Multiple sclerosis – a review
Abstract
Multiple sclerosis (MS) is the commonest non-traumatic disabling disease to affect young adults. The incidence of MS is increasing worldwide, together with the socioeconomic impact of the disease. The underlying cause of MS and mechanisms behind this increase remain opaque, although complex gene–environment interactions almost certainly play a significant role. The epidemiology of MS indicates that low serum levels of vitamin D, smoking, childhood obesity and infection with the Epstein–Barr virus are likely to play a role in disease development. Changes in diagnostic methods and criteria mean that people with MS can be diagnosed increasingly early in their disease trajectory. Alongside this, treatments for MS have increased exponentially in number, efficacy and risk. There is now the possibility of a diagnosis of ‘pre-symptomatic MS’ being made; as a result potentially preventive strategies could be studied. In this comprehensive review, MS epidemiology, potential aetiological factors and pathology are discussed, before moving on to clinical aspects of MS diagnosis and management.
Introduction
Multiple sclerosis (MS) is the commonest non-traumatic disabling disease to affect young adults 1. There is increasing incidence and prevalence of MS in both developed and developing countries 2, the underlying cause of which remains uncertain. MS is a complex disease; many genes modestly increase disease susceptibility in addition to several well defined environmental factors, in particular vitamin D or ultraviolet B light (UVB) exposure, Epstein–Barr virus (EBV) infection, obesity and smoking 3.
Multiple sclerosis has historically been classified as an organ-specific T-cell mediated autoimmune disease. However, the success of B-cell targeted therapies challenges the standard T-cell autoimmune dogma 4. It is traditionally viewed as a two-stage disease, with early inflammation responsible for relapsing–remitting disease and delayed neurodegeneration causing non-relapsing progression, i.e. secondary and primary progressive MS 5, 6.
The emergence of increasingly effective biological therapies and an active approach to treating MS, in particular treating to a target of no evident disease activity (NEDA), are changing the long-term outcome for people with MS (pwMS). More aggressive immune reconstitution therapies, that result in a proportion of pwMS entering long-term remission, offer a small number of pwMS a potential cure 7. Recent positive trials of disease-modifying therapies in progressive MS offer those with more advanced MS the hope of slowing their disease progression, with preservation of residual function 8. The fact that treatments appear to work at multiple stages in the disease course significantly challenges the traditional two-stage view of the natural history of MS 9.
Epidemiology and aetiology
It is often stated that the cause of MS is unknown; however, this is not quite correct. EBV, sunshine (UVB), smoking and vitamin D, combined with an individual's genetic background, play important roles in the causal pathway that results in MS development 10. Migration studies consistently support MS being secondary to an environmental exposure 11. Adult migrants from low risk countries, such as the West Indies, to Europe are at low risk of developing MS; however, children born to migrants in Europe are at high risk. Migration studies indicate that environment trumps genetics and argue strongly for prevention studies targeting known environmental risk factors.
Being truly EBV negative protects from developing MS 12, 13; symptomatic EBV infection (i.e. infectious mononucleosis) doubles the chances of getting MS 14. Evidence regarding the mechanism via which EBV increases MS risk is heterogeneous; molecular mimicry is historically a popular theory 15. More recently EBV-induced B-cell immortalization and/or transformation has been thought to play an important role in disease development 16.
Multiple sclerosis is increasingly a global disease 2. MS prevalence increases with latitude; however, this gradient is decreasing in Norway and the USA, the two countries where it has been studied 17. The latitudinal gradient in MS prevalence is strongly correlated with UVB exposure, which stimulates cutaneous vitamin D (vD) production. Low vD levels, decreased intake of vD, reduced outdoor activity and increased MS susceptibility associated with genetic polymorphisms causing low vD levels have implicated vD in the causal pathway of MS 18.
Multiple sclerosis is more common in females, but this has not always been the case. In case series from the early 1900s the sex ratio was almost equal. Since then, the sex ratio has steadily been increasing and it is now close to 3:1 (F:M) in most developed countries 19. Smoking, which increases MS risk by approximately 50%, can explain up to 40% of the increased incidence of MS in women 20. Prior to the Second World War, few women smoked, but the number of women smoking rapidly increased post-war, mirroring the increasing incidence of MS in women 20. The observation that organic solvents 21 and smoked tobacco 22, but not oral tobacco or snuff 23, are associated with MS has led to the hypothesis that these agents cause post-translational modifications via antigen presentation occurring in the lungs.
It is likely that MS risk modification occurs throughout life, starting in utero 10. The month-of-birth effect and increased concordance in dizygotic twins compared to siblings indicates that the intrauterine environment is important in establishing MS risk; it is unclear whether this is due to common environmental exposures, or epigenetic mechanisms, or both 10. There is a genetic influence on MS susceptibility; about one in eight patients have a family history of MS 24. Concordance in female monozygotic twins approaches 30% in the UK and Canada, but is as low as ~8.5% in southern Europe 25.
The main genetic risk associated with MS resides in HLA-DRB1*15 and/or other loci in strong linkage disequilibrium with this allele 26. Heterozygotes for HLA-DRB1*15:01 have an odds ratio of MS >3 and homozygotes >6 26, yet the mechanism remains unknown. It is hypothesized that HLA-DRB1*15:01's role is via antigen presentation; however, this does not explain the protective effects of class 1 alleles (e.g. HLA-A*02:01) 27.
Genome-wide association studies have identified more than 150 single nucleotide polymorphisms associated with MS susceptibility 28. The odds ratio associated with the majority of these is small, around 1.1–1.2. Many of these single nucleotide polymorphisms lie close to genes associated with immune function, typically in regulatory rather than coding regions. Functional variants identified include those within IL7R 29, IL2RA 30, TNFR1 31, BAFF 32 and CYP2R1 33. Mendelian randomization studies have provided evidence for a role of vitamin D 33-35 and obesity 36 as independent risk factors causing disease.
Recent work has uncovered genetic differences between relapsing–remitting MS (RRMS) and primary progressive MS (PPMS) 37 not previously detected in genome-wide association studies, most probably due to the under-representation of PPMS in these cohorts. Genetic variants associated with other progressive neurological disorders are relatively over-represented in progressive MS 37. Similar genetic risk exists when all MS-associated alleles are taken into account, indicating additional risk for progressive disease superimposed on underlying genetic susceptibility. Evidence of differential gene transcription between RRMS and PPMS 38 again hints at individual differences on a background of shared genetic risk.
Pathology and immunology
In Charcot's original descriptions of the pathology associated with sclérose en plaques, he described ‘sclerosed plaques’ affecting the periventricular area, pons and spinal cord 39. The characteristic pathological hallmark of MS is perivenular inflammatory lesions, leading to demyelinating plaques 40. The inflammatory infiltrates contain T-lymphocytes, dominated by MHC class I restricted CD8+ T-cells; B-cells and plasma cells are also present, although in much lower numbers 41. Oligodendrocyte damage and demyelination occur as a result of inflammation. Axons are relatively preserved in the early stages of the disease; however, as disease progresses irreversible axonal damage develops 42. The ‘classical active lesion’, with profound lymphocytic inflammation, predominates in RRMS. It is seen less commonly in progressive disease, where lesions tend to have an inactive lesion core surrounded by a narrow rim of activated microglia and macrophages 43.
Despite a clinical distinction between RRMS and progressive MS, pathologically defined inflammatory changes are seen in both, albeit to a greater degree in relapsing–remitting disease. The composition of the inflammatory infiltrate in relapsing–remitting and progressive MS is similar, although the proportion of B-cells and plasma cells is higher in progressive MS 44. Whether the cytokine profile or activation stage of T-cells and B-cells differs between clinical disease types remains unclear 41.
Remyelination is seen in all disease stages, most commonly in progressive disease 41. Patients with secondary progressive MS have higher levels of demyelination and a reduction in axonal density in the normal appearing white matter in the cervical spinal cord in PPMS 45. There is no single characteristic histological difference between MS subtypes, but instead a difference in the proportion of areas showing particular characteristics. Thus, whilst three clinical forms of MS have been defined, the pathological changes form a continuum. This fits with gradual clinical disease evolution in patients, from RRMS to secondary progressive MS over a period of years.
Clinical features
Multiple sclerosis is a journey from being at risk, through the asymptomatic, prodromal and symptomatic phases of the disease. MS is typically suspected when a person presents with a clinically isolated syndrome (CIS). This can be mono- or poly-symptomatic depending on the location of the eloquent lesion(s). The most commonly seen presentations are optic neuritis, brainstem and spinal cord syndromes; however, numerous other less common presentations exist, including cortical presentations such as dominant parietal lobe syndromes.
Multiple sclerosis relapses usually develop subacutely over hours to days, reach a plateau lasting several weeks, and then gradually recover. Gross clinical recovery from relapses often appears complete in early MS; however, most relapses leave behind some damage. For example, following acute optic neuritis gross visual acuity may recover but colour vision, contrast sensitivity and depth perception abnormalities persist. As neuronal reserve is lost, recovery from relapses becomes incomplete, and neurological deficits accrue leading to sustained disability.
For every clinical attack, approximately 10 ‘asymptomatic’ lesions are noted on magnetic resonance imaging (MRI). Symptomatology results from a combination of location and size – a small lesion in an eloquent area is likely to cause symptoms. Macroscopic, or MRI-visible, lesions are the tip of the iceberg; many more lesions can be seen at microscopic level and even more in deep and cortical grey matter.
Secondary progressive MS typically develops 10–15 years after RRMS onset, with a gradual evolution from discrete relapses to slowly progressive disease. There is not a distinct transition between disease types; rather, relapses occur on a background of subtle progression, prior to progression being dominant. The cognitive impairment and progressive MRI atrophy seen in early MS indicate that neurodegeneration is present from clinical onset.
In 5%–15% of cases there is a primary progressive onset (PPMS), typically with gradual accrual of progressive disability involving one dominant neuronal system. The commonest presentation is with a progressive spastic paraparesis, but sensory ataxia, cerebellar ataxia and cognitive and progressive visual failure are well-described PPMS variants.
There has been a reduction in the proportion of people with PPMS 46. This is probably related to the fact that there are no licensed treatments for PPMS; patients may be labelled as having relapsing MS in order to receive treatment, raising ethical questions about the division of MS into distinct subtypes. This artificial division of MS into different diseases was driven by the pharmaceutical industry to get interferon beta licensed under the Orphan Drug Act in the USA.
Paediatric MS is considerably rarer than adult onset disease, with a highest reported incidence of 2.9/100 000 47. The diagnosis is based on repeated episodes of demyelination separated by time and space. Differentiating paediatric MS from acute disseminated encephalomyelitis can be challenging, as paediatric MS may be multifocal at onset 47. Relapse rates may be higher, but physical recovery tends to be more complete. Few treatments are licensed for use in children, and referral to a paediatric neurologist with expertise in demyelinating disorders is recommended where the diagnosis is suspected.
Given the above, MS can be thought of as a single disease existing within a spectrum extending from relapsing (‘inflammatory dominant’) to progressive (‘neurodegeneration dominant’), in keeping with the 2013 revisions to the clinical course of MS 48. At present, MS definitions place artificial distinctions between patients with progressive and patients with relapsing disease. Instead, these subtypes should be seen as points on a continuum of disease, which should be expanded to include prodromal (i.e. radiologically isolated) disease.
Preclinical disease and the at-risk population
Multiple sclerosis has an at-risk period prior to preclinical and clinical phases 49. Migration studies indicate that the time from exposure to environmental risk factors and the onset of disease is 10–20 years 49. Pathological studies indicate that the preclinical phase of MS could be decades; a Danish series found that a quarter of cases with postmortem pathological evidence of MS were never diagnosed with MS in life 50.
Multiple sclerosis begins before the first clinical attack; most patients presenting with a CIS have older, inactive, lesions on their MRI. Radiologically isolated syndrome (RIS), or asymptomatic MS, is detected on an MRI done for unrelated reasons, such as headache, head injury or screening in the airline industry. Even in these earliest stages there is evidence of end-organ damage. MRI in young people with CIS shows brain volume loss compared to controls 51. School performance in children who later develop MS is poorer than their peers 52, and a quarter of patients with RIS have significant cognitive impairment with a profile similar to patients with established MS 53. This appears to indicate that not only is inflammation present prior to diagnosis, but there is accompanying neurodegeneration from the start.
It is predicted that MS has the potential to become a model neurodegenerative disease, setting the stage for pre-symptomatic diagnosis for other neurodegenerative diseases, in particular Alzheimer's and Parkinson's disease. The big question is whether society is ready for population screening and pre-symptomatic diagnosis. At some point in time it is going to be necessary to accept that, to have a meaningful impact on the burden associated with neurodegenerative disease, these conditions are going to have to be diagnosed in the pre-symptomatic phase.
Important differential diagnoses
Table 1 lists the most common MS differential diagnoses or mimics. Red flags include a first relapse at an older age, where vascular disease is more likely. Non-specific white matter lesions may be seen in patients with no objective persisting neurological disability and history of migraine, although migraine is more common in the MS population 54. In those from low prevalence areas and/or ethnic minorities, differential diagnoses must be carefully considered, as neurosarcoidosis, neuromyelitis optica spectrum disorder and infections such as tuberculosis are more likely, and MS-specific disease-modifying therapy may cause a worsening of these diseases.
| Clinical presentation | Differential diagnosis | Relevant aspects and investigations to consider |
|---|---|---|
| Monosymptomatic | ||
| Acute optic neuritis (ON) | Neuromyelitis optica (NMO) | Often associated with severe visual loss. May be bilateral rapidly sequential ON. AQ4 and MOG antibodies. Possible additional MRI lesions in area postrema or diencephalon |
| Leber hereditary ON | Genetic testing | |
| Toxic/nutritional ON | Clinical history, alcohol and tobacco use. B12, methylmalonic acid and/or plasma homocysteine | |
| Non-arteritic ischaemic ON | Age – usually in older patients. Clinical history and examination; vascular risk factors | |
| Arteritic ischaemic ON | Age – usually occurs in patients aged >70. Autoimmune/ANA screen, ESR | |
| Transverse myelitis (TM)/spinal cord syndrome | Neuromyelitis optica (NMO) | Consider if long segment transverse myelitis (>3 segments) involving much of the central spinal cord with oedema and gadolinium enhancement. Additional MRI lesions in area postrema or diencephalon. May have previous ON. AQ4 and MOG antibodies |
| TM associated with systemic autoimmune disease | May have systemic features or clinical history of autoimmune disease (rash, renal involvement, dry eyes etc.). ANA screen, ESR | |
| Anterior spinal artery occlusion | Sudden, catastrophic onset with anterior spinal cord syndrome. Usually older patients and/or those with vascular risk factors. MRI may differentiate with bilateral anterior involvement in watershed mid thoracic area typical | |
| Arteriovenous fistula/malformation | Stepwise onset, mixed upper and lower motor neurones. MRI and/or spinal angiography may make the diagnosis with dilated and/or tortuous dural veins seen | |
| Radiation myelopathy | Clinical history, MRI may show vertebral changes | |
| B12/folate deficiency | Clinical history of dietary insufficiency and/or nitrous oxide inhalation. FBC/serological changes may coexist. May have additional optic neuropathy and/or peripheral nerve involvement. Long segment changes in dorsal columns on MRI. Serum B12 and plasma homocysteine/methylmalonic acid levels | |
| Copper deficiency | Clinical history of gastrectomy or excessive zinc intake. Long segment changes in dorsal columns on MRI. Serum copper levels diagnostic | |
| Brainstem | Ischaemic event (stroke, transient ischaemic attack) | Clinical history, age – usually in older patients. MRI and CSF may help differentiate |
| Space occupying lesion | More gradual onset. MRI can differentiate | |
| Migraine | More rapid resolution; may have severe headache. MRI can help differentiate | |
| Brainstem encephalitis (Bickerstaff's) | Patients may be encephalopathic and/or obtunded. MRI and CSF can help differentiate | |
| Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) | Clinical history – may have peripheral nerve involvement in brainstem | |
| Polysymptomatic | Migraine | More rapid resolution; may have severe headache. MRI can help differentiate |
| Ischaemic event (stroke, transient ischaemic attack, small vessel disease) | Clinical history, age – usually in older patients. MRI and CSF may help differentiate | |
| Cerebral autosomal dominant arteriopathy with cortical infarcts and leukoencephalopathy (CADASIL) | Family and clinical history – typically migraine, stroke-like events and prominent cognitive involvement. MRI can show typical appearances. NOTCH-3 mutation testing diagnostic | |
| Sarcoidosis | May have multisystem involvement – CT chest may help. OCBs often negative in CSF | |
| Systemic autoimmune disease | May have systemic features or clinical history of autoimmune disease (rash, renal involvement etc.). ANA screen, ESR, Ro/La, SCL-70 | |
| Primary CNS vasculitis | Patients often encephalopathic. MRI shows small ischaemic (rather than inflammatory) lesions. MRI angiography can be helpful | |
| Susac's syndrome | Clinical history of encephalopathy, deafness and/or visual impairment may be present – most patients do not have complete triad at presentation. Branch retinal infarcts on fundoscopy. Characteristic callosal lesions on MRI. Fluoroscein angiography mandatory if diagnosis suspected | |
| Neuro-Behçet's | Systemic and/or additional CNS features – venous sinus thrombosis and meningitis. Associated with HLA-B5 | |
| Acute disseminated encephalomyelitis (ADEM) | Acute polysymptomatic onset, often post-viral. MRI shows large demyelinating lesions all of similar age with gadolinium enhancement but without T1 black holes at presentation | |
| Progressive disease | Spinal cord compression by disc, tumour, syrinx etc. | MRI |
| Progressive metabolic myelopathy | Clinical history, copper/B12 levels, MRI | |
| Genetic progressive spastic paraparesis/cerebellar ataxia (HSP, SCA) | Family and clinical history, relevant genetic test | |
| Leukodystrophies | Very long chain fatty acids (especially in males) and white cell enzymes | |
| Infectious causes – HTLV and HIV | Clinical (+/− family history), HTLV-1 and HIV serology | |
- ANA, antinuclear antibody; AQ4, aquaporin-4; CNS, central nervous system; CSF, cerebrospinal fluid; CT, computed tomography; ESR, erythrocyte sedimentation rate; FBC, full blood count; HIV, human immunodeficiency virus; HSP, hereditary spastic paraparesis; HTLV, human T-cell lymphotropic virus; MOG, myelin oligodendrocyte glycoprotein; MRI, magnetic resonance imaging; NMO, neuromyelitis optica; OCB, oligoclonal band; ON, optic neuritis; SCA, spinocerebellar ataxia; TM, transverse myelitis.
Another red flag is comorbid systemic symptoms and signs; this should alert clinicians to exclude multisystem diseases such as systemic lupus erythematosus, Sjögren's, Behçet's, Susac's and other vasculitides. MS can coexist with other autoimmune diseases, and so the presence of these does not necessarily exclude MS, and the overall clinical picture must be carefully considered.
A diagnostic lumbar puncture is advised in all patients presenting with possible MS. Cerebral spinal fluid (CSF) analysis is helpful in both identifying MS mimics and either supporting or arguing against a diagnosis of MS. Central nervous system (CNS) synthesis of oligoclonal immunoglobulin G bands or oligoclonal bands (OCBs) can now be used to establish dissemination in time; it is hoped that this will lead to a renaissance in the use of CSF for diagnostic, prognostic and treatment response purposes.
Investigations
The diagnosis of MS remains clinical. However, treatable mimics should be excluded using paraclinical investigations where indicated. All patients with suspected MS should have a lumbar puncture to help support the clinical diagnosis of MS, exclude MS mimics and to help establish a baseline prognostic profile.
Serological investigations
A standard baseline profile should include anti-nuclear antibody, vitamin B12 and thyroid function. Syphilis and human immunodeficiency virus 1 serology are recommended. Depending on the clinical presentation human T-cell lymphotropic virus 1 and 2 serology, anti-aquaporin-4 and anti-myelin oligodendrocyte glycoprotein antibody screening may be indicated.
Magnetic resonance imaging
All patients should undergo MRI imaging of at least the brain and, if the presentation is spinal, imaging should include the spinal cord. Imaging has a dual purpose – it can help to confirm the diagnosis by demonstrating dissemination in both time and space, but it can also exclude MS mimics when interpreted by an experienced neuroradiologist. Approximately 2% of non-MS-related abnormalities picked up on MRI are incidental findings, e.g. pituitary adenomas, pineal cysts, vascular malformations, benign meningiomas and prolapsed intervertebral discs. These incidental findings may clinically complicate things but should not distract from diagnosing MS. Visual, auditory and sensory evoked potentials and central motor conduction times can establish dissemination in space, and demonstrating slowed conduction in patients with equivocal clinical signs and MRI appearances can be useful; however, they may not add much clinical value. The corollary is that normal electrophysiology can be helpful in actively excluding or undiagnosing MS, a clinical problem that is much more common than often realized.
Table 2 summarizes the latest set of diagnostic criteria for RRMS 55. As with previous renditions, they have limitations in their clinical implementation. Using baseline OCBs to provide evidence of dissemination in time means that many patients previously diagnosed with CIS now meet the diagnostic criteria for MS. This could create significant problems in clinical practice, as guidelines for treatment typically mandate a clinico-radiological diagnosis of MS – reclassified patients may acquire a label of MS but remain ineligible for treatment until a second clinical attack or MRI lesion.
| MacDonald 2010 (relapsing–remitting MS) | MacDonald 2017 (relapsing–remitting MS) | |
|---|---|---|
| DIS | Either | Either |
| (i) Objective clinical evidence of ≥2 lesions or objective clinical evidence of 1 lesion with reasonable historical evidence of a prior attack involving a different CNS site or | (i) Objective clinical evidence of ≥2 lesions or objective clinical evidence of 1 lesion with reasonable historical evidence of a prior attack involving a different CNS site or | |
| (ii) ≥1 T2 lesion in at least 2 of 4 MS-typical regions of the CNS (periventricular, juxtacortical, infratentorial, spinal cord); symptomatic lesions in patients with brainstem or spinal cord syndromes are excluded | (ii) ≥1 T2 lesion in at least 2 of 4 MS-typical regions of the CNS (periventricular, juxtacortical, infratentorial, spinal cord) | |
| DIT | Either | Either |
| (i) ≥2 attacks separated by at least 1 month or | (i) ≥2 attacks separated by at least 1 month or | |
| (ii) simultaneous presence of asymptomatic gadolinium-enhancing and non-enhancing lesions at any time or | (ii) simultaneous presence of asymptomatic gadolinium-enhancing and non-enhancing lesions at any time or | |
| (iii) a new T2 and/or gadolinium-enhancing lesion on follow-up MRI irrespective of its timing with reference to a baseline scan | (iii) a new T2 and/or gadolinium-enhancing lesion on follow-up MRI irrespective of its timing with reference to a baseline scan or | |
| (iv) demonstration of CSF-specific OCBs (as a substitute for DIT) |
| MacDonald 2010 criteria for primary progressive MS | |
|---|---|
| (i) 1 year of disease progression (retrospectively or prospectively determined) and | |
| (ii) 2 out of 3 of | Evidence of DIS in the brain based on ≥1 T2 lesion in at least one area characteristic for MS (periventricular, juxtacortical, infratentorial) and/or |
| evidence of DIS in the spinal cord based on ≥2 T2 lesions in the cord and/or | |
| positive CSF (OCBs on isoelectric focusing and/or elevated IgG index) | |
- CNS, central nervous system; CSF, cerebrospinal fluid; DIS, dissemination in space; DIT, dissemination in time; IgG, immunoglobulin G; MRI, magnetic resonance imaging; MS, multiple sclerosis; OCB, oligoclonal band.
Some would argue that these criteria do not go far enough as they do not include a diagnosis of ‘asymptomatic MS’. Patients diagnosed as having RIS are not eligible for treatment. This is troubling as a proportion of these subjects already have evidence of end-organ damage with brain atrophy and cognitive impairment. Approximately 30% go on to develop MS within 5 years 56, and it may be possible to prevent some, or even all, of these patients from developing clinically apparent neurological disease with early interventions. Based on the biological understanding of MS, early and effective treatment with a disease-modifying therapy will have benefits for individual patients.
The role of MRI in establishing prognosis and treatment response is wide ranging. Traditionally, lesion accrual/count together with ‘active’ lesions (gadolinium-enhancing) has been used to estimate disease activity; however, correlation with long-term outcomes is imperfect. The importance of brain atrophy seen on volumetric MRI is increasingly realized, as when taken alongside lesion load there is good correlation with long-term clinical outcomes 57.
High field and double inversion MRI techniques have enabled the visualization of cortical MS lesions, the presence and number of which appear to correlate with clinical outcomes, most notably cognitive impairment 58. Newer MRI techniques, including magnetization transfer imaging, diffusion tensor imaging and functional MRI are providing insights into disease with widespread abnormalities outside of focal lesion development 59; however, these techniques are not yet in routine clinical practice.
Treatment and management of MS
The treatment of MS can be divided into disease-modifying therapies that tend to be MS-specific and symptomatic therapies that are often used in different disease areas to treat symptoms resulting from neurological dysfunction.
Disease-modifying therapies
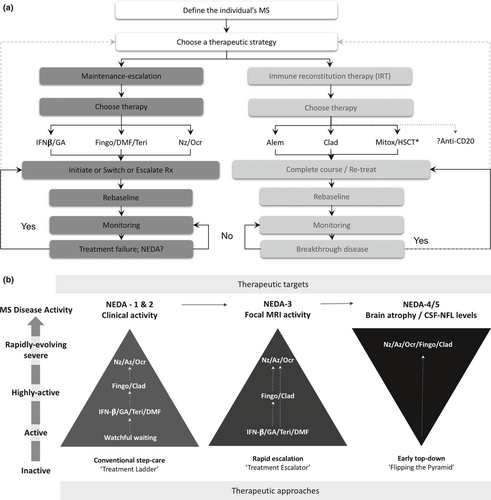
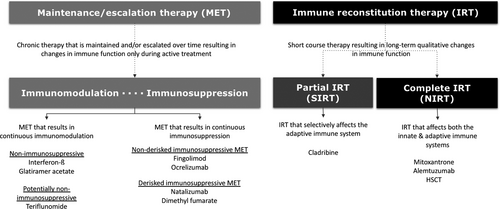
As the number, and efficacy, of disease-modifying therapies has increased, interest in early treatment of MS in order to prevent long-term disability has grown. Historically, treatments have been immunosuppressant (including fingolimod, natalizumab, ocrelizumab) or immunomodulatory (such as interferon beta, glatiramer acetate, teriflunomide), meaning that ongoing treatment is required to maintain suppression of inflammation (and disease activity). Immune reconstitution therapies (including alemtuzumab and cladribine) can be given as short courses with the aim of producing enduring immunological actions – this is at present the closest to a potential cure for MS. This raises the question as to whether early, or even pre-symptomatic, treatment can prevent clinically apparent disease (Figs 1 and 2, Table 3).
| Trade name | Mechanism of action | Efficacy | Route of administration | Main adverse effects | Monitoring requirements | |
|---|---|---|---|---|---|---|
| First line injectable therapies | ||||||
| IFN-beta 1a and 1b | Avonex, Rebif, Betaseron, Betaferon, Extavia | Immunomodulatory, pleiotropic immune effects | Moderate | Variable and depends on formulation | Injection site reactions, flu-like symptoms, abnormal LFTs, lymphopaenia, leukopaenia |
Baseline: FBC, U&E, LFTs, TFTs, SPE, urine protein Follow-up: 1-month, 3-month, 6-month and 6-monthly FBC, U&E and LFTs. TFTs 12 monthly. NABs 12 and 24 months |
| Peg-IFN-beta-1a | Plegridy | Pegylated (long-circulating half-life). Immunomodulatory, pleiotropic immune effects | Moderate | Prefilled syringe 125 μg SC 2 weekly | Injection site reactions, flu-like symptoms, abnormal LFTs, lymphopaenia, leukopaenia |
Baseline: FBC, U&E, LFTs, TFTs, SPE, urine protein Follow-up: 1-month, 3-month, 6-month and 6-monthly FBC, U&E and LFTs. TFTs 12 monthly. NABs 12 and 24 months |
| Glatiramer acetate | Copaxone | Immunomodulatory, pleiotropic immune effects | Moderate | Prefilled syringe 20 mg SC daily or 40 mg SC three times weekly | Injection site reactions, lipoatrophy, flushing reactions | None required |
| Oral immunomodulatory therapies | ||||||
| Dimethyl fumarate | Tecfidera | Pleotropic, NRF2 activation, downregulation of NFκB | Moderate/high | 240 mg twice daily PO | Flushing, gastrointestinal symptoms (dyspepsia, cramps and diarrhoea), lymphopaenia, abnormal LFTs, proteinuria, PML |
Baseline: FBC, U&E, LFTs, urine protein Follow-up: FBC and urine protein 3 monthly for a year, then 6 monthly |
| Teriflunomide | Aubagio | Dihydro-orotate dehydrogenase inhibitor (reduced de novo pyrimidine synthesis), anti-proliferative | Moderate | 7 or 14 mg daily PO (7 mg dose only licensed in the USA) | Hair thinning, gastrointestinal symptoms (nausea, diarrhoea), abnormal LFTs, leukopaenia |
Baseline: BP, FBC, U&E, LFTs, urine protein Follow-up: fortnightly LFTs for 6 months then every 8 weeks. Weekly LFT if ALT 2–3 × ULN. 3-monthly FBC for 1 year then 6 monthly |
| Oral immunosuppressive therapy | ||||||
| Fingolimod | Gilenya | Selective sphingosine 1-phosphate modulator, prevents egress of lymphocytes from lymph nodes | High | 0.5 mg daily PO | Bradycardia (first dose), hypertension, bronchospasm, lymphopaenia, abnormal LFTs, infections, basal cell carcinoma, macular oedema, opportunistic infections (PML, cryptococcosis etc.) |
Baseline: BP, FBC, U&E, LFTs, TFTs, serum immunoglobulin levels, serology (VZV, HIV 1 and 2, hepatitis B and C, syphilis), interferon gamma assay for tuberculosis (or similar), electrocardiogram Follow-up: 3-monthly FBC, U&E and LFTs. TFTs 12 monthly. Optical coherence tomography at 3 months for macular oedema |
| Intravenous immunosuppressive therapies | ||||||
| Natalizumab | Tysabri | Anti-VLA4, selective adhesion molecule inhibitor | Very high | 300 mg IV 4 weekly | Infusion reactions, PML |
Baseline: FBC, U&E, LFTs, JCV serology Follow-up: LFTs 3 monthly for a year. NABs at 12 months. JCV serology 6 monthly |
| Ocrelizumab | Ocrevus | Anti-CD20, B-cell depleter | Very high | Initially 300 mg IV, followed 2 weeks later by second dose of 300 mg IV. Subsequent dosing 600 mg IV 6 monthly | Infusion reactions, infections, possible hypogammaglobulinemia with prolonged use |
Baseline: FBC, U&E, LFTs, TFTs, serum immunoglobulin levels, serology (VZV, HIV 1 and 2, hepatitis B and C, syphilis), TB elispot, cervical smear Follow-up: annual serum immunoglobulin levels |
| Induction/immune reconstitution therapies | ||||||
| Alemtuzumab | Lemtrada | Anti-CD52, non-selective immune depleter | Very high | 12 mg IVI × 5 days year 1, 12 mg IVI × 3 days year 2 | Infusion reactions, infections, opportunistic infections, leukopaenia, secondary autoimmunity (thyroid, immune thrombocytopenic purpura, renal etc.) |
Baseline: FBC, U&E, LFTs, TFTs, serum immunoglobulin levels, serology (VZV, HIV 1 and 2, hepatitis B and C, syphilis), TB elispot, cervical smear Follow-up (for 48 months after last course): monthly FBC, U&E and urine analysis and 3-monthly TFTs |
| Cladribine | Mavenclad | Deoxyadenosine (purine) analogue, adenosine deaminase inhibitor, selective T- and B-cell depletion | High | 10 mg tablets: cumulative dose of 3.5 mg/kg over 2 years. Tablets given for 4–5 days in months 1 and 2 in year 1 and the cycle is repeated in year 2 (8–10 days of treatment per year) | Lymphopaenia, infections (in particular herpes zoster) |
Baseline: FBC, U&E, LFTs, TFTs, serum immunoglobulin levels, serology (VZV, HIV 1 and 2, hepatitis B and C, syphilis), TB elispot, pregnancy test and cervical smear. Follow-up: FBC 2 and 6 months after start of treatment in each treatment year |
| Mitoxantrone | Novatrone | Immune depleter (topoisomerase inhibitor) | Very high | 12 mg/m2 IVI 3 monthly for 2 years; maximum dose of 140 mg/m2 | Leukopaenia, hair loss, nausea, vomiting, infections, cardiomyopathy, amenorrhoea |
Baseline: FBC, U&E, LFTs, TFTs, SPE, serum immunoglobulin levels, serology (VZV, HIV 1 and 2, hepatitis B and C, syphilis), TB elispot Follow-up: 3-monthly (predosing) FBC, U&E and LFTs. TFTs 12 monthly |
| Autologous haematopoietic stem cell transplantation | Autologous stem cell transplantation using standard haematology protocols | Very high | According to local protocols | Adverse events related to induction chemotherapy | Dictated by haematology protocols | |
- ALT, alanine aminotransferase; BP, blood pressure; FBC, full blood count; HIV, human immunodeficiency virus; IV, intravenous; IVI, intravenous infusion; JCV, John Cunningham virus; LFT, liver function test; MS, multiple sclerosis; NABs, neutralizing antibodies; NFκB, nuclear factor kappa-light-chain-enhancer of activated B cells; PML, progressive multifocal leukoencephalopathy; PO, oral; SC, subcutaneous; SPE, serum protein electrophoresis; TFT, thyroid function test; U&E, urea and electrolytes; ULN, upper limit of normal; VZV, varicella zoster virus.
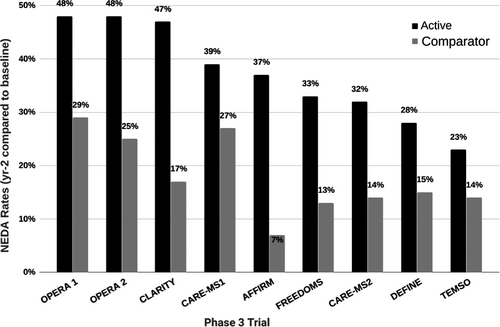
A recent concept in the treatment of MS is ‘no evidence of disease activity’, or NEDA. This has developed from the understanding that clinical relapses are only the tip of the iceberg in terms of MS disease activity. Ongoing inflammatory MRI activity occurs in excess of clinical relapses; in addition, brain atrophy can progress in the absence of overt inflammatory disease activity. NEDA is defined by clinical parameters (NEDA-1 and -2 – absence of relapses and clinical disease progression), inflammatory MRI activity (NEDA-3) and MRI atrophy and biomarkers (NEDA-4 and -5 – CSF neurofilament levels). In clinical practice, this has led to treatment escalation earlier in disease, or early treatment with highly active therapies as first line (Figs 1b and 3).
Given that MS is most commonly diagnosed in young women, pregnancy and family planning are real concerns for women with MS. Current evidence suggests that pregnancy does not increase the risk of long-term disability in MS. However, it is also important that disease-modifying treatment is not unduly delayed, especially in those with active disease. European guidelines briefly discuss issues around pregnancy 60, and UK consensus guidelines are currently in press.
Symptomatic treatments
Symptomatic therapies refer to pharmaceutical and physical therapies that target symptoms arising as a result of CNS damage. In general terms, these treatments are not MS-specific. They include anticholinergics for bladder dysfunction (which may contribute to cognitive impairment, necessitating an individualized approach) and medication for neuropathic pain (typically tricyclic antidepressants, or gabapentin and derivatives). Treating cognitive impairment in MS is complex and centres around the avoidance of possible contributors. Several symptomatic therapies have been licensed specifically for MS. These include sativex for spasticity and fampridine for walking difficulties. An important aspect related to symptomatic therapies is sleep. The prevalence of difficulties with sleeping increases as MS disease duration increases, and anxiety, depression and fatigue are more common in those reporting poor sleep 61. A detailed review of these is beyond the scope of this paper.
Treatment of comorbidities contributing to long-term disability
Multiple sclerosis reduces the brain and cognitive reserve that delays the onset of age-related neurodegenerative disorders in later life. This may explain a component of the age-related progression in older patients with MS.
Patients with comorbid disease, in particular vascular disease and smoking, have a poorer outcome with more rapidly progressive disease 22. Recurrent infections such as urinary tract infections may not only result in transient worsening of MS-related symptoms but could upregulate mechanisms known to speed up worsening disability.
Although the evidence supporting lifestyle and wellness modifications in MS is weak, the value of these for general health is important. Patients who exercise do better than those who do not. Patients should be encouraged to have four to five aerobic exercise sessions per week. They should avoid vigorous exercise during relapse, as this may cause excessive energy demands on an already compromised pathway and theoretically could increase neuroaxonal loss. In patients with significant disability, a bespoke exercise programme should be designed to allow them to exercise, which is best done in conjunction with a physiotherapist with experience in neurodisability.
Despite numerous claims about dietary interventions in MS there are no randomized controlled trials to suggest that one diet is superior to the others. Patients should adopt a healthy eating pattern that is compatible with their culture; their diet should avoid processed foods, in particular sugar and other processed carbohydrates. The World Health Organization recommends that no more than 5% of dietary calories should be consumed as sugar. In general, a varied diet rich in unprocessed foods is recommended.
Future prospects
By refinement of the MS phenotype, through both expansion to include prodromal cases and extension of disease into a single entity rather than artificially separated disease states, the illness in question can be better understood and treated. At present, disease-modifying treatments are only available to people with clinically relapsing forms of the disease and a minority of those with progressive disease – those showing high levels of inflammatory disease on MRI.
By better understanding MS as a disease continuum, it can be seen that there is potential for treatment effects in all MS subtypes. Clinical trial outcome measures for relapsing disease are relatively easy to define; in those patients with progressive disease, clinically measurable rate of change is slow and measuring impact on this already slow rate requires more sensitive outcome measures than are in current use. Patients with progressive disease have historically been denied treatment on the basis of negative clinical trials; if the outcome measures used in these trials are insufficiently sensitive to measure treatment effects then it is our responsibility as physicians to develop outcome measures with better sensitivity, rather than artificially separate disease subtypes.
The fact that aetiological factors implicated in MS development have the potential to be modified prior to disease development opens the door to the potential for preventive trials. However, these would need to be enriched for a high-risk population group and will take many years to set up. In the meantime, early treatment of those at risk of long-term disability is needed in order to minimize the physical morbidity associated with MS.
Acknowledgements
GG would like to thank the National MS Society and the MS Society of Great Britain and Northern Ireland for their financial support and the team at Barts-MS for their support and hard work. RD is supported by grants provided by Barts Charity and the MS Society of Great Britain and Northern Ireland. This work was supported by the Preventive Neurology Unit, Wolfson Institute of Preventive Medicine, QMUL and Blizard Institute, Barts and the London School of Medicine and Dentistry, Queen Mary University London.
Disclosure of conflicts of interest
RD has received funding to attend educational events from Biogen, Sanofi-Genzyme and Teva, and honoraria from Biogen, Teva and Celgene. GG has received compensation for participating on Advisory Boards in relation to MS clinical trial design, trial steering committees and data and safety monitoring committees in the last 5 years from Abbvie, Attara Bio, Biogen, Sanofi-Genzyme, Genentech, GSK, Merck-Serono, Merck, Novartis, Roche, Synthon BV, Teva and UCB Pharma. In the last 5 years his institution has received educational or research grants from Biogen, Sanofi-Genzyme, Merck, Novartis, Roche and Teva.




