Diagnosis and management of transverse root fractures
This article is being published concurrently in Journal of Endodontics. The articles are identical. Either citation can be used when citing this article.
Abstract
Background
Root fractures are not a common injury, but a thorough understanding of their etiology, healing responses, diagnosis, management, and prognosis is essential.
Review
The prognosis is largely related to the patient’s age; degree of displacement, if any, of the coronal fragment; and the location and orientation of the fracture. The more apical the fracture is located, the better the prognosis. Teeth with root fractures located supracrestally may have the worst prognosis, but their management and outcome depend on many factors, with the most influential factor being the ability to restore the tooth because the coronal fragment usually needs to be removed. In contrast, root fractures located in the apical and middle thirds and those subcrestally in the coronal third of the root have a good prognosis and usually require little, if any, treatment apart from immediate repositioning (if the coronal fragment has been displaced) and stabilization. Monitoring of root-fractured teeth over time is essential to determine the healing response and to assess whether the pulp survives or not. In some cases, the pulp in the coronal fragment may necrose and become infected, thus requiring root canal treatment, but this should only be done to the fracture line. Pulp necrosis and infection typically occur within the first 3-4 months if it is a direct result of the trauma. However, pulp necrosis and infection can also occur many years later, in which case it is likely to be a result of bacterial penetration via cracks or breakdown of restorations.
Conclusion
Overall, root fractures should be managed conservatively unless they are located supracrestally.
Significance
Transverse, or horizontal, root fractures are uncommon, but as with all dental injuries, they require appropriate management, which in turn requires a thorough understanding of the injury. This article discusses the classification, diagnosis, tissue responses to, and prognosis of transverse root fractures. The management of transverse root fractures depends on many factors, particularly the level of fracture in the root. Conservative management should be the first approach unless the fracture is located supracrestally.
1 INTRODUCTION
Root fractures are defined as a fracture of a tooth that involves the dentin, cementum, and pulp.1 Root fractures may occur in any direction or orientation, and they are generally classified as vertical fractures (usually also involving the crown) or transverse (often called horizontal) root fractures. Vertical fractures will not be discussed in this article because these injuries usually require extraction of the tooth and replacement with a prosthesis. Although the other group of fractures are commonly called transverse or horizontal root fractures, it is important to understand that such fractures can occur as oblique fractures with varying orientations (eg, more apical toward the palatal surface, more apical toward the labial surface, and so on). In the interest of simplicity in this article, the general term root fracture is used to discuss transverse, horizontal, and oblique fractures. The aim of this article was to review the relevant literature regarding such root fractures in the permanent dentition and to provide guidelines for their management.
Root fractures are not a very common injury to the teeth, with studies reporting the proportion of root fractures among all dental injuries ranging from 1.2% to 7.0% in the permanent dentition.1-6 Some studies regarding the incidence of dental injuries have not reported any root fractures although it is not clear whether they did not occur or they were just not considered in the study design, such as retrospective studies in which only clinical examinations were performed and radiographs were not taken.7, 8 It is also possible that some root fractures may not be diagnosed at the time of initial trauma management because they can only be seen via radiographic imaging techniques and at times the fracture may not be evident immediately after the accident if there has not been any displacement of the coronal fragment. Hence, if adequate radiographs and/or computed tomographic scans are not taken and if the teeth are not regularly reviewed in the early posttrauma period, then root fractures may remain undetected. Notwithstanding this, a root fracture is a significant injury that requires dentists to have a thorough understanding of the mechanisms that lead to this type of fracture, the tissue responses to the fracture, the management options for the different types of root fractures, and the prognosis of these injuries.
Root fractures are a result of direct trauma to a tooth when there is a horizontal, frontal impact, usually with a hard object or during a fight.1, 9 Small and sharp objects concentrate the force of impact to a smaller area on the tooth, and this typically causes a fracture rather than displacement of the tooth. If the root is the site of impact, then a root fracture is likely to occur. If a hard but blunt object strikes the crown of the tooth, the increased area of resistance to the force in the crown causes the force of the impact to be transmitted to the tooth root, resulting in a root fracture, which is most likely to occur in the coronal (cervical) third of the root.1
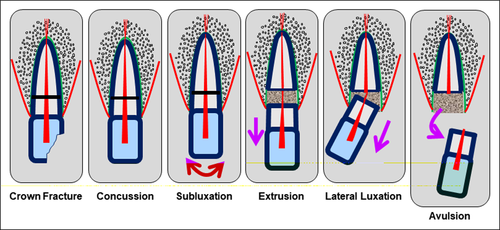
Root fractures may occur as a concurrent injury with another injury to the same tooth and specifically to the coronal fragment of the root (ie, the fragment coronal to the root fracture). Such injuries could be a crown fracture, concussion, subluxation, lateral luxation, extrusion, or avulsion of the coronal fragment (Figure 1). The most common concurrent injuries are likely to be concussion or subluxation, but, unfortunately, studies reporting the incidence of the various dental injuries (see earlier) have not reported how often these concurrent injuries occur to teeth with root fractures.
Root fractures involve many different tissues in both the teeth and the supporting structures. Hence, there will be complex healing patterns involving the many different tissues, namely, the dentin, cementum, dental pulp, periodontal ligament (PDL), and bone. When a root fracture occurs, the hard tissues of the tooth root (ie, the dentin and cementum) fracture, whereas the soft tissue of the tooth (ie, the dental pulp) may have a variety of injuries depending on whether the coronal fragment of the root has been displaced or not.
If there has been no displacement of the coronal fragment of the root, then the pulp in that fragment may not be damaged to any extent apart from a localized acute inflammatory response at the fracture site or it may have hemorrhage and bruising. However, if there has been displacement of the coronal fragment of the root, then the pulp may be stretched, or it may be completely severed (lacerated) at the fracture site1, 10; this leads to the coronal fragment of the tooth having a reduced or severed blood supply, which, in turn, could lead to pulp necrosis. In some cases, the pulp’s blood supply to the coronal fragment may recover, and then the pulp in the coronal fragment may heal. In other cases in which there has been pulp necrosis, subsequent infection of the root canal system may occur if there is a pathway for bacteria to enter the tooth. This is certainly possible because the traumatic incident may also have caused cracks, fractures, or displacement of the tooth.
The apical fragment of the tooth root is usually not affected by the injury because all the forces of the impact have been absorbed at the fracture site.10 The pulp's neurovascular bundle at the apical foramen will not be stretched, severed, or harmed because the apical fragment is not displaced, so the pulp in this fragment usually remains clinically normal.11-20 Likewise, the PDL around the apical fragment will not be damaged.10
The PDL at the fracture line and surrounding the coronal fragment will be damaged when there is a root fracture, and the extent of the damage will vary at different levels of the root; in the region of the fracture, there will be at least some acute inflammation, but the damage may be more extensive if there has been concurrent concussion, subluxation, luxation, or avulsion of the coronal fragment.
It is also likely that the alveolar bone may be damaged. The injury could be localized to the bone adjacent to the root fracture, or it may be more extensive, again depending on the presence of concurrent concussion, subluxation, luxation, or avulsion of the coronal fragment. The alveolar socket wall may also be fractured, and this is most likely to be the labial wall because it is usually very thin. Hence, a complex series of injuries may be associated with the root fracture.
2 CLASSIFICATION OF ROOT FRACTURES
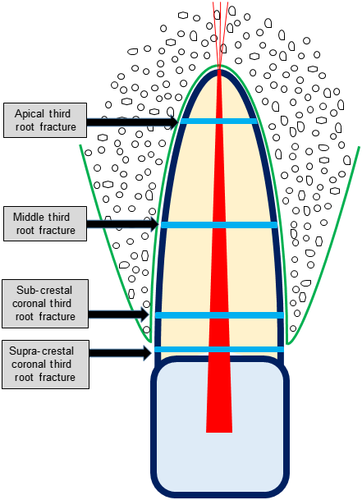
Traditionally, root fractures have been classified according to the location of the root fracture and specifically whether the fracture is located in the apical, middle, or coronal third of the tooth root.1 This classification is useful because the management and prognosis for a root fracture vary according to its location. The more apical fractures generally require the least management and have the best prognosis, whereas coronal root fractures require the most complex management and may have the worst prognosis. This classification also allows the analysis of cases for research purposes, which can then translate to a better understanding of the injuries and more appropriate management strategies.
Notwithstanding the usefulness and long-term use of the previously described classification system, it does have 1 shortcoming, which is related to fractures within the coronal third of the root. The management and prognosis of fractures in this part of the root are dependent on the very specific location of the fracture with respect to the crestal bone level. Root fractures that are located subcrestally (ie, within the bony socket) have a much better prognosis than those located supracrestally (ie, outside the bone socket). This is a result of several factors, such as the lack of root length of the coronal fragment, the lack of bone, and the lack of PDL to retain the coronal fragment if the fracture is located supracrestally so there is no possibility of PDL repair and stabilization of the coronal fragment. This was highlighted many years ago by Andreasen.21 Another major factor is the possible presence of bacterial infection because supracrestal root fractures typically communicate with the gingival sulcus and thus the mouth in general. This implies that infection of the fracture site is likely, and this can result in infection of the pulp in both the coronal and apical root fragments. Hence, a more aggressive approach to managing supracrestal root fractures is usually required (see later).
- The apical third of the tooth root.
- The middle third of the tooth root.
- The coronal third of the tooth root.
- Subcrestal.
- Supracrestal.
2.1 Responses to Root Fractures
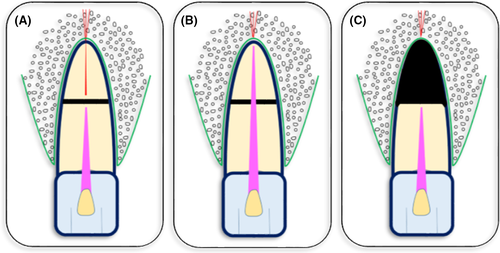
- Healing with hard dental tissue.
- Healing with connective tissue.
- Healing with bone and connective tissue.
- No healing where granulation tissue (inflammatory tissue) forms in the fracture line as a result of pulp necrosis and infection of the pulp space in the coronal fragment.
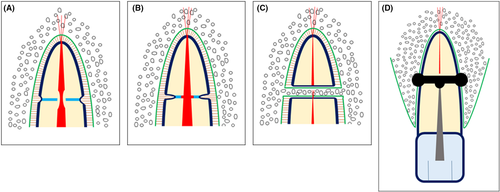
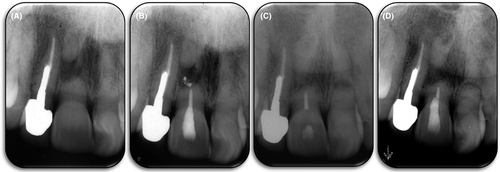
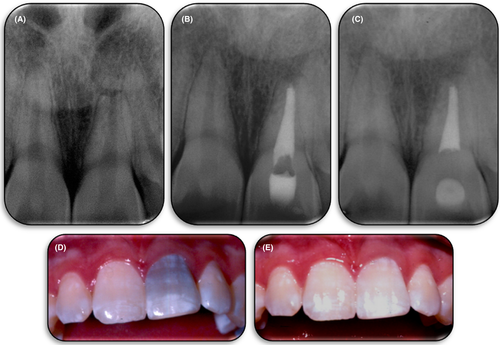
- Late pulp necrosis and infection of the coronal fragment (Figure 4A-D): initial healing with hard tissue, connective tissue, or bone and connective tissue in which the pulp in the coronal fragment survives the injury, but it later undergoes necrosis and becomes infected, leading to granulation tissue in the fracture line. This may occur many years after the injury.
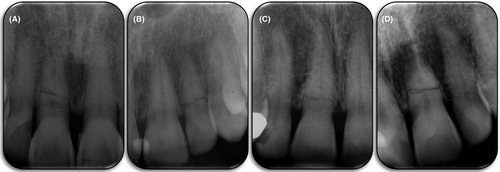
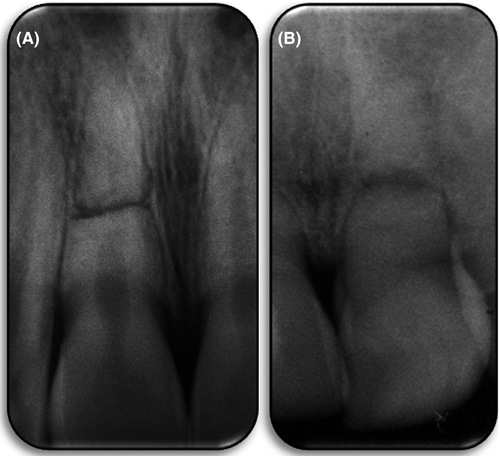
- Healing with dental hard tissue is the most ideal response (ie, healing occurs with dentin and cementum; Figures 3A and 5A-D). This is most likely to occur when there has been no displacement of the coronal fragment or only very minimal displacement with good repositioning after the accident. It may also occur in cases with significant displacement of the coronal fragment if there has been immediate or no significant delay in repositioning and stabilizing the coronal fragment. If there has been no displacement, the pulp tissue is unlikely to have been damaged. When there has been minimal displacement, the pulp may be stretched slightly but will maintain its blood supply. If there has been more substantial displacement, the blood supply to the coronal fragment will be severed, but revascularization may occur once the coronal fragment has been repositioned. Contamination of the wound with microorganisms is unlikely in these cases (unless there has been a concurrent crown fracture), and, therefore, the odontoblasts in the pulp have favorable conditions in which to produce reparative dentin to reunite the apical and coronal fragments. It is a similar process to the formation of a dentin bridge, except the dentin typically forms along the canal walls at the fracture line rather than across the pulp space (ie, it forms in a vertical manner rather than horizontally). It is also similar to a bone callus, and it can stabilize the fracture. At the same time, the PDL will attempt to repair itself at the periphery of the fracture, with the most likely response being some remodeling with minor resorption at the edges of the fracture to create rounded corners plus new cementum, which may help to unite the 2 fragments. The pulp in the apical fragment of the root remains normal because the blood supply at the apical foramen has not been affected. Pulp canal calcification (also called obliteration) also usually occurs over time in both fragments. In a large study of 400 teeth with root fractures, healing with hard tissue occurred in 30% of the teeth.17 This healing response can be diagnosed within 6 weeks of the injury.14
- Healing with connective tissue (Figures 3B and 6A, B) is the more likely response to a root fracture with displacement of the coronal fragment. The displacement may be extrusion, lateral luxation, or avulsion. In extrusion and lateral luxation cases, the pulp will be quite stretched or severed completely depending on the amount of displacement. When the coronal fragment has been avulsed, the pulp will be completely severed. Once the coronal fragment has been repositioned and stabilized (see later), the pulp may undergo repair by revascularization as long as there are no bacteria present at the fracture line or within the coronal fragment. Some of the pulp may grow into the space of the fracture, but the PDL cells are usually the dominant contributor to the healing reaction such that connective tissue derived from the PDL grows into the fracture line. In these cases, there is no union of the fractured segments, but the coronal fragment can still be quite stable. Remodeling via resorption at the edges of the fracture is common, and this creates rounded corners. In some cases, there may be some cementum formation, which may unite the 2 fragments to some extent. The pulp in the apical fragment of the root remains normal because the blood supply at the apical foramen has not been affected. Pulp canal calcification also usually occurs over time in both fragments. In a large study of 400 teeth with root fractures, healing with connective tissue occurred in 43% of the teeth.17 This type of healing response can usually be diagnosed within 6 weeks of the injury.14
- Healing with bone and connective tissue (Figures 3C and 7) typically occurs if the root fracture has occurred before the completion of growth of the alveolar bone; hence, this response is only observed when root fractures occur in young patients. Essentially, the coronal fragment erupts normally as the usual alveolar downgrowth process occurs, but the apical fragment remains in the position it occupied at the time of the injury. For this to occur, there must be no union of the fragments and no bacteria present in the pulp. A PDL space is often visible radiographically around the 2 fragments, including across the fracture line. Pulp canal calcification and rounding of the corners of the fragments at the edges of the fracture line are common. It is likely that the blood vessels of the pulp in the coronal fragment anastomose with blood vessels in the tissue that grow into the space between the root fragments and hence establish a new blood supply. The pulp in the apical fragment of the root remains normal because the blood supply at the apical foramen has not been affected. Pulp canal calcification also usually occurs over time in both fragments. In a large study of 400 teeth with root fractures, healing with bone and connective tissue occurred in 5% of the teeth.17
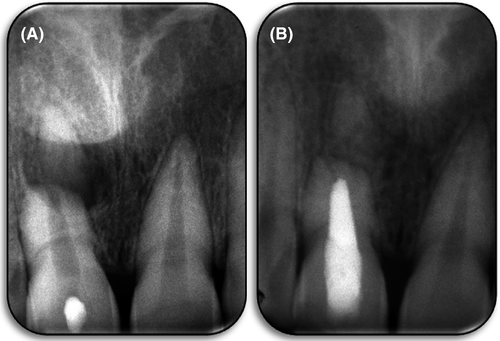
- No healing (Figures 3D, 8A, B, and 9A and E) of the fracture occurs if the pulp of the coronal fragment becomes necrotic and infected. When this happens, granulation tissue forms between the 2 fragments (ie, in the diastasis or space at the fracture line). The granulation tissue typically also extends into the bone adjacent to the fracture line giving the appearance of a radiolucency extending laterally. This inflammatory reaction is the same process that occurs within the periapical tissues whenever the root canal system becomes infected in teeth without root fractures, except that it is occurring at the fracture site rather than in the periapical tissues. The coronal fragment effectively has a new “apical foramen,” which is now located at the fracture line rather than at the apical end of the root, which is why the reaction occurs at this site. Some external inflammatory (infection-related) resorption of the coronal fragment may occur, especially around the canal opening, resulting in a wide or open “foramen” at the fracture line. External inflammatory resorption and/or remodeling of the cementum may also occur at the periphery of the fracture line to create round corners. The 2 fragments will not be joined if the coronal pulp becomes necrotic and infected soon after the injury.

Infection of the root canal system in the coronal fragment can occur by several means. It is typically caused by bacterial contamination at the time of the injury or immediately afterward. If the fracture is located supracrestally, then dental plaque in the gingival sulcus may be the source of bacteria because the fracture line is usually located at the base of the gingival sulcus. This may also occur in some subcrestal root fractures.
Infection of the root canal system of the coronal fragment may also be a result of cracks and/or fractures of the crown of the tooth because both cracks and fractures can be pathways for bacteria to enter the tooth. This may occur for root fractures at all levels of the tooth root.
Pulp necrosis and infection of the root canal system can occur soon after the injury (Figures 8 and 9) or many years later (Figure 4); see later for more details. If it occurs soon after the injury, it can often be diagnosed after about 3 weeks14 although it is typically noted after 3 to 4 months.13 This indicates that the pulp in the coronal fragment did not survive the injury, and bacterial contamination probably occurred at the time of the injury or at least very soon afterward.
In these scenarios, the pulp within the apical fragment is usually unaffected by the infection process in the coronal fragment although pulp canal calcification may occur.10-20 Dentin may be laid down over the coronal opening of the apical fragment as a protective mechanism.
- Late pulp necrosis and infection (Figure 4) can occur many years after the injury occurs. When a pulp necroses and becomes infected many years later, this indicates that the pulp initially survived the injury and continued to function (usually with pulp canal calcification also occurring) until some other event occurred to allow bacteria to enter the tooth system. The typical “other event” is likely to be a restoration breaking down (eg, if there had been a crown fracture restored with composite resin), an infraction extending to dentin, periodontal disease, and so on. Hence, the infection is not a direct result of the trauma and root fracture; rather, it is a secondary or indirect result of the overall situation after trauma to the tooth.
No studies have reported the specific incidence of late pulp necrosis and infection after root fractures.
3 PROGNOSIS
The frequency of pulp necrosis and infection of the root canal system after root fractures is relatively low. The pulp is more likely to survive a root fracture than a luxation injury.1, 22 Andreasen et al1 listed 15 studies that reported the frequency to be as low as 4% and ranging up to 55% in 1 study. Ten of these studies reported pulp necrosis in 18%-26% of the teeth, with only 4 studies reporting more than 26%. The 15 studies had a combined total of 1017 teeth, with only 274 (26.9%) teeth developing pulp necrosis (ie, only about 1 in 4 teeth with root fractures). Hence, the prognosis for the pulp in root fractured teeth is good and emphasizes the recommendation to not remove the pulp as part of the emergency management. Instead, a “wait and see” approach should be taken in order to monitor the tooth to see if signs of pulp necrosis and infection develop. These teeth can always have root canal treatment done at a later time when a definitive diagnosis of pulp necrosis and infection has been made. There is no advantage, and no evidence or sense, in commencing root canal treatment early or as a “preventive measure.” Such an approach is contraindicated because it removes the most important tissue (the dental pulp), which can provide the best healing outcomes (ie, internal repair with hard tissue).
Pulp survival is dependent on the age of the patient at the time of the fracture with younger teeth having a better prognosis. This is likely because of the better vascularity and wider root canals assisting pulp revascularization at the fracture site.
Pulp canal calcification is quite common after root fractures with reports ranging from 69% to 73%.14, 23, 24 The process typically occurs soon after the injury. It is usually well advanced by 9-12 months and approaches full density after 2 years.24 This calcification should not be considered as a poor outcome or an indication of a poor prognosis because calcification is a positive sign that the pulp has survived. Only a viable pulp is capable of producing dentin, so pulp canal calcification should be considered as a normal physiological response. It may complicate root canal treatment if this becomes necessary in the future, but this is not a reason to remove the pulp when calcification is noted because the pulp may never undergo necrosis or it may survive for many years. Root canal treatment of calcified canals can be performed by skilled operators with modern techniques and the assistance of magnification and illumination.
Teeth that have had root fractures commonly have some root resorption. However, this is not usually of any clinical consequence because it is typically a transient surface resorptive process; when external surface resorption occurs, it results in rounded corners or edges of the root at the ends of the fracture line. When internal surface resorption occurs, it results in rounding of the fracture edges at the junction between the root canal and the fracture line; this can occur in both the apical and coronal fragments. Hence, although the overall reported incidence of all types of resorption is quite high (about 60%), this figure is misleading because much of the resorption is transient and just a part of the remodeling process.1
Some teeth with root fractures may develop external inflammatory resorption, external replacement resorption, or internal inflammatory resorption.1 However, these types of resorption are usually a result of concurrent injuries such as luxation or avulsion of the coronal fragment with subsequent damage to the cementum and PDL, rather than being caused by the fracture itself. In the case of inflammatory resorption, infection of the root canal system leads to the resorptive process (ie, it is not the root fracture per se that causes the resorption).
The main preinjury factors affecting the healing of root fractures are the stage of root development (especially the diameter of the pulp lumen at the fracture site) and the patient's age.16, 17 The younger the patient and the wider the root canal, then the more favorable the tooth is for healing with hard tissue.
Factors associated with the injury that affect the prognosis are the stage of root development, type of concurrent injury if present, degree of displacement (if present) of the coronal fragment, the diastasis between the fragments after the fracture, mobility of the coronal fragment, and the response to pulp sensibility tests.16, 17 The location of the fracture is not a factor affecting healing outcomes, except when the fracture is located supracrestally in the coronal third; such fractures have the worst prognosis of all root fractures because of the lack of PDL and bone to support the coronal fragment, as discussed previously.1, 21 Teeth with coronal third fractures also have a higher risk of being lost if there is subsequent trauma to the tooth, even if only a minor injury19 or if the patient develops periodontal disease. An analysis of root fractured teeth from the Dental Trauma Guide website25 is summarized in Table 1, and this shows that 31% of the teeth with coronal third fractures were lost over 10 years, whereas only 8.7% of teeth with midthird root fractures were lost over the same period of time.
| No. of teeth | No. of years of follow-up | Apical third root fracture | Middle third root fracture | Coronal third root fracture |
|---|---|---|---|---|
| 13 | 46 | 16 | ||
| Tooth loss | 1 | 0 | 2 | 1 |
| 3 | 1 | 3 | 1 | |
| 10 | 1 | 4 | 5 | |
| Pulp necrosis and infection of the root canal system | 1 | 2 | 12 | 5 |
| 3 | 3 | 14 | 5 | |
| 10 | 3 | 14 | 5 | |
| Pulp canal calcification | 1 | 2 | 16 | 2 |
| 3 | 5 | 24 | 4 | |
| 10 | 9 | 25 | 9 |
Note
- The numbers are cumulative over the follow-up periods of 1, 3, and 10 y.
The presence of restorations in a tooth at the time of injury has been reported to be predictive of the healing response, as has the presence of periodontal disease at the time of injury.14 Teeth in these situations are more likely to heal with connective tissue rather than by hard tissue union, presumably because the pulp may have been compromised by previous trauma, dental caries, restoration, and/or periodontal disease. Teeth with restorations also have the potential for no healing of the fracture because bacterial penetration through the restoration:tooth interface may occur if the restoration is not ideal; this, in turn, can lead to pulp necrosis and infection of the root canal system followed by the formation of granulation tissue in the fracture line.
Treatment can also affect the prognosis of root fractured teeth, with the most favorable healing reported to be associated with optimal repositioning and splinting that does not require forceful application. Delays in seeking treatment did not affect the overall healing outcomes18 although this is likely to be affected by the injury factors mentioned previously (eg, teeth with displacement of the coronal fragment are likely to be more affected by treatment delay). Antibiotics did not help healing and even had a slight negative effect, as reported in 2 studies.14, 18 Hence, antibiotics are not indicated for a root fracture, and they should not be prescribed unless the patient has another injury that specifically requires them (eg, a fully developed avulsed tooth in which antibiotics are indicated to help prevent external inflammatory resorption).26
The 10-year survival rate for all root fractures is approximately 87%25 (Table 1). More studies are needed to investigate this further, but many clinicians who are very experienced in managing dental trauma cases anecdotally report that root fractured teeth can last for many, many years provided there is no further trauma to the tooth and provided the patient does not develop periodontal disease. The level of the root fracture is likely to be an important factor, with the more coronally located fractures, especially those with supracrestal root fractures, being more susceptible to these problems.
- Incompletely developed teeth: only 13 teeth from 11 patients have been analyzed. Because of the limited number of cases, they were not divided into apical, middle, and coronal third root fractures. The low number of cases is highly suggestive of this type of injury being extremely rare in young children whose teeth have not fully developed. The data also suggest that the prognosis for these teeth is extremely good because none of the 13 teeth were lost over the 10-year follow-up period, none of them had external resorption or ankylosis, none had bone loss, and there were no cases of pulp necrosis and infection of the root canal system. After 1 year, 4 teeth (31%) had pulp canal calcification. At the 3-year follow-up, 2 further teeth showed pulp canal calcification (cumulative total = 46%). After 10 years, 3 more teeth had pulp canal calcification for a cumulative total of 9 teeth (69%). As mentioned earlier, this calcification is a normal physiological response, and it indicates that the pulps in these teeth survived and continued to function.
- Fully developed teeth: a total of 75 teeth have been analyzed over 10 years. Most of these teeth had middle third root fractures (46, 62%) with 16 (21%) in the coronal third and 13 (17%) in the apical third of the roots. Unfortunately, the coronal third fractures were not divided into subcrestal and supracrestal fractures, so these 2 subgroups were considered together.
- Bone loss was evident for 19% of the coronal third fractures, 6% of the middle third fractures, and none of the apical third fractures.
- Ankylosis and replacement resorption were evident in 2.5% of the middle third fractured teeth but none for the coronal and apical third fractures.
- There were no cases with external inflammatory resorption.
Table 1 summarizes the other findings for the 75 fully developed teeth over the 10-year follow-up period. These data show the very good prognosis for teeth with root fractures because only 10 teeth (13%) were lost over this period of time with half of them being coronal third fractures. Pulp canal calcification is likely to occur if the pulp does not necrose; in the middle third group, only 7 (17%) of the 42 surviving teeth did not have calcification or pulp necrosis after 10 years, whereas 25 teeth (60%) had calcification and 14 teeth (33%) had necrosed and become infected. For apical third root fractures, 9 (75%) of the 12 surviving teeth had pulp canal calcification, and 3 (25%) had pulp necrosis and infection of the root canal system. Eleven teeth with coronal third root fractures survived; 82% of these had pulp canal calcification, and 5 (18%) had pulp necrosis and infection of the root canal system.
4 EXAMINATION AND DIAGNOSIS OF ROOT FRACTURES
- Increased mobility and/or displacement of the coronal fragment (but this may also resemble displacement of the entire tooth without a root fracture).
- Tenderness to percussion may indicate injury to the PDL, such as concussion or subluxation of the coronal fragment.
- Transient coronal discoloration may occur, either red or grey.
- Bleeding from the gingival sulcus may indicate subluxation of the coronal fragment.
Pulp sensibility testing is essential to perform at the initial posttrauma appointment because the results of these tests can be useful for predicting the long-term prognosis of the pulp. Initially, teeth with root fractures and no or only minor displacement will usually respond to pulp tests. However, if there has been displacement of the coronal fragment, then it is likely that the tooth will not respond to cold and electric pulp tests. It is important to understand that this lack of response should not be interpreted as the tooth having pulp necrosis, and they should not be used to indicate root canal treatment at this early stage. The response to pulp sensibility tests at the immediate posttrauma appointment should be noted for 3 reasons. First, a lack of response indicates that the tooth has suffered an injury and the pulp’s nerve supply has been affected, at least temporarily. Second, a lack of response is important for assessing healing complications because teeth that do respond have a significantly reduced risk of the pulp necrosing later. Thirdly, the results of these tests provide a baseline set of data to which future tests results can be compared, and this allows long-term monitoring and reassessment of the pulp status.
Root fractures will not be evident clinically, even if they are mobile, tender to percussion, and so on. It is usually not possible to clinically distinguish between tooth displacement because of a root fracture from displacement caused by a luxation injury. This highlights the essential need to take radiographs. The standard “trauma series” of periapical radiographs should be taken during the immediate posttrauma examination; this includes periapical, eccentric, and occlusal radiographs. Root fractures are often best seen on occlusal radiographs, especially if the fracture is in the apical or middle third of the root.1, 25 A bisecting angle periapical radiograph may be needed to visualize a coronal third root fracture.1, 25
When there has been no displacement of the coronal fragment, some root fractures may not be evident during the initial clinical and radiographic examinations. However, they may become evident at subsequent follow-up examinations because of the inevitable inflammatory response that will occur in the fracture line.23, 27, 28 This can lead to slight separation of the apical and coronal fragments, which may then be visible on radiographs. This highlights the need to review teeth with root fractures after 7-14 days with further radiographs.
Cone-beam computed tomographic (CBCT) imaging may help to show a root fracture, especially if there has not been any displacement of the coronal fragment.29 However, such imaging techniques will not always be readily available, and they are unlikely to change the management of the case because nondisplaced coronal fragments do not normally require any specific immediate management apart from occlusal relief (see later). Hence, CBCT imaging is not essential. However, the recent use of CBCT imaging has highlighted that the labial cortical plate of the alveolar socket may also fracture in conjunction with a root fracture. This is not surprising, given the nature of the injury and the thin bone wall that is typically present. Such bone fractures are most likely to occur when the coronal fragment has been displaced.
5 EMERGENCY MANAGEMENT
When a tooth has been diagnosed as having a root fracture, the emergency management will depend on several factors. The most important factors will be displacement of the coronal fragment and the level of the root fracture. If the coronal fragment has been avulsed, then it should be managed in the same manner as for an avulsed tooth.1 However, the apical fragment does not require any specific treatment in this scenario. Coronal fragments that have been laterally luxated or extruded should be repositioned back into their sockets.1
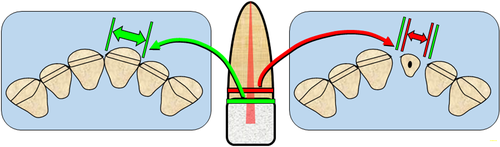
The level of root fracture is important because it dictates the emergency and subsequent treatment. Root fractures in the apical and middle thirds plus those that are subcrestal in the coronal third of the root should be managed in a conservative manner. The management of 3 types of root fracture is the same, whereas fractures that are located supracrestally in the coronal third must be managed differently (see later). Thus, the value of the proposed classification outlined previously becomes apparent.
- Repositioning and splinting: if the coronal fragment is not displaced and not mobile, then splinting is not required although it will not harm the tooth if a splint is placed. However, when the coronal fragment has been displaced or is mobile (ie, subluxated), then stabilization with a splint is indicated. A simple splint will suffice as long as it holds the fragment in its correct position. Simple splints can be made by using a stainless steel wire that is bonded with composite resin to the labial surface of the affected tooth and anchored in the same manner to 1 or 2 teeth on either side of the affected tooth. Ideally, the splint should not allow any movement of the coronal fragment. If the labial wall of the bone socket has also fractured, then this type of splint will also stabilize the bone fragments. Rigid stabilization is important because it provides the most ideal conditions for healing with hard tissue; if movement of the fragments occurs, then it is less likely that this type of healing response will occur. The length of time to splint the tooth has been questioned in recent years. Traditionally, 2-3 months was recommended for root fractures at all levels of the root.21 However, studies that have analyzed the effects of the splinting time have reported that shorter splinting periods did not affect the outcome for root fractures.16, 19 Hence, 4 weeks is now generally recommended for fractures in the apical and middle thirds but up to 4 months for fractures in the coronal third, especially when close to the cervical margin of the tooth.30 However, despite these recommendations, no harm from longer splinting times has been shown, so in order to create better conditions for healing by hard tissue, it is suggested that clinicians consider leaving splints in place for 3 months in all cases and possibly for 4 months for a fracture that is very close to the cervical part of the root (but still subcrestal).1
- Root canal treatment should not be commenced at the emergency appointment for these root fractures. As outlined previously, the prognosis for pulp recovery is quite good, and, therefore, the pulp should be provided with the opportunity to heal and continue to function. Maintaining the pulp in the tooth also allows for the possibility of hard tissue repair with dentin along the canal walls at the fracture site, which is the most favorable healing response.
- Antibiotics are not indicated for teeth with root fractures because it is unlikely that the wounds will be infected, except if the coronal fragment has been avulsed. Studies have shown that the use of antibiotics may even have a slight negative effect on pulp healing.14, 18 Therefore, they should be avoided unless there is another injury present that requires the use of antibiotics to prevent infection or external inflammatory resorption.
- Reviews of the healing response are essential and should be performed at intervals of 4 weeks while the splint is in place and then at 3-month intervals for the first 12 months. If no adverse findings become evident in that time, then annual reviews for 5 years should be arranged. Ideally, the tooth should be continually reassessed every 3-5 years thereafter.
- Attempt to retain the coronal fragment, but this is unlikely to be successful for the reasons outlined previously.
- Remove the coronal fragment immediately and assess whether the tooth can be adequately restored.
- If the remaining root is not suitable for restoration, then it should be extracted, and the site can be managed prosthetically with an osseo-integrated implant, a bridge, or a removable partial denture depending on the individual patient’s circumstances (the specific site, the mouth in general, the systemic health, finances, and so on).
- If the remaining root is suitable for restoration, root canal treatment should be performed followed by one of the following options to restore the tooth: restoration with a post-retained core and crown, periodontal (crown lengthening) surgery followed by restoration with a post-retained core and crown, or orthodontic extrusion followed by periodontal (crown lengthening) surgery and then restoration with a post-retained core and crown.
Most cases will require 1 of the last 2 options because it is usually not possible to simply restore these teeth with a crown without supplementary procedures such as surgery and/or orthodontics. Particular factors to consider with periodontal surgery are the depth of the fracture and the likely esthetic result because the gingival margin may not match the adjacent teeth. Orthodontic extrusion of the remaining root was first proposed by Heithersay in 1973.31 When considering this procedure, the remaining root length, the length of post required, and the length of the clinical crown must all be considered in order to ensure there are adequate crown:post and crown:root ratios for restoration and stability of the tooth.32 The emergence profile is another important aspect because the cervical diameter of the root at the level of the fracture may be less than the diameter at the natural gingival margin (Figure 10). Hence, the restoration will have greater divergence from the gingival margin toward the incisal edge,32 thus possibly creating esthetic and cleansing issues for the patient. The latter may lead to inflammation, which will be difficult to resolve. The more tapered the root is, the greater the effect will be and the more unsuitable the root becomes for these procedures.
Once the tooth has been restored, recall examinations of the periapical healing response are essential and should be performed after 6 months and then after another 12-24 months. If no adverse findings become evident in that time, then ideally the tooth should be continually reassessed every 4-5 years thereafter in the same manner as any tooth that has had root canal treatment and a comprehensive restoration.
6 FOLLOW-UP MANAGEMENT
As outlined previously, all teeth that have had root fractures should be reviewed at regular intervals just as all traumatized teeth should be. The main tissues to assess over the long-term will be the pulp (unless root canal treatment has been done), the PDL, and the gingivae (especially if the fracture is near the gingival margin).
When assessing the pulp, cold and electric pulp sensibility tests are essential and should be performed at each review appointment. A periapical radiograph should also be taken to assess the pulp and periapical tissues plus the tissues in and adjacent to the fracture line. It is likely that pulp canal calcification will become evident in both the apical and coronal root fragments. As discussed earlier, this is a favorable response, and it does not indicate the need for any intervention. If any signs of a radiolucency or resorption become evident, then appropriate treatment should be commenced. This will usually mean root canal treatment (see later) unless the resorption is replacement resorption with ankylosis, in which case extraction will be indicated at some stage.
The PDL will usually heal as outlined earlier, but it needs monitoring to ensure it remains healthy. The periapical radiographs are used to assess the PDL in conjunction with percussion, palpation, and mobility tests. If there has been any displacement of the coronal fragment, then the possibility of external inflammatory and/or external replacement resorption and ankylosis must be considered. The nature and degree of the displacement are key factors, which will be evident from the history and the emergency management of the tooth. These types of resorption may occur early in the follow-up period, or they may occur many years later. Hence, regular radiographic reviews are essential.
Periodontal probing is also essential, especially in cases with coronal third root fractures. The patient must maintain excellent oral hygiene to prevent plaque formation on the tooth because this could lead to premature loss of the tooth (because of the effective short root) or infection of the root canal system via the fracture if sufficient gingival recession occurs to provide a pathway for bacteria to reach the fracture.
7 ROOT CANAL TREATMENT, IF REQUIRED
Root canal treatment is only required in about one quarter of cases, as discussed earlier, because most pulps survive and function normally after root fractures. The typical response is pulp canal calcification, but this is not an indication for root canal treatment.
The need for root canal treatment arises within the first 3-4 months after the injury (Figures 8 and 9) or many years later (Figure 4). In both situations, only the coronal fragment needs the root canal treatment because the pulp in the apical fragment is usually unaffected and does not become necrotic. Hence, root canal filling and filling procedures should only be performed to the fracture line.
- The use of several long-term calcium dressings to encourage the formation of a hard tissue barrier across the opening before completing the root canal filling with a conventional technique, such as lateral compaction of gutta-percha and cement (Figures 8 and 9).
- Placement of an artificial barrier (eg, a hard-setting bioceramic material) at the opening before filling the remaining root canal with a conventional technique.
Both of these techniques appear to be associated with favorable outcomes. The latter technique is technically more difficult to perform and has the risk of extrusion of the artificial barrier material into the tissues between the 2 root fragments, which may lead to ongoing inflammation, a foreign body reaction, or delayed healing. Hence, this technique should only be attempted by experienced specialist practitioners in order to avoid such complications. The former technique creates a natural hard tissue barrier, which helps to confine the root filling materials to within the tooth root. This is important because healing has been shown to be more predictable if the root filling material had not extruded into the fracture line.20 It can be performed by most practitioners without the need for specialist training or extensive experience. One or 2 extra appointments may be required, and the overall treatment time will be longer, but these should be weighed against the very predictable outcomes and the simplicity of this technique. One advantage of this technique is that the long-term use of calcium hydroxide helps to ensure maximum antibacterial action has been obtained because this has been shown to improve treatment outcomes.33 If an artificial barrier technique is used, then calcium hydroxide should still be used as an intracanal medicament for a period of time before root filling to ensure no viable bacteria remain in the canal.
When the pulp necroses and becomes infected many years after the trauma, there has most likely been some pulp canal calcification before the pulp necrosis (Figure 4). Hence, the root canal typically has a very small opening at the fracture line, so the long-term calcium hydroxide or the artificial barrier techniques are not required. Notwithstanding this, the pulp canal calcification may complicate the treatment because it may be difficult to locate the canal orifice and then to negotiate the canal to the fracture line. However, once the canal has been located and negotiated, routine root canal treatment can be completed, and the access cavity can be restored.
Very occasionally, teeth with root fractures may develop pulp problems in the apical fragment. This could be irreversible pulpitis or an infected root canal system. If either of these occur, then the options are to perform root canal treatment of both the coronal and apical fragments or to perform root canal treatment of the coronal fragment and surgically remove the apical fragment (Figure 11). Fortunately, the apical fragment rarely has such problems and therefore does not normally require any treatment.
Cvek et al10 reported one case where the pulp recovered after the root fracture and had internal hard tissue repair but then the tooth developed irreversible pulpitis 5 years later as a result of caries. The entire pulp was removed and root canal treatment was performed to the apical fragment. No complications were reported and the lack of extrusion of any material through the fracture line confirmed the earlier internal hard tissue repair.
However, in another case reported by Cvek et al,10 there was no internal repair with hard tissue and when the entire root canal was treated to the apical foramen, there was considerable extrusion of root filling materials out through the fracture line which resulted in inflammation and separation of the two fragments. The apical fragment and the excess material then had to be surgically removed. At the 4-year review appointment, radiographic signs of healing were evident.
Cvek et al20 reviewed a series of 98 teeth with middle third and apical third root fractures. They reported that no healing occurred when the root canals of both fragments were filled. They noted that the lack of healing was related to extrusion of the root filling materials and/or necrotic debris through the fracture line. This caused persistent radiolucencies in the adjacent tissues. In contrast, 76% of cases healed when only the coronal fragment was filled. If the apical fragment had been removed surgically, healing was evident in 68% of the cases. Hence, there is good evidence available to show that only the coronal fragment should be endodontically treated in the first instance and the apical fragment should be left alone unless there is a very specific reason for treating it.
Teeth that have had pulp necrosis may also have some discoloration of the crown. If so, internal bleaching can be performed after the root canal treatment has been completed and before restoration of the access cavity (Figure 9B and D).
All teeth with root fractures that have had root canal treatment should be followed up in the usual manner; first, ensure that healing of the tissues in and adjacent to the fracture line occurs. This is mainly assessed by radiographic observation of the radiolucency disappearing and normal bone and PDL forming (Figures 4, 8, and 9). Second, these teeth should be monitored over the long-term to ensure the tooth is stable and that no further infection of the root canal system occurs (Figures 4C, D and 9E). As with any tooth that has had root canal treatment, these teeth will have at least a restoration in the access cavity. They may also have other coronal restorations if the crown had fractured during the accident that caused the root fracture or if there has been any caries. Restorations have a finite life span, and they will break down over time; this can provide pathways for bacteria to enter the tooth and reinfect the root canal system along with causing inflammation in the tissues surrounding the apical end of the coronal fragment. Thus, regular reviews should be performed every 4-5 years after healing has been confirmed.
8 CONCLUSION
Teeth with horizontal, oblique, or transverse root fractures have a very good long-term prognosis if the fracture is located in the apical or middle third of the root or if the fracture is located subcrestally in the coronal third of the root. Immediate repositioning (if displaced) and stabilization of the coronal fragment are essential because this provides the best situation for healing. Various healing responses have been reported with the most ideal being internal hard tissue repair with dentin. Some cases may have pulp necrosis with infection of the root canal system in the coronal fragment. These can be managed with root canal treatment. Supracrestal root fractures are the most difficult to manage and usually require removal of the coronal fragment, root canal treatment of the remaining root, and then a restoration. However, orthodontic and/or periodontal treatment is also usually required to facilitate the restoration. Figures 4-9 illustrate a range of cases with excellent long-term survival with most of them not requiring any treatment, and those that did require root canal treatment demonstrate healing and stability over time.
ACKNOWLEDGMENTS
The authors deny any conflicts of interest related to this study.