicular lymphoma precursors. Haematologica 2014; 99; 802–810.
- 23Dolken G, Dolken L, Hirt C, Fusch C, Rabkin CS, Schuler F. Age-dependent prevalence and frequency of circulating t(14;18)-positive cells in the peripheral blood of healthy individuals. J. Natl. Cancer Inst. Monogr. 2008; 39; 44–47.
10.1093/jncimonographs/lgn005 Google Scholar
- 24Cheung MC, Bailey D, Pennell N et al. In situ localization of follicular lymphoma: evidence for subclinical systemic disease with detection of an identical BCL-2/IGH fusion gene in blood and lymph node. Leukemia 2009; 23; 1176–1179.
- 25Belaud-Rotureau MA, Parrens M, Carrere N et al. Interphase fluorescence in situ hybridization is more sensitive than BIOMED-2 polymerase chain reaction protocol in detecting IGH-BCL2 rearrangement in both fixed and frozen lymph node with follicular lymphoma. Hum. Pathol. 2007; 38; 365–372.
- 26Espinet B, Bellosillo B, Melero C et al. FISH is better than BIOMED-2 PCR to detect IGH/BCL2 translocation in follicular lymphoma at diagnosis using paraffin-embedded tissue sections. Leuk. Res. 2008; 32; 737–742.
- 27Bonzheim I, Salaverria I, Haake A et al. A unique case of follicular lymphoma provides insights to the clonal evolution from follicular lymphoma in situ to manifest follicular lymphoma. Blood 2011; 118; 3442–3444.
- 28Carbone A, Della Libera D, Zannier L et al. In situ follicular lymphoma associated with overt B- orT-cell lymphomas in the same lymph node. Am. J. Hematol. 2011; 86; E66–E70.
- 29Carbone A, Tibiletti MG, Zannier L, Selva A, Sulfaro S, Gloghini A. A unique case of extranodal DLBCL sharing genetic abnormalities with a synchronous ileal lymphoma exhibiting immunoarchitectural features of in situ follicular lymphoma. Am. J. Hematol. 2012; 87; E134–E135.
- 30Mamessier E, Drevet C, Broussais-Guillaumot F et al. Contiguous follicular lymphoma and follicular lymphoma in situ harboring N-glycosylated sites. Haematologica 2015; 100; e155–e157.
- 31Morita K, Nakamine H, Nakai T et al. A retrospective study of patients with follicular lymphoma (FL): identification of in situ FL or FL-like B cells of uncertain significance in lymph nodes resected at the time of previous surgery for carcinomas. J. Clin. Pathol. 2015; 68; 541–546.
- 32Bödör C, Grossmann V, Popov N et al. EZH2 mutations are frequent and represent an early event in follicular lymphoma. Blood 2013; 122; 3165–3168.
- 33Green MR, Gentles AJ, Nair RV et al. Hierarchy in somatic mutations arising during genomic evolution and progression of follicular lymphoma. Blood 2013; 121; 1604–1611.
- 34Mamessier E, Song JY, Eberle FC et al. Early lesions of follicular lymphoma: a genetic perspective. Haematologica 2014; 99; 481–488.
- 35Vogelsberg A, Steinhilber J, Mankel B et al. Genetic evolution of in situ follicular neoplasia to aggressive B-cell lymphoma of germinal center subtype. Haematologica 2020. E-pub ahead of print, 27 August.
- 36Banz Y, Tzankov A, Dirnhofer S, Perren A, Hoeller S. Lymphadenectomy specimens in a large retrospective cohort of pediatric patients reveal no in situ lymphomas but a broad spectrum of reactive changes. Pathobiology 2017; 84; 139–143.
- 37Ferry JA, de Leval L, Louissant A, Harris NL. Follicular lymphoma. In ES Jaffe, DA Arber, E Campo, NL Harris, L Quintanilla-Martinez eds. Hematopathology. Philadelphia, PA: Elsevier, 2017; 321–352.
- 38Gru AA, Kreisel F, Duncavage E, Nguyen TT, Hassan A, Frater JL. Acute EBV infection masquerading as ‘in-situ follicular lymphoma’: a pitfall in the differential diagnosis of this entity. Diagn. Pathol. 2013; 8; 100.
- 39Torlakovic E, Torlakovic G. Follicular colonization by follicular lymphoma. Arch. Pathol. Lab. Med. 2002; 126; 1136–1137.
- 40Sotomayor EA, Shah IM, Sanger WG, Mark HF. In situ follicular lymphoma with a 14;18 translocation diagnosed by a multimodal approach. Exp. Mol. Pathol. 2007; 83; 254–258.
- 41Montes-Moreno S, Castro Y, Rodriguez-Pinilla SM et al. Intrafollicular neoplasia/in situ follicular lymphoma: review of a series of 13 cases. Histopathology 2010; 56; 658–662.
- 42Handa T, Maki K, Segawa A, Masawa N, Mitani K. In situ follicular lymphoma associated with progressive transformation of germinal centers. Int. J. Surg. Pathol. 2011; 19; 521–523.
- 43McDonald CL, Calzada PJ. Crohn’s disease diagnosis following discovery of in situ follicular lymphoma. Gastrointest. Cancer Res. 2011; 4; 184–187.
- 44Carbone A, Tibiletti MG, Canzonieri V et al. In situ follicular lymphoma associated with nonlymphoid malignancies. Leuk. Lymphoma 2012; 53; 603–608.
- 45Li JN, Zhang WY, Tang Y, Li GD, Dong DD. In situ follicular lymphoma with progressive transformation of the germinal centers confirmed by laser capture microdissection, IGH gene rearrangement analysis, and fluorescence in situ hybridization for t(14;18). Hum. Pathol. 2012; 43; 138–143.
- 46Sakhadeo U, Mane A, Shet T. In situ follicular neoplasia/lymphoma: three illustrative cases exemplifying unique disease presentations. Indian J. Pathol. Microbiol. 2012; 55; 218–221.
- 47Lee JC, Hoehn D, Schecter J et al. Lymphoid follicle colonization by BCL-2(bright+)CD10(+) B-cells (‘follicular lymphoma in situ’) at nodal and extranodal sites can be a manifestation of follicular homing of lymphoma. Hum. Pathol. 2013; 44; 1328–1340.
- 48Obumneme ON, Uche I, Adekunbiola B, Ralph A, Nicholas I. Follicular lymphoma in situ presenting as dermatopathic lymphadenopathy. Case Rep. Pathol. 2013; 2013; 481937.
- 49Alobeid B, Mears JG, Bhagat G. Follicular lymphoma (in situ) pattern in the bone marrow: does it indicate an early stage in disease evolution? Clin. Case Rep. 2015; 3; 442–443.
- 50Ferry JA, Klepeis V, Sohani AR et al. IgG4-related orbital disease and its mimics in a western population. Am. J. Surg. Pathol. 2015; 39; 1688–1700.
- 51Kurian RR, Balamurugan T, Ping B, Hendry L, Whitaker S, Bagwan I. Follicular lymphoma in situ in intra-abdominal lymphadenectomies—a study of 5 cases: revisiting the entity. Adv. Mod. Oncol. Res. 2015; 1; 62–67.
10.18282/amor.v1.i1.22 Google Scholar
- 52Sagasta A, Molina-Urra R, Martinez D et al. CD8-positive peripheral T-cell lymphoma with aberrant expression of CD20 and concurrent in situ follicular lymphoma. J. Cutan. Pathol. 2015; 42; 66–72.
- 53Roncati L, Maiorana A. Ectopic extra-nodal in situ follicular neoplasia (ISFN). J. Hematopathol. 2016; 9; 151–153.
- 54Suarez JP, Dominguez ML, Gomez MA, Fernandez N, Munoz J. A unique case of in situ follicular lymphoma associated with two nonlymphoid malignancies. Leuk. Lymphoma 2016; 57; 2917–2918.
- 55Teixeira Mendes LS, Wotherspoon A. The relationship between overt and in-situ lymphoma: a retrospective study of follicular and mantle cell lymphoma cases. Histopathology 2016; 68; 461–463.
- 56Conde-Montero E, Baniandres-Rodriguez O, Horcajada-Reales C, Parra-Blanco V, Suarez-Fernandez R. Paraneoplastic acrokeratosis (Bazex syndrome): unusual association with in situ follicular lymphoma and response to acitretin. Cutis 2017; 100; E3–E5.
- 57Kashimura M, Kojima M, Matsuyama N, Tadokoro J. Follicular lymphoma in situ in the spleen of a patient with autoimmune hemolytic anemia and carrying HCV was associated with more clonal B-cells than t(14;18) positive B-cells. Pathol. Res. Pract. 2017; 213; 585–589.
- 58Jelloul FZ, Chen QH, Yang T et al. Composite small lymphocytic lymphoma/chronic lymphocytic leukemia and follicular lymphoma: a clinicopathological study of six cases. Int. J. Surg. Pathol. 2018; 26; 135–144.
- 59Kosmidis P, Mankel B, Fend F, Adam P. The t(14;18) translocation is absent from endothelial and follicular dendritic cells of follicular lymphoma (FL) and shows heterogeneous presence in preserved FL mantle zones. Diagn. Pathol. 2018; 13; 25.
- 60Nardi V, Kuo FC, Hasserjian RP. Premalignant clonal hematopoietic proliferations. Am. J. Clin. Pathol. 2019; 152; 347–358.
- 61Alnoor FNU, Gandhi JS, Stein MK, Solares J, Gradowski JF. Prevalence of lymphoid neoplasia in a retrospective analysis of Warthin tumor: a single institution experience. Head Neck Pathol. 2020; 14; 944–950.
- 62Koh J, Jeon YK. Morphologic variant of follicular lymphoma reminiscent of hyaline-vascular Castleman disease. J. Pathol. Transl. Med. 2020; 54; 253–257.