Implicit gender bias in the diagnosis and treatment of type 2 diabetes: A randomized online study
A. Skvortsova and S. H. Meeuwis have equally contributed to this manuscript.
Abstract
Aims
Implicit gender biases (IGBs) are unconscious evaluations about a person based on gender. IGBs of healthcare providers may affect medical decision making. This study investigated whether IGBs and genders of patients and general practitioners (GPs) influence diagnostics and treatment decisions in the context of diabetes type 2.
Methods
Ninety-nine GPs participated in this randomized online study. Implicit Associations Tasks were used to measure two IGBs, related to lifestyle (women have a healthier lifestyle than men) and communication (men are less communicative than women). Clinical decisions regarding type 2 diabetes were measured with vignettes that included a fictional male or female patient case.
Results
Female GPs exhibited a significant lifestyle IGB (p < 0.001). GPs of both genders exhibited a significant communication IGB (p < 0.001). Several associations between IGBs and clinical decisions were found. The gender of the vignette character affected several outcomes, for example GPs were less certain in the diabetes diagnosis when the character was a woman (p < 0.001).
Conclusion
We demonstrated that GPs have IGBs and these biases as well as patient's gender affect decisions of GP's when they are solving a diabetes vignette case. Future research is needed to understand the most important consequences of IGBs in the context of type 2 diabetes.
What's new?
Gender biases affect medical decision making and women tend to get less optimal healthcare than men. No one has described the effects of gender biases in the context of type 2 diabetes care. In this study, we found that Dutch general practitioners have an implicit gender bias regarding communication style of their patients and that female general practitioners also have a bias that men have an unhealthier lifestyle than women. These biases were associated with several aspects of clinical decision making in a fictional vignette case. Future research should investigate the consequences of gender biases and find ways to prevent them.
1 INTRODUCTION
The genders of patients and healthcare providers play a role in various steps of clinical decision making: from screening and diagnosis to treatment choices.1-3 Particularly, women tend to receive less optimal diagnostics and treatment interventions relative to men.4-8 The quality of healthcare also varies depending on doctor–patient gender interactions.3 Gender could be relevant for chronic disorders that require regular contact between healthcare providers and patients, in particular when the disorder's pathophysiology involves sex or gender differences, as for type 2 diabetes.
Multiple sex (biological characteristic) and gender (socially constructed characteristic) differences have been described in the pathophysiology of type 2 diabetes.9, 10 Women with type 2 diabetes have a significantly higher relative risk of cardiovascular complications compared to men.11, 12 Type 2 diabetes doubles the risk of cardiovascular mortality for men and triples it for women.13 One possible explanation for these increased risks might be that men are usually diagnosed with type 2 diabetes at an earlier stage than women.14 Moreover, women with type 2 diabetes have higher HbA1c and LDL cholesterol levels compared to men,15 which are important risk factors for cardiovascular and other complications. Finally, there are important sex and gender differences in psychosocial consequences of type 2 diabetes: women with diabetes have worse quality of life, worse mental well-being and more daily limitations compared to men with diabetes.16
These differences between men and women in type 2 diabetes outcomes may be partially explained by the disparities in received healthcare. One of the ways how sex and gender can affect treatment is through implicit gender biases of healthcare professionals. Implicit gender biases (IGBs) are unconscious evaluations about a person based on their gender17 that can manifest in various steps of the decision making process of a healthcare professional. Healthcare providers might consciously or unconsciously utilize the knowledge and attitudes regarding sex and gender when they treat their patients, which can influence the process of decision making. Literature shows that implicit biases affect clinical decisions of the healthcare professionals, but the majority of such research focused on racial biases.18 IGBs were shown to affect the diagnostic and treatment strategies in the context of coronary heart disease.19 Additionally, there are differences between men and women in their IGBs. Some studies find that men have more positive implicit biases towards men,20, 21 while women have either no bias20 or more positive biases towards women.21 These gender differences in IGBs might be the reason why patient–doctor gender interaction can affect the treatment outcomes. It was, for example, shown that women with type 2 diabetes who have a female general practitioner had the highest adjusted rates of HbA1c control, while women with male doctors had the lowest.22
To our knowledge, no research to date has investigated the role of IGBs in the context of type 2 diabetes. We focused on two potential IGBs that might be related to symptom communication and treatment of type 2 diabetes: (1) that women have healthier lifestyle habits than men (a lifestyle bias); (2) that women are more communicative and outspoken, while men are more reserved and stoic (a communication bias). We chose an implicit bias about lifestyle, as lifestyle majorly influences the development and progression of type 2 diabetes.23 Literature regarding gender differences in lifestyle of individuals with diabetes is inconsistent but some studies indicate that women with type 2 diabetes tend to have healthier nutrition habits than men.10 Symptom communication is another important factor that is involved in timely diagnosis and treatment of various diseases.24 Literature indicates that women tend to give more detailed histories and present more symptoms during medical visits than men.25 These gender differences might be consciously or unconsciously taken into the account by GPs and lead to development of implicit biases. In this vignette study, we investigated whether GPs have IGBs regarding lifestyle and communication styles of their patients, and whether these biases and patient's and GP's own genders affect clinical decisions of GPs in diagnosis and treatment of type 2 diabetes. We hypothesized that higher biases would be associated with less optimal vignettes' outcomes, such as giving the diagnosis at a later stage, less certainty in diagnosis and less certainty in the acceptance of the treatment. Additionally, we explored whether GPs' and patients' genders affect clinical decisions. We expected that GPs would have stronger negative biases against the other gender.
2 METHODS
2.1 Study design
A randomized between-subjects study design was applied. The study consisted of a vignette experiment which was embedded in an online survey. Randomization to the groups (male vs. female vignette character) was stratified according to participants' gender. The study was approved by the Psychology Research Ethics Committee of Leiden University (CEP19-1104/540).
2.2 Participants
GPs and GPs in training across the Netherlands were invited to participate in the study on the online survey platform Qualtrics. The study was advertised to be investigating the effects of patient characteristics and lifestyle on treatment decisions, without mentioning diabetes and gender (Appendix S1). Inclusion criteria consisted of being either a GP or GP in training, and having a good understanding of Dutch and English language.
The target sample size was 200 participants. Because no studies have looked at lifestyle and communication biases before or investigated the relation between implicit biases and type 2 diabetes treatment choices, it was not possible to use previous literature for statistical power analysis. Instead, we based our sample size on the average sample size of studies that investigated implicit biases in physicians by implicit associations.18
2.3 Measurements
2.3.1 Medical vignette
Participants rated a vignette that described a series of consultations with a hypothetical person (either male or female) and a GP. Vignettes are a set of systematically varied descriptions of people, objects or situations used to assess participants' beliefs, attitudes or intended behaviour towards them.26 In each vignette, the hypothetical patient's symptoms and complaints associated with type 2 diabetes were described (see Appendix S1). The vignettes were identical except for the gender of the described character. Participants rated aspects of the vignette based on the specific consultation phase presented in the following fixed order:
Initial consultation
Participants rated the likelihood that the complaints could indicate the following medical conditions: burn-out, vitamin B12 deficiency, anaemia, type 2 diabetes. Ratings were on a scale of 0 (‘very unlikely’) to 100 (‘very likely’).
Diagnosis
Participants rated the likelihood of type 2 diabetes diagnosis using the same 0–100 scale as described above. The likelihood rating was based on blood analyses in which a HbA1c of 48 mmol/mol was found. This value is considered ambiguous in the Netherlands, where type 2 diabetes diagnostics do not mention HbA1c but are based on glucose levels combined with the hyperglycaemia complaints.27 Secondarily, participants rated how confident they were about the diagnosis (0 ‘not sure at all’ to 100 ‘very sure’).
Treatment consultation
Participants ranked the following treatment options and advices: motivational interview, exercise advise, dietary advise, increase of the oral therapy doses, switch to insulin treatment. Participants also rated how confident they were that the vignette character would follow each advice or treatment option (0 ‘not sure at all’ to 100 ‘very sure’).
2.3.2 Implicit association task (IAT)
The IAT is a standard validated task for measuring implicit biases.28 It measures implicit associations between two categories by stimuli-sorting tasks.29 Participants sorted words into different categories (e.g., man–woman, or unhealthy–healthy) that were presented either in the left or right upper corner of the computer screen. The IAT assumes that the word sorting speed increases when implicit predispositions are present and the congruent categories are presented in the same corner of the screen.29 Two potential sources of bias were assessed in two separate IATs: lifestyle (unhealthy–healthy; lifestyle IGB) and communication style (stoic-communicative; communication IGB). The Appendix S1 comprises the words included in both IATs. A d-score was calculated for each IAT that represented the difference between the congruent and non-congruent presentations of the categories.29 A d-score of 0 indicates no differences, a positive d-score indicates the presence of bias (i.e., faster during congruent blocks) and a negative d-score indicates bias in the opposite direction (faster during incongruent blocks). A positive d-score on the lifestyle IAT indicates implicit bias that females have a healthier lifestyle than males. A positive d-score on the communication IAT indicates an implicit bias that men are more stoic and less communicative than women.
2.4 Procedures
GP digitally signed informed consent prior to participation. After a short demographic survey that measured age, gender and work experience of GPs, participants rated the vignette. Next, the IATs were conducted. Which IAT (lifestyle or communication) was presented first was randomized and counterbalanced across GPs' genders. Participants could opt to skip the second IAT because of time constraints to prevent dropout. Finally, participants were debriefed and had the opportunity to partake in a lottery (€15 were raffled among each 20 participants).
2.5 Statistical analysis
Data analyses were performed two-tailed with α < 0.05 using SPSS Statistics version 21 (IBM Corporation). For the data and the code for the analysis see https://osf.io/kh6px.
d-Scores were calculated with the IATGEN tool (iatgen.wordpress.com) by taking the within-subject difference between congruent and non-congruent block means, divided by a pooled standard deviation. Data were preprocessed and the scores were calculated following the guidelines of Greenwald and colleagues.30 To investigate whether implicit biases were present, d-scores on the lifestyle and communication IAT were compared to 0 with one-sample t-tests. Independent samples t-tests were used to compare d-scores between male and female GPs. Cohen's d was calculated as an estimate of the effect size, with d = 0.20, 0.50 and 0.80 interpreted as small, medium and large effects, respectively.31
Factorial 2 × 2 (vignette character's gender vs. GP's gender) analysis of variance (ANOVA) was used to associate the GP's and patient's gender with the medical vignette outcomes: diagnosis, certainty of diagnosis, preferred advice and certainty of the patient's compliance with the advice. Aligned Rank Transform ANOVA32 was used to analyse vignette outcomes that were not normally distributed or contained outliers.
Pearson's correlations were calculated to investigate relationships between d-scores and the medical vignettes outcomes for male and female vignette character separately, and for male and female GPs separately. Because of the study's exploratory nature, no corrections for multiple comparisons were made.
3 RESULTS
3.1 Demographic characteristics
Data collection started on 27 January 2020 and, due to the global outbreak of COVID-19, stopped prematurely in March 2020. The final study sample consisted of 100 GPs who completed at least one part of the study. The number of GPs that completed different parts of the study is presented in Table 1. Fifty-nine GPs (59.6%) were still in training, 37 (36.6%) GPs worked in primary care, 1 (1%) worked in an academic hospital, 1 (1%) worked for Doctors without Borders, the primary work of another 1 (1%) was a university professor and one reported ‘other specialization’ without further specification. Mean work experience was 17.0 years (SD = 8.6) for GPs. GP trainees on average had 1.5 years (SD = 0.8) of experience as a trainee. Thirty-two participants (32%) were men, 67 (67%) women and 1 (1%) preferred not to report their gender.
| Variable | N completed |
|---|---|
| Demographics survey | 100 |
| Vignette: diagnosis | 99 |
| Vignette: certainty of the diagnosis of diabetes | 99 |
| Vignette: treatment advice | 95 |
| Vignette: certainty of following the advice | 95 |
| Communication style implicit bias | 67 |
| Lifestyle implicit bias | 70 |
| Gender roles questionnaire | 57 |
3.2 Vignettes
Regardless of the vignette character's gender, female GPs gave a higher likelihood to the vignette character having type 2 diabetes than male GPs (F(1,90) = 5.51, p = 0.021, Cohen's d = 0.53) at the initial consultation (Table 2). In the diagnosis phase, based on the HbA1c results, both male and female GPs were more certain that the male vignette character had type 2 diabetes than the female vignette character (F(1,90) = 24,38, p < 0.001, Cohen's d = 1.03). There was a significant interaction between GPs' and vignette character's genders on the GPs' certainty about the character's willingness to follow oral therapy advice (F(1, 36) = 10.69, p = 0.002, Cohen's d = 0.69): male GPs were more certain that a male character would follow the advice about oral therapy better, while female GPs were more certain about the willingness of a female versus male vignette character to follow the advice. Regardless of GPs' gender, the female character was more likely to be referred to a dietician compared to the male character (F(1, 90) = 5.52, p = 0.021, Cohen's d = 0.49). Finally, there was a significant interaction effect between GPs' and vignette character's gender on the priority of motivational interviewing (F(1,90) = 10,6, p = 0.002, Cohen's d = 0.68): female GPs gave a higher priority to a motivational interview than male GPs (F(1,90) = 6.16, p = 0.015, Cohen's d = 0.56) regardless of the vignette character's gender, whereas male GPs prioritized the motivational interview with a male character more than with a female character (F(1,90) = 4.11, p = 0.046, Cohen's d = 0.42).
| Male GPs | Female GPs | |||
|---|---|---|---|---|
| Male character | Female character | Male character | Female character | |
| Chance of the character having type 2 diabetes (0–100) | 40.26 (28.18) | 42.82 (28.63) | 60.21 (24.95) | 49.83 (22.71) |
| Chance of the character with HbA1c of 48 mmol/mol having type 2 diabetes | 56.05 (30.19) | 45.00 (28.35) | 50.18 (29.79) | 49.33 (28.53) |
| Certainty about type 2 diabetes diagnosis (0–100) | 61.11 (25.21) | 29.36 (33.27) | 57.54 (31.05) | 22.36 (29.91) |
| Advice priority: increase of oral therapya | 3.58 (1.35) | 3.45 (0.93) | 3.75 (0.967) | 3.72 (1.34) |
| Advice priority: switch to insulina | 4.16 (1.30) | 3.91 (1.58) | 4.68 (0.67) | 4.64 (1.58) |
| Advice priority: dietary plana | 2.53 (0.77) | 1.91 (0.30) | 2.39 (0.83) | 2.25 (0.48) |
| Advice priority: sporta | 3.21 (1.03) | 3.36 (1.12) | 3.00 (0.77) | 2.94 (0.72) |
| Advice priority: motivational interviewa | 1.53 (1.02) | 2.36 (1.80) | 1.18 (0.61) | 1.44 (0.84) |
| Likelihood of following the advice: increase of oral therapy (0–100) | 74.42 (16.59) | 52.82 (26.10) | 66.75 (24.37) | 75.56 (16.32) |
| Likelihood of following the advice: switch to insulin (0–100) | 22.68 (16.89) | 27.09 (20.99) | 24.10 (21.94) | 30.61 (19.25) |
| Likelihood of following the advice: dietary plan (0–100) | 37.95 (17.88) | 34.18 (18.09) | 34.68 (19.67) | 39.67 (15.90) |
| Likelihood of following the advice: sport (0–100) | 27.26 (13.55) | 17.91 (14.65) | 31.36 (20.10) | 30.11 (17.39) |
- a Advice priority is measured in the rank where 1 indicates highest priority and 5 lowest.
3.3 Implicit biases
Due to exceeding 10,000 ms response time, 0.04% of all IAT responses were deleted. Incorrect responses (4.9%), that is wrong category chosen, were also deleted from the analysis as recommended by the standard cleaning protocol.29
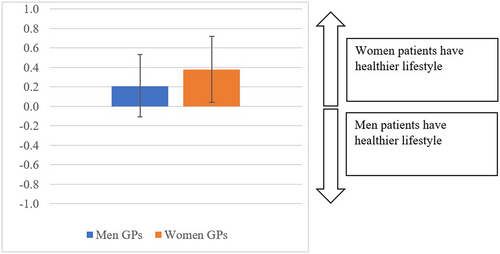
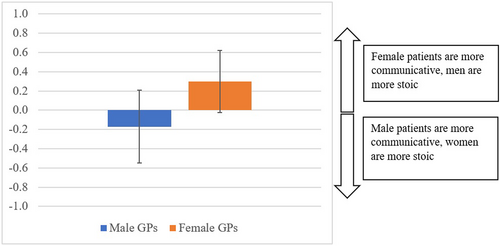
Significant lifestyle IGB was found (t(69) = 3.25, p = 0.002, Cohen's d = 0.39; Figures 1 and 2). Lifestyle bias differed according to GPs' gender: female GPs showed larger bias that women have a healthier lifestyle than men (t(48) = 6.41, p < 0.001, Cohen's d = 0.91). There was a trend in male GPs for the opposite bias, that men have a healthier lifestyle than women (t(20)= − 2.08, p = 0.051, Cohen's d = 0.45). GPs had a significant communication IGB (t(66) = 7.44, p < 0.001, Cohen's d = 0.91), that women are more communicative than men. The communication bias was larger in female than male GP's (t(65) = 2.65, p = 0.01, Cohen's d = 0.71).
3.4 Associations between implicit biases and clinical decisions
A larger communication IGB in GPs was associated with a lower certainty of GPs about the diagnosis of type 2 diabetes based on HbA1c in a male vignette character (r(30) = 0.40, p = 0.042). Lower lifestyle bias (that men have unhealthy lifestyle) was associated with a higher priority to recommend the motivational interview to a male vignette character (r(30) = − 0.37, p = 0.026). The IGB that women have a more healthy lifestyle was associated with higher priority to recommend sports to women (r(30) = 0.52, p = 0.002). Male GPs were less certain about the diagnosis of type 2 diabetes based on HbA1c when they viewed gender roles as less equal in household (r(14) = − 0.57, p = 0.034), childcare (r(14) = − 0.66, p = 0.011) and work tasks (r(14) = − 0.56, p = 0.037). No other correlation analyses were significant (p > 0.059; Appendix S1).
4 DISCUSSION
The aim of this study was to investigate whether GPs in the Netherlands have IGBs regarding lifestyle and communication styles of their patients, and whether these biases and patient's and GP's own gender affect clinical decisions of GPs in diagnosis and treatment of type 2 diabetes. We found that both implicit biases were present in GPs. Moreover, IGBs and vignette character's gender were associated with GP's decisions in a type 2 diabetes vignette case.
To our knowledge, only one study so far used a validated Implicit Bias Test to investigate IGBs in healthcare professionals and its potential influence on medical decision making.33 It looked at a doctors' bias that men are stronger and more prone to risk-taking than women, and the association of these biases with the clinical decisions regarding coronary artery disease. Our study is the first to apply implicit bias measures in the context of type 2 diabetes. We have chosen lifestyle and communication style biases as lifestyle is an important factor in the development of type 2 diabetes,23 while communication can influence patient-doctor relationships.24
Our study confirmed the hypothesized existence of IGBs in GPs. The lifestyle bias differed by the GP's gender, and GPs tended to ascribe a healthier lifestyle to vignette characters of their own gender. These findings correspond to literature that showed that people tend to have more positive biases towards their own gender.20, 21 GPs of both genders had an IGB that women are more communicative, while men are more reserved and stoic. Research confirms that women in general tend to disclose more information during the medical communication.34 However, applying such knowledge to individual treatment might lead to inequality if concerns presented by women are taken less seriously than those of men.34
Importantly, IGBs correlated with several decision-making measures. Higher communication bias was associated with the lower certainty of GPs in the diagnosis of type 2 diabetes based on HbA1c in a male vignette character. Possibly, if GPs expect men to be less communicative, they might assume that they do not receive enough information for the diagnosis which then promotes uncertainty. Moreover, implicit biases were associated with the priority of the GPs' provided treatment advice. When GPs implicitly considered men as having a healthier lifestyle, they tended to prioritize a motivational interview for a male vignette character. A higher IGB that women have healthier lifestyle prioritized recommending sports to women. Therefore, it can be speculated that when GPs are implicitly more convinced that individuals of a certain gender have a healthier lifestyle, they prioritize advice related to this lifestyle for this gender.
This is the first study to look at the impact of patient's gender on clinical decision making in type 2 diabetes. We demonstrated that when a male vignette character has an HbA1c of 48 mmol/mol, GPs are more certain of the diagnosis of diabetes in comparison to when the character is a woman. While in some countries HbA1c of 48 mmol/mol is the blood level for diagnosing type 2 diabetes, the Dutch guidelines for type 2 diabetes diagnostics do not mention HbA1c but rather glucose levels combined with the hyperglycaemia complaints.27 We have explicitly chosen a measurement that is not a necessarily a clear marker for the diagnosis to study the decisions of doctors in a relatively ambiguous situation. Heightened HbA1c levels, in combination with other symptoms described by the vignette character, should be a reasonable indication for the diagnosis of type 2 diabetes. It remains unclear why the GPs were more certain that a male vignette character with these symptoms had type 2 diabetes rather than a female character. Previous research found that women tend to be diagnosed with type 2 diabetes at a later stage that men.14 Our study demonstrated that this delay might be related to lower certainty of GPs about a type 2 diabetes diagnosis in women. There was no relation between certainty and IGBs however; therefore, it remains unclear what makes GPs less certain about diagnosing women with type 2 diabetes. Future research should pinpoint the reasons for this phenomenon as it is essential to ensure that every person receives a timely diagnosis regardless of their gender.
We also found that patient–GP gender interaction affects the GPs' certainty that a vignette character will follow the oral therapy advice: male GPs thought that a male character would follow the advice about oral therapy better than a female character, while female GPs were more certain that a female vignette character would follow this advice. Also, male GPs prioritize the motivational talk with a male vignette character more than with a female character. Possibly, these findings again suggest that GPs have a general more positive bias towards their own gender. At the same time, this bias did not manifest in all parts of the vignette; therefore, it might be not a very robust phenomenon.
Finally, female GPs gave a higher priority for a motivational talk in general, which corresponds to the previous findings that female physicians tend to have longer visits and engage in more positive talk, ask more questions and give more information than male physicians.35, 36
Our study has several limitations that have to be addressed. The initial sample size was planned to be twice as large. Due to the COVID-19 pandemic, the study had to be stopped prematurely, as it would have been unethical to ask for time investment from the physicians at that moment. Certainly, a larger sample would make our results more robust and generalizable. At the same time, there are several other studies with IAT with sample sizes comparable with our final sample size.37, 38 Another limitation is that our sample included many GPs who were still in training. We recruited only GPs starting from the second year of their training to ensure that they already had some clinical experience, but it is still possible that their experience with type 2 diabetes is limited. Finally, we emphasize the exploratory nature of this study. Because implicit biases were never investigated in the context of type 2 diabetes before, we did not have directional hypotheses on several of our research questions and performed multiple exploratory analyses to investigate possible connections between our measures. The current results highlight areas for further study and allow follow-up research to have directional hypotheses and target certain aspects of clinical decisions, for example, early diagnosis of type 2 diabetes in women.
Overall, our study demonstrated that gender and IGBs are related to GPs' decision making in diagnosis and treatment of type 2 diabetes. IGBs might be one of the causes of discrepancies in the diabetes care that men and women receive. Follow-up research should focus on the areas highlighted by our study (e.g. certainty of GPs while diagnosing women and the communication gender bias) and investigate directional hypotheses with large enough samples. Understanding the role of gender biases and gender in medical decision making is an important first step towards limiting their negative impact in healthcare. Research shows that IGBs are malleable and can be changed by deliberate strategies.39 Therefore, clinicians should be made aware of their possible biases and about techniques to overcome them as a part of their education. By addressing this topic, we might be able to close the gender gap in the quality of care and guarantee that every person gets the best care possible regardless of their gender.
AUTHOR CONTRIBUTIONS
All authors contributed to the design of the study. A. Skvortsova and S. H. Meeuwis created the surveys, conducted the statistical analyses, and wrote the first draft of the manuscript. R. C. Vos, H. M. M. Vos, D. S. Veldhuijzen, H. van Middendorp and A. W. M. Evers provided input for the manuscript and commented on the text. All authors read and approved of the final draft.
ACKNOWLEDGEMENTS
We would like to thank all GPs and GP trainees who participated in this study.
FUNDING INFORMATION
The study was funded by the Diabetes Fonds and the Netherlands Organization for Health Research and Development ZonMW.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are openly available in OSF at https://osf.io/kh6px/, reference number kh6px.