Diagnosis, management and impact on patients' lives of cancer-related neuropathic pain (CRNP): A European survey
Funding Information: Financial support for the conduct of the research (carried out by Hall & Partners) and preparation of the article was provided by Grünenthal GmbH.
Abstract
Objective
This study assessed the impact of cancer-related neuropathic pain (CRNP) on patients and the importance of the patient–healthcare professional (HCP) relationship in diagnosis and management.
Methods
A quantitative online survey was conducted involving adult patients from 13 European countries who had been diagnosed with treatable cancer and experienced symptoms of peripheral neuropathy.
Results
Of 24,733 screened respondents, 549 eligible persons met the inclusion criteria and completed the questionnaire. Among individuals still experiencing pain, 75% rated it as ‘severe’ or ‘moderate’. In addition, 61% reported a negative impact on day-to-day activities, and 30% said they had stopped working as a result. A third of respondents had received no diagnosis of CRNP despite reporting painful symptoms to an HCP. HCPs spending enough time discussing pain and understanding the impact on patients' lives were each associated with an increased likelihood of a formal CRNP diagnosis. Compared with individuals currently in active cancer treatment, cancer survivors were less likely to have a diagnosis of CRNP or regular pain conversations with HCPs.
Conclusion
CRNP remains under-recognised despite its substantial impact on patients' lives. Clinical practice may be improved by strengthening patient–HCP relationships around pain discussions and increasing the focus on pain management among cancer survivors.
1 INTRODUCTION
Worldwide, it is estimated that there will be 27.5 million new cases of cancer each year by 2040 (Worldwide cancer statistics|Cancer Research UK, n.d.). A 2016 systematic review of prevalence of cancer-related pain in an adult population reported that 66% of patients with advanced, metastatic or terminal disease will experience pain and that 38% of all patients with cancer will experience pain of moderate to severe intensity (Van Den Beuken-Van Everdingen et al., 2016).
Cancer-related neuropathic pain (CRNP) is thought to affect 19–39% of patients of patients with cancer, when considering both pure neuropathic and mixed (e.g., neuropathic and nociceptive) pain (Bennett et al., 2012). Chemotherapy-induced peripheral neuropathy, a common treatment-related type of CRNP, has been reported to be prevalent in 68% of patients after the first month of chemotherapy, 60% at 3 months and 30% at 6 months or more (Seretny et al., 2014).
CRNP may result from direct damage to the central or peripheral nervous system caused by a primary tumour or metastases, or from cancer treatments such as chemotherapy (painful chemotherapy-induced peripheral neuropathy), surgery (post-surgical neuropathic pain) or radiotherapy (Bennett, Kaasa, et al., 2019; Edwards et al., 2019).
CRNP is clinically heterogeneous, typically comprising many widely varying positive and negative symptoms. Positive symptoms include spontaneous and evoked pain, often characterised as shooting, sharp, stabbing, tingling, pricking, electric shock-like or pins and needles; negative symptoms include hypoaesthesia and hypoalgesia (Edwards et al., 2019; Fallon et al., 2018).
There is no clear consensus on the optimal stepwise approach to the treatment of CRNP (Edwards et al., 2019). Recommended drug therapies include opioids as well as ‘adjuvant analgesics’ such as tricyclic antidepressants and anticonvulsants (Berger et al., 2006; Fallon et al., 2018; Swarm et al., 2019). However, CRNP is likely to be under-recognised and under-treated in clinical practice (Edwards et al., 2019; Fallon et al., 2018). Furthermore, the psychological impact and the effects on patients' personal, social and professional lives remain poorly defined.
Individuals with cancer or with a history of the disease should be routinely screened for pain. In addition, healthcare professionals (HCPs) should play a proactive role in empowering and encouraging patients with cancer to discuss their pain, and patients should be educated on their management options (Bennett, Eisenberg, et al., 2019; Fallon et al., 2018). However, patients are often reluctant to discuss pain and HCPs do not always routinely ask about it (Bennett, Eisenberg, et al., 2019; Sancak & Butler, 2019). Few individuals with CRNP are referred to a pain specialist (Sancak & Butler, 2019), and standards of pain assessment and patient education may be suboptimal among non-specialists (Kwon, 2014). Thus, the effectiveness of patient–HCP partnerships in relation to CRNP management and support remains unclear.
The present study, based on an online patient questionnaire, had the following prespecified objectives: to assess the personal impact of CRNP on patients, to examine how the patient–HCP relationship affects the overall experience and to identify solutions to improve the management of CRNP. Upon review of the final dataset, an additional post hoc objective was added: to evaluate whether there are differences in support levels throughout the patient cancer journey.
This findings from this study will contribute to the literature base of the patient experience of CRNP and provide insights to better understand this condition for all specialties involved in cancer care. It is hoped that this will enhance the patient–HCP relationship, improve diagnosis and management, and empower patients to play an active role in managing their condition.
2 METHODS
2.1 Study design and participants
A quantitative online survey was offered to adult patients diagnosed with cancer and experiencing symptoms of peripheral neuropathy. The survey was developed by Hall & Partners, an independent market research agency, on behalf of Grünenthal. Survey questions were prepared with input from patient representatives, clinical experts and nurses. Recruitment aimed to include at least 25 participants from smaller countries and at least 50 participants from larger countries.
Participants were required to meet the following inclusion criteria: age ≥18 years, a diagnosis of cancer (of any type) that was deemed treatable (i.e., not palliative) and sure of their current cancer treatment status. They were also required to state that they had experienced at least 3 out of 10 listed symptoms relating to neuropathic pain from the Douleur Neuropathique en 4 Questions (DN4) questionnaire (Bouhassira et al., 2005). This is one fewer symptom than is normally required for a CRNP diagnosis; a lower cut-off was used because patients were self-assessing rather than being prompted by an HCP. There was no requirement for respondents to have discussed their symptoms with an HCP or to have received a formal diagnosis of CRNP. The survey was available in multiple languages and was estimated to take around 15 min to complete. Data were collected between 10 February and 1 June 2021.
Most participants (n = 517) were recruited and sent an invitation to complete the online survey using consumer/patient online market research panels consisting of consumers/patients who were willing to take part in online surveys (Dynata and Toluna consumer panels worked on recruitment for all markets; Opinion Health, the patient panel, worked on all apart from France), but a small number (n = 32) were recruited via flyer and communication by partnering patient organisations (through social media and websites). Prior to initiation of the survey, participants were made aware of the study sponsor and gave their explicit informed consent to participate.
The survey was conducted in accordance with legal and ethical guidelines from the Market Research Society (MRS), the British Healthcare Business Intelligence Association (BHBIA), the Association of the British Pharmaceutical Industry (ABPI) Code of Practice and the European Pharmaceutical Market Research Association (EphMRA) Code of Conduct. As is common with other similar purely attitudinal surveys where there is no requirement for respondents to take medications, the approval of an ethical review board was not necessary.
2.2 Survey content
The survey was divided into six sections: screening questions to ensure respondents met all of the inclusion criteria, disease journey and knowledge regarding neuropathic pain and peripheral neuropathy, HCP contact, current CRNP treatment, living with CRNP, and demographics. All parts of the survey were mandatory, apart from the demographics section, which was completed on a voluntary basis. Questions were multiple choice with provision for free-text responses where appropriate.
2.3 Screenout data
Due to the strict eligibility criteria, many participants were screened out from inclusion in the final dataset. There was a high dropout rate at survey section S2 (confirmation of diagnosis of cancer) and S4b (presence of CRNP symptoms)—this is to be expected in a patient demographic with a large reach via panels. Higher dropouts were observed with the consumer panels (the patient panel was used later in recruitment). Following standardised data checks, 15 samples were replaced due to anomalous readings/data quality issues.
2.4 Statistical analysis
Data were analysed using Askia Analyse (version 5.3.5.5). Comparisons between subgroups were made using the z-test whereby the calculated P values of <0.05 were considered to be statistically significant.
Descriptive statistics are provided, including frequency and percentage for categorical variables. The denominator is N = 549 throughout unless stated otherwise.
3 RESULTS
3.1 Patient characteristics
From a total of 24,733 screened individuals, 549 respondents (2.2%) met the inclusion criteria and completed the questionnaire (Table 1). Responses were collected from participants across 13 countries in Europe: Austria (n = 29), Belgium (n = 30), Denmark (n = 43), France (n = 40), Germany (n = 50), Ireland (n = 24), Netherlands (n = 48), Norway (n = 28), Portugal (n = 26), Spain (n = 49), Sweden (n = 49), Switzerland (n = 30) and the United Kingdom (n = 103). Most were aged 36–55 years (n = 287; 52%). Among 529 respondents who consented to providing personal information, 329 (62%) identified as female and 199 (38%) as male.
| Characteristic (N = 549) | Patients, n (%) |
|---|---|
| Sexa | |
| Male | 199 (38) |
| Female | 329 (62) |
| Does not identify as either | 1 (<1) |
| Age, years | |
| ≤35 | 61 (11) |
| 36–55 | 287 (52) |
| 56–65 | 134 (24) |
| ≥66 | 67 (12) |
| Employment statusa | |
| Employed, studying or seeking employment | 221 (42) |
| Retired or unemployed | 276 (52) |
| Cancer treatment status | |
| Pre-cancer treatment (not yet receiving treatment) | 7 (1) |
| In active treatment (currently receiving treatment) | 240 (44) |
| Not in active treatmentb | 232 (42) |
| Cancer survivor (treatment finished and no longer in oncology care) | 70 (13) |
| Pain status | |
| Currently experiencing this pain all the time (chronic) | 176 (32) |
| Currently experiencing this pain intermittently | 301 (55) |
| Just started experiencing this pain | 21 (4) |
| No longer experiencing this pain (controlled by treatments taken) | 22 (4) |
| No longer experiencing this pain (went away on its own) | 29 (5) |
| Neuropathic pain interventions triedc | |
| Pharmaceutical treatments prescribed by a doctor | 245 (47) |
| Pharmaceutical treatments bought from a pharmacy | 131 (25) |
| Complementary and alternative therapies | 108 (21) |
| Heat packs or ice packs | 113 (22) |
| Contrast baths | 77 (15) |
| Self-distraction when pain occurs | 200 (38) |
| Avoidance (not using body area when pain is bad, etc.) | 57 (11) |
| Exercise | 185 (36) |
| Physiotherapy | 127 (24) |
| Relaxation | 177 (34) |
| Keeping a diary | 48 (9) |
| Cannabis | 41 (8) |
| Alcohol | 32 (6) |
| Comorbidity present | 243 (44) |
- a N = 529 (20 participants did not complete the demographics section).
- b Patients had completed cancer treatment (cancer gone or stable) but still in oncology care for monitoring/check-up or had completed cancer treatment and disease was progressive and might need future treatment.
- c N = 520 (respondents still experiencing pain).
The most common cancer types were breast cancer (n = 214; 39%), haematological malignancies (n = 67; 12%), lung cancer (n = 57; 10%) and gastrointestinal cancer (n = 55; 10%). The majority of respondents were either in active treatment for cancer (n = 240; 44%) or were not in active treatment but were still seeing their oncologist for monitoring or follow up (n = 232; 42%).
When asked to describe their neuropathic pain, most said that they were currently experiencing symptoms (n = 498; 91%); a minority had previously had neuropathic pain symptoms but were no longer experiencing them (n = 51; 9%). When asked to assess which of the 10 pain items of DN4 applied to them, 63 respondents (11%) selected three of these criteria, 261 (48%) chose four criteria and 225 (41%) selected five or more. The most common selections were: ‘My pain is associated with numbness’ (n = 384; 70%), ‘My pain is associated with tingling’ (n = 384; 70%), ‘My pain is associated with pins and needles’ (n = 328; 60%) and ‘I feel a pain which is like a burning sensation’ (n = 323; 59%).
3.2 Impact of CRNP on patients' lives
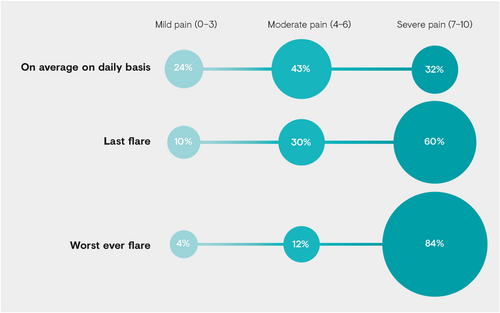
Respondents were asked to assess their CRNP on a scale of 0 (no pain at all) to 10 (worst pain imaginable). Among 520 individuals still experiencing pain, 167 (32%) said that it was ‘severe’ (rated 7–10) on an average daily basis and 226 (43%) felt that it was ‘moderate’ (rated 4–6) (Figure 1). Furthermore, 492 of 549 respondents (90%) said that, during their last CRNP flare, their pain was ‘severe’ or ‘moderate’.
When asked to describe how their life had changed as a result of CRNP (if at all), 337 (61%) reported a negative impact on their day-to-day activities, 263 (48%) reported decreased self-esteem and 84 (15%) said that their relationship with a partner had been negatively affected. Furthermore, 164 (30%) reported having to retire or stop working as a result of their CRNP.
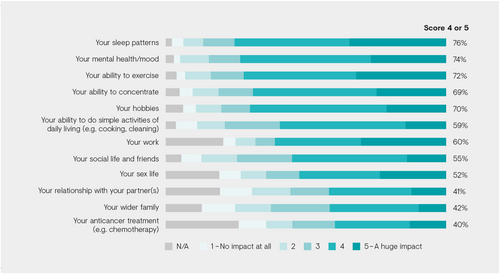
Respondents were also asked to assess the impact of CRNP on various aspects of their life using a scale of 1 (no impact at all) to 5 (huge impact). Ratings of 4 or 5 were considered to be indicative of ‘high’ impact (Figure 2). In total, 415 individuals (76%) said that CRNP had a high impact on sleep patterns, and most also stated that CRNP had a high impact on their mental health/mood (n = 404; 74%), ability to exercise (n = 397; 72%) and hobbies (n = 383; 70%). Furthermore, 218 (40%) noted a high impact of CRNP on their anticancer treatment.
Among 385 respondents who had not had to retire or stop working because of CRNP, 150 (39%) said that they had missed five or more days of work or education in the past 12 months due to their pain.
When asked about their expectations from treatment, around a third of respondents hoped that it would keep them pain-free (n = 201; 37%), and fewer than half expected that treatment would keep pain at a bearable level (n = 242; 44%).
3.3 Impact of patient–HCP relationship on patient experience
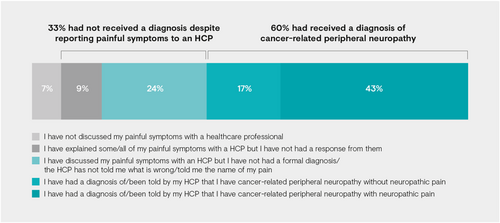
Although all 549 of the included respondents reported at least 3 of the 10 pain items of DN4 (and 89% reported at least 4), only 329 (60%) said that they had received a formal diagnosis of cancer-related peripheral neuropathy (Figure 3). Meanwhile, 183 individuals (33%) had received no diagnosis despite reporting painful symptoms to an HCP.
Responses to questions relating to the patients' relationship with their HCPs were compared between individuals with a formal diagnosis and those without. Being diagnosed with CRNP was strongly associated with HCPs from various specialties spending enough time discussing pain during appointments (Table 2). Furthermore, compared with those with no CRNP diagnosis, patients with a formal diagnosis were significantly more likely to feel that their HCP understands the impact of CRNP on their life (n = 82/131 [63%] vs. n = 231/271 [85%], respectively) and makes every effort to find the best treatment (n = 80/131 [61%] vs. n = 226/271 [83%]); additionally, they were significantly less likely to state that their HCP makes them feel like their CRNP is unimportant (n = 64/131 [49%] vs. n = 41/271 [15%]).
| No CRNP diagnosis | With CRNP diagnosis | P value | |
|---|---|---|---|
| Made appointment to see HCP to discuss CRNP when pain was particularly bada | 106/173 (61%) | 233/295 (79%) | P ≤ 0.0005 |
| Oncologist spends enough time discussing CRNP during appointmentb | 26/81 (32%) | 179/217 (82%) | P ≤ 0.0005 |
| Oncology nurse spends enough time discussing CRNP during appointmentb | 9/30 (30%) | 67/84 (80%) | P ≤ 0.0005 |
| GP spends enough time discussing CRNP during appointmentb | 28/77 (36%) | 93/125 (74%) | P ≤ 0.0005 |
| My HCP makes me feel like my CRNP symptoms aren't realc | 54/131 (41%) | 35/271 (13%) | P ≤ 0.0005 |
| My HCP understands how CRNP impacts my overall lifec | 82/131 (63%) | 231/271 (85%) | P ≤ 0.0005 |
| My HCP makes every effort to find the best treatment for mec | 80/131 (61%) | 226/271 (83%) | P ≤ 0.0005 |
| My HCP makes me feel like my CRNP is unimportantc | 64/131 (49%) | 41/271 (15%) | P ≤ 0.0005 |
- Note: Data are n/N (%); data in bold indicate the higher percentage.
- Abbreviations: CRNP, cancer-related neuropathic pain; GP, general practitioner; HCP, healthcare professional.
- a Based on responses to the question ‘In the past 12 months, how many times have you seen a doctor or other HCP for help/treatment for when your neuropathic pain has been particularly bad?’.
- b Based on responses to the question ‘Do you feel that the HCPs that you see spend enough time talking to you about managing your CRNP?’.
- c Based on responses to the question ‘Using the scale below where 5 is completely agree and 1 is not agree at all, please rate your agreement with the following statements about your relationship with the HCP who you discuss your neuropathic pain with as part of routine follow ups’.
When asked about pain management strategies, respondents with a CRNP diagnosis were more likely to have received prescription pharmaceutical treatment (n = 182/312 [58%] vs. n = 63/209 [30%]) or physiotherapy (n = 96/312 [31%] vs. n = 31/209 [15%]) compared with those without a diagnosis.
In addition, those with a diagnosis of CRNP were significantly more likely than those without a formal diagnosis to say that they were ‘highly satisfied’ or ‘satisfied’ with their current neuropathic pain treatments (n = 164/244 [67%] vs. n = 59/138 [43%], respectively).
3.4 Impact of cancer treatment status on CRNP care
When asked about their current cancer treatment status, most respondents said that they were in active treatment (n = 240; 44%), no longer in active treatment but still in oncology care (n = 232; 42%) or that their treatment was finished and they were no longer in oncology care (i.e., a ‘cancer survivor’; n = 70; 13%) (Table 1).
There were differences in characteristics between these three groups. Those in active treatment were typically more likely to be young and male, and to suffer from intermittent pain; those no longer in active treatment but still in oncology care were more likely to be middle-aged with multiple malignancies and were less likely to be in full-time employment; and cancer survivors were more likely to be older, female and have a comorbidity.
An analysis was performed of responses to various survey questions subdivided according to current cancer treatment status. Over the previous 12 months, cancer survivors were significantly more likely than the other two groups to have not discussed CRNP during routine HCP appointments (active treatment, n = 8/230 [3%]; no longer in active treatment but still in oncology care, n = 20/192 [10%]; cancer survivor, n = 14/39 [36%]) (Figure 4). They were also significantly more likely to have not seen an HCP for help/treatment when their pain was particularly bad (active treatment, n = 34/230 [15%]; no longer in active treatment but still in oncology care, n = 72/192 [38%]; cancer survivor, n = 22/39 [56%]).
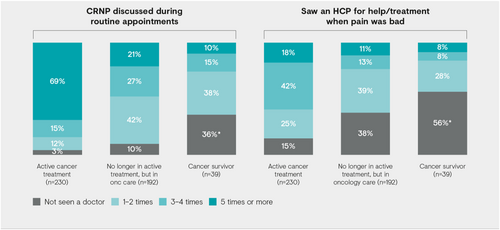
When asked whether they had discussed CRNP symptoms with their HCPs in the past 6 months, 31/70 cancer survivors (44%) had had no such conversations; by contrast, 14/240 patients (6%) in active cancer treatment and 45/232 individuals (19%) no longer in active treatment but still in oncology care had had no such conversations with an HCP in the past 6 months.
With regard to being diagnosed with cancer-related peripheral neuropathy, this was significantly more frequent among respondents still in active treatment (n = 165/240; 69%) compared with those no longer in active treatment but still in oncology care (n = 124/232; 53%) or cancer survivors (n = 37/70; 53%).
When asked about CRNP management strategies, patients in active cancer treatment were more likely than those no longer in active treatment but still in oncology care or cancer survivors to have been given prescription pharmaceuticals (n = 144/233 [62%] vs. n = 80/217 [37%] vs. n = 19/64 [30%], respectively) or physiotherapy (n = 80/233 [34%] vs. n = 39/217 [18%] vs. n = 8/64 [13%]).
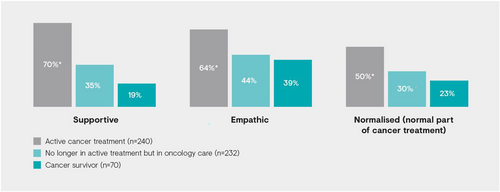
Finally, patients in active cancer treatment were also more likely than the other two groups to feel that their HCPs were supportive and empathic towards their CRNP and that they normalised this pain as part of cancer care (Figure 5).
4 DISCUSSION
This quantitative online survey was completed by 549 eligible individuals with cancer and neuropathic pain symptoms from across Europe. The most commonly described symptoms were numbness, tingling, pins and needles, and a burning sensation. These overlap with results from another recent patient survey, which found that tingling, electric shock, and pins and needles were the most frequently reported CRNP symptoms (Baek et al., 2021).
Eligible respondents were only required to show 3 of the 10 symptoms listed in DN4, which is one fewer than is typically needed for a CRNP diagnosis (Bouhassira et al., 2005; Shkodra et al., 2021), but a lower threshold was justified because patients were self-evaluating rather than being guided by an HCP. Most respondents (n = 486/549, 89%) showed more than three symptoms listed in DN4. The DN4 covers a variety of pain sensations but does not consider other types of pain (i.e., nociceptive, central sensitisation); the assumption was made that by selecting the minimum number of symptoms on the DN4, the participant's pain would be considered as neuropathic. As cancer survivors often experience mixed pain types (Leysen et al., 2019), it cannot be discounted that other pain types may have influenced the overall pain score.
The study demonstrated that CRNP has a significant impact on patients' lives. Around three-quarters of those currently experiencing pain rated it as ‘severe’ or ‘moderate’ on an average daily basis, and over half reported a negative effect on day-to-day activities. This aligns with previous data (Oh et al., 2017; Oosterling et al., 2016). For example, a large Korean study of more than 2000 patients with cancer found that neuropathic pain was associated with significantly increased pain severity, greater impact on daily living and worse quality of life compared with non-neuropathic pain (Oh et al., 2017).
Furthermore, the impact of CRNP on patients' professional lives is often profound, with 30% of respondents in the present study stating that they had retired or stopped working as a result; many of those who were still able to work described missing five or more days over the past year due to their pain. This aligns with data from a patient survey in France, which demonstrated that cancer survivors with neuropathic pain were less likely to be working than those without such pain—and were working fewer hours even if they were in employment (Alleaume et al., 2018).
Under-diagnosis and under-treatment are widely recognised issues in the management of CRNP (Edwards et al., 2019; Fallon et al., 2018; Oh et al., 2017). Indeed, a systematic review of cancer pain studies found that around one in three patients were not receiving medications in proportion with the intensity of their pain (Greco et al., 2014). The present work reinforces these concerns. One-third of respondents had received no formal diagnosis despite reporting painful symptoms to an HCP, and fewer than half had been prescribed pharmaceutical therapies. Moreover, patients' expectations from CRNP treatment were modest, with only 44% expecting that it would keep pain at a bearable level and fewer still aspiring to achieve complete freedom from pain.
Our data suggest that optimising the patient–HCP relationship may be crucial to minimising under-recognition and under-treatment of CRNP. Indeed, there appeared to be a strong association between HCPs spending enough time discussing pain during appointments and patients receiving a formal CRNP diagnosis. Feeling that HCPs understood the impact of cancer-related pain and recognised its importance was also linked with an increased likelihood of diagnosis. This then affected management of the condition, with formal diagnosis being associated with increased use of key treatment modalities, such as prescription drugs and physiotherapy, and greater patient satisfaction with pain treatment.
Another important insight from the current study is that the level of CRNP diagnosis and management varies greatly according to the stage of the patient's cancer journey. Individuals considered to be ‘cancer survivors’ (i.e., those whose treatment had finished and who were no longer in oncology care) reported a substantially different outlook compared with those currently in active cancer treatment. During the past year, cancer survivors were less likely to have discussed CRNP with their HCPs, less likely to have sought help when their pain was particularly bad, less likely to have received a formal diagnosis of CRNP and more likely to be under-treated for pain compared with individuals who were currently in active cancer care. Cancer survivors also described feeling less support and empathy from HCPs around their pain.
Thus, there may be a need for greater focus on neuropathic pain diagnosis and management in the cancer survivor group. Estimates suggest that up to 40% of these individuals experience chronic pain; (Bennett, Eisenberg, et al., 2019; Bennett, Kaasa, et al., 2019) ongoing pain monitoring is important not only for improved functioning and quality of life, but also as an indicator of potential cancer recurrence (Bennett, Kaasa, et al., 2019). A recent position statement from the European Pain Federation stressed the importance of routine screening for pain among individuals with a history of cancer during every engagement with an HCP – and the need for a multimodal pain management plan that integrates individual patient preferences and goals (Bennett, Eisenberg, et al., 2019). Given that cancer survivors typically have limited interactions with oncologists, the primary burden for meeting these requirements will fall on general practitioners and other specialists that may be involved in long-term care, such as neurologists or pain specialists. This emphasises the importance of appropriate referral. However, a recent HCP survey suggested that only a small proportion of patients are referred to a pain specialist (Sancak & Butler, 2019).
The present work has important strengths. In particular, it addresses key practice questions around CRNP that have not been widely assessed previously, such as the impact of the patient–HCP relationship on the overall experience, and possible gaps in pain support later in the cancer journey. Furthermore, the sample size was sufficiently large to give the data substantial weight. We must also acknowledge the limitations of the study, which are similar to other survey-based studies (Moro et al., 2020; Rakusa et al., 2021). First, the dropout rate might be considered high given that only 549 individuals were included in the analysis from almost 25,000 screened respondents. However, most of those who started the survey after completing the screening questions went on to finish it all, which suggests that the main cause of dropout was ineligibility. Second, the survey was conducted only in Europe, and hence caution is required when extrapolating the data to other parts of the world. Third, within Europe, there was a higher weighting of respondents from some countries (e.g., UK) compared with others. Nonetheless, patients came from a wide range of countries (13 overall), and some skewing is almost inevitable in survey-based research. Fourth, although the recruitment process was designed to minimise the risk of ‘self-selection’ bias, it remains possible that some individuals who enrolled were particularly keen to express their views around their condition and its treatment. Finally, the research was conducted during the COVID-19 pandemic, which may have affected patients' disease experience and their overall care.
Nonetheless, this study provides important data confirming that CRNP has a significant impact on patients' daily lives and that diagnosis is a key challenge. It is clear that many individuals affected by ongoing symptoms of CRNP remain unrecognised within the healthcare system. Furthermore, patients have low expectations of treatment despite the availability of multiple options that could reduce their pain. Clinical practice could be improved by: (i) building strong patient–HCP relationships that allow for frequent and thorough assessments of pain, and (ii) a greater focus on improving pain care for cancer survivors who are no longer receiving active cancer treatment. As this latter group is unlikely to be under regular oncology management, general practitioners and relevant pain specialists should play a central role. HCP learning could probably improve early management of CRNP.
ACKNOWLEDGEMENTS
The authors would like to thank NexGen Healthcare Communications for their medical writing and editorial support, supported financially by Grünenthal GmbH. The authors also thank the patients that have participated in this survey.
CONFLICT OF INTEREST
Denis Dupoiron has received consultancy fees from Grünenthal GmbH, Medtonic and Esteve. Gudula Petersen and Mariëlle Eerdekens are employees of Grünenthal GmbH. All other authors have no competing interests to declare. No author received a consultancy fee for this project.
Open Research
DATA AVAILABILITY STATEMENT
Research data are not shared due to privacy or ethical restrictions.