Effectiveness of therapeutic exercise and cognitive-behavioural therapy combined protocol on functionality, pain and joint health in people with haemophilia: Secondary analysis of a controlled trial
Abstract
Background
Haemophilic arthropathy is one of the main causes of morbidity in people with haemophilia (PWH), inducing pain and reduced functionality. Therefore, PWH are complex patients and must be approached from a multidisciplinary perspective.
Objectives
To evaluate the effectiveness of a therapeutic exercise and cognitive-behavioural therapy (CBT) combined protocol on functionality, pain, and joint health of PWH, arthropathy and chronic pain. Treatment satisfaction was also evaluated.
Methods
A single-blinded clinical trial with 21 PWH in prophylactic regimen was carried out. Participants were divided into an experimental group (EG, n = 11) and a control group (CG, n = 10). The EG underwent a 4-month programme of home-based therapeutic exercise plus CBT, whilst CG performed their daily activities. Patients were evaluated at baseline, post-intervention and after 12 additional weeks. Measures of functionality (Haemophilia Activities List, Timed Up and Go Test, 2-Minutes-Walking-Test and Sit-to-Stand Test), pain (PainDETECT and Visual Analogue Scale) and joint health (Haemophilia Joint Health Score) were taken. Related dimensions of the A36 Haemophilia Quality of Life Questionnaire were calculated. Effects were calculated using a two-factor ANOVA.
Results
The EG showed significant improvements in function (p < .001), pain (p < .001), joint damage (p = .006), and satisfaction with the treatment (p = .006) dimensions of the A36 Haemophilia Quality of Life Questionnaire, as well as in pain measured with the Visual Analogue Scale (p = .008) and PainDETECT (p = .035).
Conclusions
The combined physiotherapy and CBT protocol showed a partial improvement in functionality, pain and joint health of PWH, arthropathy and chronic pain. In addition, participants were satisfied with the treatment.
1 INTRODUCTION
Haemophilia is a disease linked to the X chromosome which results in an absence or decrease of coagulation factor VIII or IX.1 This triggers spontaneous or provoked haemorrhages in different parts of the body, joints being the most frequent location.2 Haemophilic arthropathy (HA) is therefore one of the main causes of morbidity in people with haemophilia (PWH). HA is responsible, in 32%–50% of patients, for the chronic pain experienced, the reduction in physical activity and the functionality decrease.1, 3-5 Regarding health-related quality of life, several investigations have shown that PWH had similar scores to the general population in domains related to mental health, emotional health and social relationships; but they found their physical function and pain deteriorated.4, 6 In addition, pain seems to have nociceptive origin, and although a neuropathic component has been found in some patients, it is not the most commonly reported.7, 8
Therefore, PWH are complex patients that must be approached from a multidisciplinary perspective, with individualized treatments in specialized centres.1, 3 Two therapies that have been shown, separately or in combination, to be effective in improving chronic pain, self-efficacy and perception of pain, quality-of-life, kinesiophobia and physical function are exercise and psychological therapy.9-12 However, recent studies suggest that the physical activity performed by PWH is significantly lower than the World Health Organization recommendations, especially in those with severe haemophilia.11, 13 This fact can negatively influence physical condition, functionality, join health and pain in PWH. For this reason, it is important that PWH take part in regular exercise programmes based in strength, cardiovascular endurance and flexibility.12, 14
Regarding psychological intervention in pain management in haemophilia, objectives are recommended to be realistic, as well as based in the reduction of fear and avoidance patterns and the creation of active strategies to cope with pain and stress.5 Cognitive-behavioural therapy (CBT) is a tool used to challenge cognitive distortions related to chronic pain and adopt adaptive coping strategies, since psychosocial factors affect the painful experience of patients with haemophilic arthropathy.3, 9, 15, 16
Therefore, the main objective of this study was to evaluate the effectiveness of a combined protocol of therapeutic exercise and CBT in the functionality of PWH, arthropathy and chronic pain. Secondary objectives were to determine the effectiveness of the combined protocol on pain and joint health. In addition, satisfaction with the treatment was studied. We hypothesised that the programme would be effective in increasing functionality and joint health of PWH, and reducing pain, chronic pain and arthropathy. Also, the patients will be satisfied with the treatment.
2 METHODS
2.1 Study design
The present study was a single-blinded, double-armed, parallel-group controlled clinical trial. Participants were recruited from the Haemostasis and Thrombosis Unit of the University and Polytechnic Hospital La Fe, Valencia, Spain. The study was registered in www.ClinicalTrials.gov (NCT03529474). Other data from this study have been used in a previous article, which addressed a different research question.9
2.2 Participants
All participants were informed about the purpose and content of the project and gave their written informed consent to participate in the study. All procedures were approved by the institution's Review Board (2017/0320) and comply with the requirements listed in the 1975 Declaration of Helsinki and its amendment in 2008.
2.3 Sample
A priori power analysis was conducted in G*Power software (3.1.9.2 version) where a total of 20 participants was estimated (α = .05, power = .80), assuming at least a medium effect size (f = .30). To confirm that the final sample was sufficient, a post hoc power analysis was performed using the obtained effect sizes.
The inclusion criteria were: people with severe haemophilia A or B, between 18 and 60 years old, with HA in at least one of the three most commonly affected joints (i.e., elbows, knees or ankles) according to the Gilbert17 or Pettersson scale,18 in prophylaxis regimen, with chronic pain and absence of active pain coping strategies (evaluated by a psychologist through a personal interview who considered active coping strategies these that favour positive adaptation to pain: constant use of distraction, self-affirmation, search for information to learn about proper management and problem solving). Those with presence of inhibitors, severe cognitive deficit, another haemostatic defect, or surgeries performed in the 6 months prior to or during the study were excluded.
2.4 Intervention
Participants were distributed by convenience sampling, based on the commitment of the participants to carry out the intervention, into two groups: experimental group (EG) and control group (CG). The EG underwent a combined therapeutic exercise and CBT intervention, while the CG performed their usual daily activities and were instructed not to start any new exercise programme during the 28-week duration of the study. Briefly, the home therapeutic exercise sessions consisted of three sessions/week dosed by a physiotherapist based on the OMNI scales of perceived exertion,19, 20 and consisted of: warm-up, aerobic training, strength-resistance training with elastic bands and stretching. The intensity of the therapeutic exercise oscillated between 3–4/10 (low intensity) and 6–7/10 (moderate intensity) punctuation on the OMNI scales. The CBT intervention consisted of 4 individual monthly sessions, based on the biopsychosocial conceptualization of pain using an adaptation of the protocol of Moix et al.21 The protocol carried out is explained in detail in a study by García-Dasi et al.9 and breafly in Supplementary material 1 and 2.
2.5 Measurements
Outcome measures were collected by a blind assessor at baseline (T0), after 16 weeks of supervised intervention (T1) and after 12 additional weeks (T2). Clinical and sociodemographic data, previous exercise performed, frequency, intensity and duration of the exercise were collected at baseline. The following outcomes were assessed.
2.5.1 Primary outcome
For assessing functionality, the Haemophilia Activities List (HAL)22 was used, where 0 represents the worst imaginable serf-perceived functionality and 100 the best. In addition to the total score, the 42 HAL questions generate 7 domain scores where higher punctuations imply the worst self-perceived functionality. Psychometric characteristics showed good values in terms of reliability (internal consistency α = .97 and test-retest ICC > .9) and convergent validity (Dutch Arthritis Impact Measurement Scale 2 and the Participation and Autonomy Impact Questionnaire).23 In addition, three functional tests were administered: (a) Timed Up and Go Test (TUG),24 where longer times imply worse functionality. This test presented good psychometric values in terms of specificity (.74, IC 95% .52–.88), sensitivity (.31, 95%, .13–.57) and reliability (test-retest ICC = .91); (b) 2-Minutes-Walking-Test (2MWT),25 where larger distances imply better functionality. This test has shown good psychometric values with a test-retest reliability index of ICC = .82 (95%CI: .76–.87), convergent validity (Berg Scale, TUG and 6-minutes-walking-test) and an area under the ROC curve .81 (p = .001); (c) Sit-to-Stand-Test (STST),26 where longer times imply worse functionality.
2.5.2 Secondary outcomes
For assessing current pain, the following questionnaires were administered. The Visual Analogue Scale (VAS), where 0 represents ‘no pain’ and 10, ‘the worst imaginable pain’. Psychometric characteristics showed good values in terms of reliability (internal consistency α = .84 and test-retest r = .79–.92). Moreover, the PainDETECT questionnaire27 was employed as a screening tool for neuropathic pain, and ranged from –1 to 38, where scores ≤12 imply ‘negative neuropathic component’, 13 to 18 ‘unclear neuropathic component’ and ≥19 ‘positive neuropathic component’. This questionnaire has acceptable psychometric rating scale properties in terms of reliability (internal consistency α = .78 and test-retest ICC = .94).
Regarding joint health, the Haemophilia Joint Health Score (HJHS)28, 29 was employed. HJHS is a clinical scale that scores each joint from 0 to 20 points and global gait from 0 to 4. Higher scores reflect worse joint condition (maximum score of 124 points, sum of elbows, knees, ankles and global gait). Psychometric characteristics showed good values in terms of reliability (internal consistency α = .83–.84) and convergent validity (Petterson Score).
In addition, the evaluation of the primary and secondary variables was enriched with the results from A36 Haemo-QoL related dimensions in order to complete information about the patients’ perceptions: ‘Physical health’ and ‘Daily activities’ (functionality); ‘Pain’ (pain); ‘Joint damage’ (joint health). Also, satisfaction with the treatment was evaluated with the ‘Satisfaction with the treatment’ dimension.30 The A36 Haemo-QoL has shown good psychometric values in terms of reliability internal consistency (α = .95) and test-retest (r = .92, p = .001) and convergent validity (SF-36 Health Survey), external criteria validity (clinical status) and sensitivity to change.
2.6 Statistics
Normality of the data was checked using the Shapiro-Wilk test. Descriptive measures were shown as mean (standard deviation) or frequencies. Demographic variables were compared using the independent samples T test or the Wilcoxon rank sum test. To determine the effects of the intervention on time (T0, T1 and T2) and group (experimental or control) factors, a two-factor ANOVA with repeated measures in the time factor for each of the study variables was used. Bonferroni correction was applied to avoid type I errors in multiple comparisons when ANOVA analysis indicated significant differences (p < .05). Effect sizes have been interpreted as small (d = .2; ηp2 = .01), medium (d = .5; ηp2 = .06) or large (d > .8; ηp2 = .14). All statistical analyses were carried out in IBM SPSS Statistics software (Version 22.0, IBM Corp, Armonk, NY).
3 RESULTS
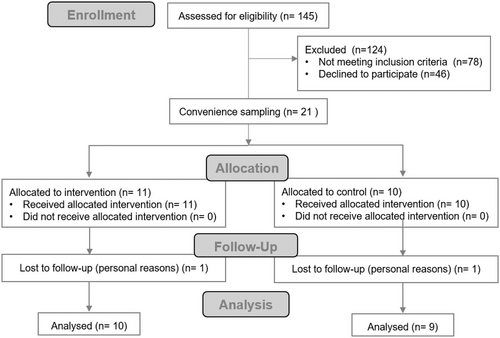
A total of 19 participants constituted the final sample, 10 in the EG and 9 in the CG (Figure 1). According to the post hoc power analysis, with the minimum effect size obtained in the variables that were significant (d = .70; f = .35) and with 19 participants, the final power was .90.
Clinical and demographic variables are depicted in Table 1. No significant differences were found between groups, except in the Factor VIII dose, which was significantly higher in the CG. Total 40.0% of the EG participants did not perform exercise prior to the study compared to 33.3% in the CG. The exercise most performed in both groups was the combination of activities such as gait, swim or weight training (66.7% in the EG and 66.6% in the CG), the intensity ranged from light to hard in most cases. Regarding the duration of the exercise, 50.0% of the EG participants reported 30–60 min per session, while 50.0% of the EG participants reported more than 60 min per session.
| EG (n = 10) | CG (n = 9) | p [95% CI] | |
|---|---|---|---|
| Age (years) | 45.00 (8.56) | 37.89 (13.31) | .12 [–2.03:16.25] |
| Duration of pain (years) | 16.43 (15.18) | 10.78 (8.12) | .33 [–6.34:17.64] |
| Height (cm) | 171.30 (4.22) | 171.33 (7.02) | .99 [–5.57:5.79] |
| Weight (kg) | 73.72 (12.55) | 66.54 (6.61) | .14 [–2.71:17.06] |
| Total HJHS | 39.70 (19.24) | 25.44 (11.17) | .07 [–1.22:29.73] |
| Haemophilia type (A/B) | 10/0 | 8/1 | – |
| HIV (n) | 7 | 4 | – |
| HCV (n) | 8 | 4 | – |
| Factor VIII dose (IU/kg) (n = 18) | 22.98 (8.58) | 31.43 (6.46) | .035 [–16.21:–.68] |
| Factor IX dose (IU/kg) (n = 1) | – | 56.00 | – |
- Data are expressed as mean (standard deviation).
- Abbreviations: cm, centimetres; CG, control group; CI, confidence interval for the mean difference; EG, experimental group; p, statistical significance; HCV, hepatitis C virus; HIV, human immunodeficiency virus; HJHS, Haemophilia Joint Heath Score; IU/kg: international units per kilogram; kg, kilograms.
In relation to functionality (Table 2), the results of the ANOVA test for HAL and for the functional tests (2MWT, TUG and STST) did not show within-group significant differences. The between-group analysis showed that at T0, the CG showed better results in ‘Sum score’, ‘Lying/sitting/kneeling/standing’ and ‘Complex lower extremity activities’ dimensions of HAL, as well as in the 2MWT, and also in ‘Physical health’ and ‘Daily activities’ dimensions of A36 Haemo-QoL. At T1, there were significant differences in ‘Lying/sitting/kneeling/standing’ and ‘Complex lower extremity activities’ dimensions of HAL, and in the STST; however, the CG showed better results than the EG, and these differences were maintained in T2. When compared with T0, the within-group (T0 vs. T1 and T0 vs. T2) analysis indicated that the intervention protocol had a significant effect in the EG in ‘Physical Health’ and ‘Daily activities’ dimensions of A36 Haemo-QoL. No within-group differences were found for the CG.
| T0 | T1 | T2 | p1 [95% CI]; ES | p2 [95% CI]; ES | ||
|---|---|---|---|---|---|---|
| HAL questionnaire | ||||||
| Lying/ sitting/ kneeling/ standing | EG | 45.75 (22.76) | 54.25 (26.88) | 57.50 (24.18) | 1.00 [–31.81:14.81] | .52 [–33.76:10.26] |
| CG | 82.50 (19.41) | 83.13 (17.72) | 86.25 (18.90) | 1.00 [–26.68:25.43] | 1.00 [–28.36:20.86] | |
| p0 [95% CI]; ES | .002 [–58.23:–15.27]; 1.73 | .019 [–52.32:–5.43]; 1.25 | .014 [–50.90:–6.60]; 1.32 | |||
| Function of the legs | EG | 43.77 (23.17) | 60.22 (18.46) | 61.56 (19.44) | .25 [–40.21:7.31] | .15 [–40.04:4.46] |
| CG | 69.18 (28.93) | 74.16 (17.54) | 74.71 (25.01) | 1.00 [–31.55:21.57] | 1.00 [–30.41:19.34] | |
| p0 [95% CI] | .06 [–51.40:.59] | .12 [–32.11:4.22] | .23 [–35.33:9.02] | |||
| Function of the arms | EG | 80.50 (21.01) | 86.50 (16.34) | 85.50 (17.71) | 1.00 [–25.74:13.74] | 1.00 [–29.16:19.16] |
| CG | 73.75 (20.49) | 87.50 (12.82) | 84.38 (12.94) | .35 [–35.82:8.32] | .93 [–37.64:16.39] | |
| p0 [95% CI] | .50 [–14.15:27.65] | .89 [–15.98:13.98] | .88 [–14.73:17.01] | |||
| Use of transportation | EG | 63.34 (29.34) | 76.66 (19.69) | 67.33 (24.44) | .46 [–37.13:10.49] | 1.00 [–28.97:20.99] |
| CG | 80.00 (26.66) | 88.34 (16.61) | 89.18 (21.05) | 1.00 [–34.95:18.28] | 1.00 [–37.10:18.75] | |
| p0 [95% CI] | .23 [–45.02:11.70] | .20 [–30.19:6.83] | .06 [–44.99:1.30] | |||
| Self-care | EG | 86.80 (14.73) | 92.00 (10.15) | 89.60 (14.01) | .86 [–17.84:7.44] | 1.00 [–16.38:10.78] |
| CG | 92.50 (8.67) | 89.50 (11.70) | 91.00 (11.66) | 1.00 [–11.13:17.13] | 1.00 [–13.68:16.68] | |
| p0 [95% CI] | .35 [–18.22:6.82] | .63 [–8.42:13.42] | .82 [–14.51:11.71] | |||
| Household tasks | EG | 80.00 (27.90) | 87.67 (17.42) | 84.00 (13.96) | .88 [–26.56:11.22] | 1.00 [–24.77:16.77] |
| CG | 87.49 (17.53) | 90.00 (10.54) | 91.26 (8.53) | 1.00 [–23.63:18.61] | 1.00 [–27.00:19.45] | |
| p0 [95% CI] | .52 [–31.55:16.57] | .74 [–17.22:12.56] | .22 [–19.22:4.70] | |||
| Leisure activities and sports | EG | 67.15 (29.55) | 77.43 (27.76) | 77.43 (23.35) | 1.00 [–38.20:17.64] | .91 [–36.18:15.62] |
| CG | 81.79 (17.15) | 77.50 (16.41) | 82.51 (15.91) | 1.00 [–26.93:35.50] | 1.00 [–29.68:28.23] | |
| p0 [95% CI] | .23 [–39.67:10.40] | 1.00 [–23.68:23.54] | .61 [–25.63:15.46] | |||
| Upper extremity activities | EG | 84.00 (13.13) | 89.54 (9.83) | 87.79 (13.42) | .74 [–17.87:6.79] | 1.00 [–18.06:10.48] |
| CG | 84.18 (12.36) | 88.61 (9.84) | 88.04 (9.52) | 1.00 [–18.22:9.35] | 1.00 [–19.82:12.09] | |
| p0 [95% CI] | .98 [–13.04:12.69] | .85 [–8.96:10.82] | .97 [–12.18:11.69] | |||
| Basic lower extremity activities | EG | 55.01 (29.58) | 79.66 (20.09) | 77.34 (21.02) | .06 [–49.93:.63] | .11 [–48.53:3.87] |
| CG | 75.83 (26.12) | 79.16 (19.44) | 78.75 (27.61) | 1.00 [–31.61:24.93] | 1.00 [–32.22:26.37] | |
| p0 [95% CI] | .14 [–49.09:7.46] | .96 [–19.42:20.41] | .90 [–25.67:22.85] | |||
| Complex lower extremity activities | EG | 30.00 (22.52) | 36.23 (31.00) | 39.12 (30.16) | 1.00 [–31.65:19.19] | .92 [–32.21:13.97] |
| CG | 67.78 (24.41) | 71.94 (17.81) | 74.45 (23.84) | 1.00 [–32.59:24.26] | 1.00 [–32.49:19.14] | |
| p0 [95% CI]; ES | .004 [–61.27:14.28]; 1.61 | .011 [–61.92:–9.50]; 1.39 | .016 [–63.06:–7.60]; 1.29 | |||
| Sum score | EG | 63.23 (19.02) | 73.33 (17.51) | 72.67 (16.75) | .40 [–27.13:6.93] | .42 [–25.75:6.87] |
| CG | 80.41 (13.72) | 82.81 (7.74) | 84.46 (12.32) | 1.00 [–21.44:16.64] | 1.00 [–22.29:14.19] | |
| p0 [95% CI]; ES | .048 [–34.20:–.19]; 1.03 | .18 [–23.66:4.69] | .12 [–26.85:–3.26] | |||
| Functional tests | ||||||
| 2MWT (metres) | EG | 166.40 (40.55) | 173.45 (46.04) | 171.44 (45.74) | .47 [–19.63:5.54] | 1.0 [–19.13:9.05] |
| CG | 211.66 (31.63) | 206.33 (28.27) | 202.06 (31.92) | .90 [–7.94:18.59] | .31 [–5.25:24.45] | |
| p0 [95% CI]; ES | .016 [–80.76:–9.75]; 1.24 | .08 [–70.40:4.64] | .11 [–69.24:8.01] | |||
| TUG (sec) | EG | 7.60 (2.61) | 7.93 (3.07) | 7.71 (2.87) | .68 [–1.02:.36] | 1.00 [–.54:.31] |
| CG | 5.60 (1.23) | 5.82 (1.18) | 5.83 (1.22) | 1.00 [–.95:.50] | .53 [–.69:.21] | |
| p0 [95% CI] | .05 [–.01:4.02] | .07 [–.20:4.41] | .09 [–.30:4.06] | |||
| STST (sec) | EG | 11.37 (4.13) | 12.37 (4.88) | 12.02 (4.21) | .41 [–2.71:.70] | .86 [–2.23:.92] |
| CG | 8.33 (4.11) | 8.16 (3.49) | 7.57 (2.87) | 1.00 [–1.62:1.97] | .71 [–.89:2.42] | |
| p0 [95% CI]; ES | .13 [–.96:7.03] | .047 [.06:8.36]; .98 | .02 [.92:7.98]; 1.22 | |||
| Dimensions of A36 Haemo-QoL | ||||||
| ‘Physical Health’ | EG | 14.50 (6.75) | 26.90 (9.02) | 23.60 (6.06) | <.001 [–18.34:–6.46]; 1.57 | <.001 [–13.10:–5.10]; 1.46 |
| CG | 21.11 (4.37) | 23.33 (4.69) | 22.89 (4.37) | 1.00 [–8.48:4.04] | .84 [–6.00:2.44] | |
| p0 [95% CI]; ES | .023 [–12.19:–1.03]; 1.15 | .30 [–3.52:10.66] | .78 [–4.46:5.88] | |||
| ‘Daily activities’ | EG | 5.20 (4.87) | 12.60 (4.33) | 12.90 (4.23) | .001 [–11.63:–3.17]; 1.28 | <.001 [–11.90:–3.50]; 1.47 |
| CG | 10.00 (2.00) | 11.11 (4.51) | 10.22 (4.60) | 1.00 [–5.57:3.35] | 1.00 [–4.65:4.21] | |
| p0 [95% CI]; ES | .014 [–8.49:–1.12]; 1.26 | .47 [–2.79:5.77] | .20 [–1.60:6.95] | |||
- Data are expressed as mean (standard deviation). CI: confidence interval for the mean difference. The effect size expressed with Cohen's d.
- Abbreviations: CG, control group; EG, experimental group; ES, effect size; p, significance; T0, pre-intervention; T1, post-intervention; T2, three months after the intervention. p0, differences between groups; p1, intra-group differences between T0 and T1; p2, intra-group differences between T0 and T2. A36 Haemo-QoL, A36-Haemophilia-Quality of Life Questionnaire; HAL, Haemophilia Activities List; 2MWT, 2-Minutes Walking Test; sec, seconds; STST, sit to stand test; TUG, timed up and go. Statistically significant differences are shown in bold.
Regarding pain (Table 3), at T0 the CG showed better results in VAS and in the ‘Pain’ dimension of A36 Haemo-QoL. No differences were found in T1. At T2, the EG showed significantly better scores than the CG in the ‘Pain’ dimension of A36 Haemo-QoL. When compared to T0, the within-group (T0 vs. T1) analysis showed that the intervention protocol had a significant effect in the EG in the ‘Pain’ dimension of A36 Haemo-QoL, as well as in VAS and in PainDETECT scores. At T2 (T0 vs T2) the intervention effects remained significant in PainDETECT and in the ‘Pain’ dimension of A36 Haemo-QoL.
| T0 | T1 | T2 | p1 [95% CI]; ES | p2 [95% CI]; ES | ||
|---|---|---|---|---|---|---|
| VAS | EG | 4.40 (3.03) | 2.00 (2.31) | 3.50 (3.44) | .008 [.59:4.21]; .79 | .45 [–.69:2.49] |
| CG | 1.78 (1.56) | 1.89 (1.83) | 2.44 (2.51) | 1.00 [–2.02:1.80] | .92 [–2.34:1.01] | |
| p0 [95% CI]; ES | .032 [.25:5.00]; 1.07 | .91 [–1.92:2.15] | .46 [–1.89:4.00] | |||
| Pain-DETECT | EG | 15.70 (7.09) | 9.90 (5.97) | 11.20 (5.39) | .035 [.35:11.25]; .88 | .029 [.39:8.61]; .70 |
| CG | 10.33 (4.15) | 10.11 (6.33) | 10.22 (6.06) | 1.00 [–5.52:5.96] | 1.00 [–4.22:4.44] | |
| p0 [95% CI] | .06 [–.35:11.08] | .94 [–6.17:5.75] | .71 [–4.56:6.52] | |||
| ‘Pain’ dimension of A36 Haemo-QoL | EG | 1.20 (2.15) | 5.40 (2.17) | 7.20 (.92) | <.001 [–6.19:–2.21]; 1.52 | <.001 [–7.59:–4.41]; 2.38 |
| CG | 3.67 (1.94) | 4.33 (1.73) | 3.78 (1.48) | 1.00 [–2.77:1.43] | 1.00 [–1.79:1.56] | |
| p0 [95% CI]; ES | .018 [–4.46:–.48]; 1.20 | .26 [–.85:2.98] | <.001 [2.24:4.60]; 2.81 |
- Data are expressed as mean (standard deviation). CI: confidence interval for the mean difference. The effect size expressed with Cohen's d.
- Abbreviations: CG, control group; EG, experimental group; ES, effect size; p, significance; T0, pre-intervention; T1, post-intervention; T2, three months after the intervention. p0, differences between groups; p1, intra-group differences between T0 and T1; p2, intra-group differences between T0 and T2. A36 Haemo-QoL, A36-Haemophilia-Quality of Life. Statistically significant differences are shown in bold.
Regarding HJHS (Table 4), the between-group analysis showed that at T0 the CG presented better joint health which was maintained in T1 and in T2. Moreover, CG showed better results in T0 on HJHS global gait. When compared to T0, the within-group (T0 vs. T1 and T0 vs. T2) analysis showed that the intervention protocol had a significant effect in the EG in the ‘Joint damage’ dimension of A36 Haemo-QoL.
| T0 | T1 | T2 | p1 [95% CI]; ES | p2 [95% CI]; ES | ||
|---|---|---|---|---|---|---|
| HJHS | ||||||
| HJHS right elbow | EG | 3.40 (4.03) | 3.30 (3.95) | 4.20 (5.05) | 1.00 [–1.54:1.74] | .56 [–2.35:.75] |
| CG | 3.67 (4.47) | 3.67 (3.54) | 3.33 (4.42) | 1.00 [–1.73:1.73] | 1.00 [–1.30:1.96] | |
| p0 [95% CI] | .89 [–4.38:3.85] | .83 [–4.01:3.28] | .70 [–3.75:5.48] | |||
| HJHS left elbow | EG | 6.10 (5.04) | 6.40 (5.66) | 7.40 (5.50) | 1.00 [–1.91:1.32] | .18 [–3.02:.42] |
| CG | 4.33 (6.60) | 4.44 (6.44) | 4.22 (6.96) | 1.00 [–1.82:1.59] | 1.00 [1.70:1.92] | |
| p0 [95% CI] | .52 [–3.88:7.41] | .49 [–3.90:7.81] | .28 [–2.86:9.22] | |||
| HJHS right knee | EG | 9.20 (8.89) | 8.90 (8.66) | 9.90 (8.66) | 1.00 [–.51:1.11] | .46 [–1.94:.54] |
| CG | 3.22 (5.59) | 3.44 (5.22) | 3.33 (5.85) | 1.00 [–1.07:.63] | 1.00 [–1.42:1.19] | |
| p0 [95% CI] | .10 [–1.31:13.27] | .12 [–1.57:12.48] | .07 [–.676:13.81] | |||
| HJHS left knee | EG | 9.00 (9.13) | 8.90 (8.96) | 9.00 (8.82) | 1.00 [–.91:1.11] | 1.00 [–1.15:1.15] |
| CG | 2.44 (4.22) | 2.67 (3.20) | 3.44 (4.98) | 1.00 [–1.28:.84] | .13 [–2.21:.21] | |
| p0 [95% CI] | .07 [–.47:13.58] | .07 [–.44:12.90] | .12 [–1.49:12.60] | |||
| HJHS right ankle | EG | 6.50 (2.64) | 7.00 (2.75) | 7.40 (3.31) | 1.00 [–2.52:1.52] | .71 [–2.84:1.04] |
| CG | 4.11 (2.52) | 4.44 (3.71) | 4.44 (3.36) | 1.00 [–2.46:1.80] | 1.00 [–2.38:1.71] | |
| p0 [95% CI] | .06 [–.12:4.89] | .10 [–.58:5.69] | .07 [–.27:6.19] | |||
| HJHS left ankle | EG | 9.00 (6.67) | 9.60 (6.55) | 9.90 (6.66) | 1.00 [–3.15:1.95] | .77 [–2.94:1.14] |
| CG | 5.78 (6.87) | 5.78 (6.82) | 6.56 (6.09) | 1.00 [–2.68:2.68] | 1.00 [–2.93:1.37] | |
| p0 [95% CI] | .31 [–3.33:9.78] | .23 [–2.65:10.30] | .27 [–2.85:9.54] | |||
| HJHS gait | EG | 3.50 (.97) | 3.20 (1.23) | 3.30 (.95) | .21 [–.11:.71] | .96 [–.32:.72] |
| CG | 1.67 (1.41) | 2.00 (1.73) | 1.78 (1.64) | .17 [–.77:.10] | 1.00 [–.66:.44] | |
| p0 [95% CI]; ES | .004 [.67:3.00]; 1.53 | .10 [–.24:2.64] | .023 [.24:2.80]; 1.15 | |||
| Total score | EG | 46.70 (23.82) | 46.80 (23.41) | 49.90 (24.20) | 1.00 [–6.11:5.91] | .19 [–7.49:1.09] |
| CG | 25.44 (10.42) | 25.78 (10.71) | 27.11 (11.33) | 1.00 [–6.67:6.00] | 1.00 [–6.19:2.85] | |
| p0 [95% CI]; ES | .025 [3.08:39.43]; 1.13 | .025 [3.04:39.01]; 1.12 | .020 [4.13:41.45]; 1.18 | |||
| Dimension of A36 Haemo-QoL | ||||||
| ‘Joint damage’ | EG | 4.90 (3.21) | 9.20 (3.33) | 8.60 (3.60) | .006 [–7.41:–1.19]; .92 | .002 [–6.08:–1.32]; 1.06 |
| CG | 6.89 (1.17) | 7.67 (1.87) | 7.56 (1.42) | 1.00 [–4.06:2.50] | 1.00 [–3.17:1.84] | |
| p0 [95% CI] | .10 [–4.38:.41] | .24 [–1.12:4.19] | .43 [–1.66:3.75] | |||
- Data are expressed as mean (standard deviation). CI: confidence interval for the mean difference. The effect size expressed with Cohen's d.
- Abbreviations: CG, control group; EG, experimental group; ES, effect size; p, significance; T0, pre-intervention; T1, post-intervention; T2, three months after the intervention. p0, differences between groups; p1, intra-group differences between T0 and T1; p2, intra-group differences between T0 and T2. A36 Haemo-QoL, A36-Haemophilia-Quality of Life Questionnaire; HJHS, haemophilia Joint Health Score; ROM, range of motion. Statistically significant differences are shown in bold. .
Finally, at T1, the EG group showed better results than the CG in the ‘Satisfaction with the treatment’ dimension of A36 Haemo-QoL (Table 5), and these differences were maintained in T2. When compared to T0, the within-group (T0 vs. T1 and T0 vs. T2) analysis indicated that the intervention protocol had a significant effect in the EG in the ‘Satisfaction with the treatment’ A36 Haemo-QoL dimension. No within-group differences were found for the CG.
| T0 | T1 | T2 | p1 [95% CI]; ES | p2 [95% CI]; ES | ||
|---|---|---|---|---|---|---|
| Satisfaction with the treatment dimension of A36 Haemo-QoL | EG | 5.90 (1.60) | 8.10 (1.37) | 7.80 (.63) | .006 [–3.80:–.60]; .93 | .002 [–3.11:–.69]; .83 |
| CG | 6.00 (2.12) | 5.67 (2.35) | 5.44 (1.94) | 1.00 [–1.35:2.02] | .79 [–.72:1.83] | |
| p0 [95% CI]; ES | .91 [–1.90:1.70] | .012 [.60:4.27]; 1.28 | .002 [.99:3.72]; 1.68 |
- Data are expressed as mean (standard deviation). CI, confidence interval for the mean difference. The effect size expressed with Cohen's d.
- Abbreviations: EG, experimental group; CG: control group; ES, effect size; p, significance; T0, pre-intervention; T1, post-intervention; T2, three months after the intervention. p0, differences between groups; p1, intra-group differences between T0 and T1; p2, intra-group differences between T0 and T2. A36 Haemo-QoL: A36-Haemophilia-Quality of Life Questionnaire. Statistically significant differences are shown in bold. .
4 DISCUSSION
The present results partly support our hypothesis that the programme would be effective in increasing functionality, pain and joint health in PWH, arthropathy and chronic pain. Also, the patients were satisfied with the treatment.
Regarding self-perceived functionality, changes in HAL were not significant. However, according to Kuijlaars et al.,31 a change of 10.2 points in total HAL score and 16.7 in the basic activities of the lower extremities means a real clinical change in the patient. The improvements found in our study for the EG are close to and higher than the reference values reported by Kuiljaars (10.1 and 24.65, respectively), whilst no changes were observed in CG. In addition, patients in EG reported a significant improvement in quality of life related to functionality measured by A36 Haemo-QoL.
With regard to functional tests, we did not find improvements. Our results are similar to those presented by Hill et al.,32 who used a home-based balance and strength programme and did not obtain significant improvements in the STST, as well as by Boccalandro et al.,33 who found no changes in HAL after physiotherapy and occupational therapy in PWH. In contrast, Calatayud et al.34 showed improvements in TUG and STST, using an elastic band training programme. However, in the latter trial, participants were supervised in all the training sessions and used moderate-vigorous intensities, which could have influenced the results. Otherwise, in the study by Czepa et al.,35 the one-year home-based programme obtained improvements in the 12-minutes-walking-test. Perhaps, if the present programme lasted more than 4 months, we could have found a significant improvement in the 2MWT.
The significant improvements obtained in pain are especially noteworthy if we consider that the EG started from significantly higher levels of pain than the CG and that our sample includes patients with long-standing chronic pain (i.e., EG = 16 years, CG = 10 years). Furthermore, it should be noted that the EG improved the PainDETECT score, from ‘unclear’ neuropathic component in pain to ‘negative’ neuropathic component. Other studies have examined the effects of exercise on pain. Cuesta-Barriuso et al.36 combined a home-based therapeutic exercise programme with education sessions, and obtained improvements in pain compared to a CG. The strength programme proposed by Calatayud et al.34 also reduced pain in PWH. The reduction in pain has generally been attributed to an increase of anti-inflammatory cytokines and a reduction in inflammatory cytokines associated with increased physical activity.37 Other theories show the importance of the release of endogenous opioids, growth factors, activation of supraspinal mechanisms in the modulation of pain perception, increase in body awareness or mechanisms associated with the gate theory.38 On the other hand, García-Dasi et al.9 showed that the combination of CBT with therapeutic exercise intervenes on negative attitudes related to pain and kinesiophobia, whilst reducing chronic pain and improving self-efficacy and emotional status.
In relation to joint health, our study found partial improvements because although no significant changes were found in HJHS, statistically significant improvements were found in the joint damage dimension of A36 Haemo-QoL (EG improved the initial score by 44%). This may be because participants had very deteriorated joint health and that severe arthropathy is not reversible, and because the strengthening exercises were performed in a safe range of motion. These results are in line with those presented by Cuesta-Barriuso et al.,36 where no improvements in joint health were found either. However, it is important to note that, in general, improvements in joint health have only been seen in studies carried out in developing countries, where there is restricted access to clotting factor and a switch to prophylaxis is made at the time of the intervention.39, 40 In contrast, more than half of the participants of our study had previously carried out other exercise programmes and were in prophylaxis regimen. In fact, only 40% of the CG and 33% of the EG had not previously performed any type of exercise.
Finally, in relation to satisfaction with the treatment, the EG improved significantly, and this improvement was maintained 3 months post-intervention. Therefore, patients in the EG showed good acceptance of the protocol.
4.1 Limitations
First, it seems difficult to determine in what proportion each therapy (therapeutic exercise and CBT) has contributed to the results. Therefore, future studies should apply both interventions independently in separate groups, in addition to the combined therapy group. Second, the sample size was small, however, it should be noted that the number of participants recruited was sufficient according to a post hoc power analysis. Third, due to the specific characteristics of the group, the face-to-face sessions, and the participants’ ability to commit to the programme, convenience sampling was carried out and the distribution of the participants in each group, in terms of age and functional status, may have impacted the results. Based on all this, there is a need for multicentre randomised clinical trials with a larger sample size and an evaluation of long-term adherence.
5 CONCLUSIONS
The combined physiotherapy and CBT protocol showed a partial improvement in functionality, pain and joint health of PWH, arthropathy and chronic pain. In addition, participants were satisfied with the treatment.
AUTHOR CONTRIBUTIONS
María García-Dasí, Sofía Pérez-Alenda and Felipe Querol conceived and designed the study. Santiago Bonand provided participants. Marta Aguilar-Rodríguez and Elena Marqués-Sulé conducted the evaluation sessions and María García-Dasí and Noemí Moreno-Segura conducted the intervention group sessions. Juan J. Carrasco analysed the data. Noemí Moreno-Segura, Marta Aguilar-Rodríguez and Sofía Pérez-Alenda drafted the manuscript. All authors reviewed and approved the final version of the paper.
ACKNOWLEDGEMENT
The authors thank the participants for their contribution to the study. This research was supported by an Investigator-Initiated Research (IIR) Award from Pfizer (Study ID: WI221634). Pfizer had no role in the study design, data collection, statistical analysis, interpretation, or writing of the manuscript.
CONFLICT OF INTEREST
The authors stated that they had no interests which might be perceived as posing a conflict or bias.
ETHICS STATEMENT
All procedures were approved by the institution's Review Board (2017/0320) and comply with the requirements listed in the 1975 Declaration of Helsinki and its amendment in 2008.
PATIENT CONSENT STATEMENT
All participants were informed about the purpose and content of the project and gave their written informed consent to participate in the study.
CLINICAL TRIAL REGISTRATION
The study was registered in www.ClinicalTrials.gov (NCT03529474).
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request