Diabetes-related major lower limb amputation incidence is strongly related to diabetic foot service provision and improves with enhancement of services: peer review of the South-West of England
Abstract
Aims
To investigate the relationship between high diabetes-related lower limb amputation incidence and foot care services in the South-West region of England.
Methods
The introduction of 10 key elements of foot care service provision in one area of the South-West resulted in stabilization of foot ulcer incidence and sustained reduction in amputation incidence from 2007. Services introduced included administrative support, standardized general practice foot screening, improved community podiatry staffing, hospital multidisciplinary foot clinics, effective care pathways, availability of an orthotist and audit. Peer reviews of the region's diabetes foot care services were undertaken to assess delivery of these service provisions and compare this with major amputation incidence in other regions with data provided by Yorkshire and Humber Public Health Observatory Hospital Episode Statistics. Recommendations were made to improve service provision. In 2015 changes in service provision and amputation incidence were reviewed.
Results
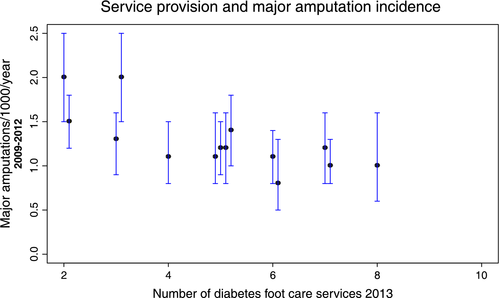
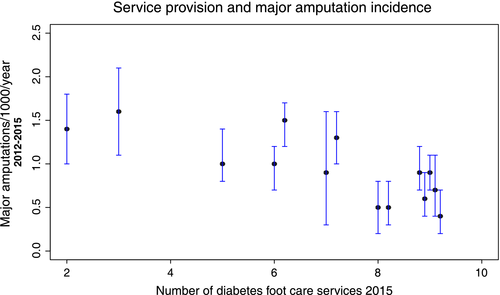
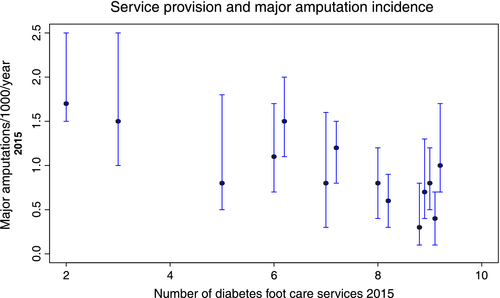
Initial reviews in 2013 showed that the 3-year diabetes-related major amputation incidence correlated inversely with adequate delivery of diabetes foot care services (P=0.0024, adjusted R2 =0.51). Repeat reviews in 2015 found that two or more foot care service improvements were reported by six diabetes foot care providers, with improvement in outcomes. The negative relationship between major amputation incidence and service provision remained strong both in the period 2012–2015 and in the year 2015 only (P ≤0.0012, adjusted R2 =0.56, and P= 0.0005, R2=0.62, respectively).
Conclusions
Major diabetes-related lower limb amputation incidence is significantly inversely correlated with foot care services provision. Introduction of more effective service provision resulted in significant reductions in major amputation incidence within 2 years. Failure to improve unsatisfactory service provision resulted in continued high amputation incidence.
What's new?
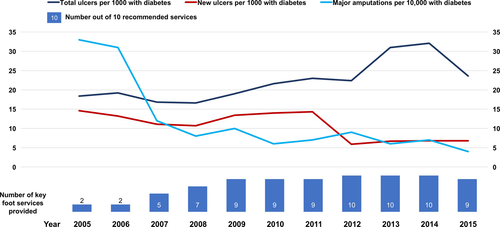
- The 10-year incidence and prevalence of diabetic foot ulcer and amputation incidence were recorded and compared with service provision in one Clinical Commissioning Group [the National Health Service (NHS) funding body for hospital and community services in each area of the UK].
- Evaluation of the effective delivery of 10 key diabetes foot care service provisions was undertaken in 14 service providers in one NHS region.
- There was a strong negative relationship between provision of 10 key services for diabetes foot care and major diabetes-related lower limb amputation rates.
- Improvement in diabetes foot care services resulted in a reduction in major amputation incidence within 2 years.
- The acceptability and effectiveness of peer review in evaluating diabetes foot care services were demonstrated across a whole region of England.
Introduction
Of people living with diabetes, 20% will have an increased risk of foot ulceration as a result of neuropathy 1-3. Peripheral arterial disease is also common and can be difficult to diagnose in the presence of diabetes 4, 5. Up to 7% of people living with diabetes in the UK have current or previous foot ulceration and are at high risk of recurrence 6. Progression from ulceration to amputation is often associated with co-existing peripheral arterial disease, and a range of other factors, including ethnicity 7, 8. The South-West region of England has a total population of 5.5 million, of whom 8.6% were living with diabetes in 2015. More than 95% of these people were of white British ethnicity, a group at high risk of diabetes-related amputation. Diabetes-related major and total lower limb amputation incidence has historically been very high across most of the South-West region; however, incidence rates in different parts of the South-West region vary from 0.5 to 2.5 per 1000 persons living with diabetes per annum [Health Episode Statistics (HES)] 9. This suggests that differences in care between areas may affect outcomes. The range of factors which may influence diabetes foot care outcomes in the UK have been well summarized 10. Delays in referral of serious foot problems are of particular concern. In the UK, National Health Service (NHS) annual review in general practice offers the best opportunity to provide consistent regular foot examination and education to all people living with diabetes. It is crucial for achievement of success that practice nurses are themselves educated to perform foot examination correctly and to provide appropriate advice. Referral of those at high risk to an adequately staffed podiatry service and, if necessary, prompt review in secondary care, including vascular surgery, is essential 11, 12.
A sustained reduction in diabetes-related lower limb amputation was observed after the institution of job-planned multidisciplinary secondary care diabetic foot clinics 13-15, while an earlier report showed a continued high amputation incidence over a decade where no restructuring of services was undertaken 16. Diabetes foot care services in England are commissioned by Clinical Commissioning Groups (CCGs). CCGs are clinically led statutory NHS bodies which are responsible for the planning and commissioning of healthcare services for their local area; however, as this process is not standardized, there can be wide variation in funding for diabetes foot care services between providers even within the same CCG. Vascular services are mandated separately as part of centrally funded specialized NHS commissioning, but access to these also varies between CCGs. A recent joint specialty recommendation highlights the need for integrated care in hospital-based diabetic foot services 17. One diabetes foot care service in the South-West region, South Devon, experienced very high diabetes-related major amputation rates: >3/1000/year in the period 2005 to 2007 (the NHS average for England was 1.1/1000/year). The successful introduction of service improvements and the incidence rates of diabetic foot ulcer and major amputation have been closely correlated. These service improvements have been used as standards in peer reviews of all foot care providers in the region to highlight the successes of and challenges that arise in integrated diabetic foot care. Outcomes of peer reviews have been monitored to assess the impact of enhancement of diabetic foot care services.
Methods
Evaluation of key service provisions for diabetes foot care
Root cause analysis of major amputations in 2005 and 2006 highlighted delays in treatment of diabetes-related foot ulcers at all stages of care in one area of the South-West, South Devon. This included lack of awareness of foot risk amongst service users, delay in presentation of foot ulcers and referral to podiatry, absence of foot care pathways, and delay in referral to the multidisciplinary foot clinic. There was no administrative support for the foot service. All of these issues were addressed after 2007. A significant reduction in the rate of major amputation was achieved over the ensuing 8 years.
Ulcer incidence and prevalence in South Devon
Community podiatrists in South Devon recorded all diabetes-related foot ulcer consultations from 2007 onwards on a shared data base. These data are collated annually to determine annual ulcer prevalence. The annual ulcer incidence rate was derived from the number of new diabetes-related foot ulcers in that year.
Amputation incidence
The incidence rate for major diabetes-related amputation was taken from vascular surgical records, and HES methodology-compatible searches of foot care activity profiles in the South Devon health economy. Annual data are shown to clarify the relationship between service provision and outcomes. The 3-year HES statistics for the South Devon CCG are consistent with these amputation numbers. The improvements in diabetic foot care service provision and associated decrease in major amputation and ulcer incidence rates from 2007 are shown in Fig. 1. A reduction in the incidence of amputation over time (P=0.0115, z value=–2.526, residual deviance=3.4), was calculated in a Poisson regression of log-transformed number of major amputations with a right side offset of patient population by year using statistical software ‘R’. The recommended service provisions and criteria used to score their effective delivery are shown in Table 1.
| Commissioning recommendations key for effective diabetic foot care services | Criteria for adequacy of services |
|---|---|
| Patient education at annual review | Confirmation by general practice lead and patients at interview |
| Regular community healthcare professional education | Confirmation by general practice and podiatry leads and evidence of education programme |
| Adequate podiatry community staffing with rotation in to MDFT | Comparison of service with Society for Podiatry guidelines and confirmation by podiatrists |
| Job planned MDFT weekly | Evidence from clinic records and MDFT members |
| Administrative support | Interview with A&C staff, Podiatry and MDFT leads |
| Pathways and communication of plan of care to patient | Confirmation by patients at interview, documentation in notes, and examples of summary sheet of patient care pathway |
| Identification of diabetic in-patients and their foot checks | Evidence of Information technology used to identify patients and protocol for foot assessment |
| Orthotist an integral part of MDFT | Review of MDFT clinic |
| Urgent vascular opinion available to foot clinic staff | Review of MDFT clinic |
| Ulcer database and root cause analysis of all amputations | Review of results of data base and analyses. |
- A&C staff, administrative and clerical staff; MDFT, multidisciplinary diabetic foot team
Peer review of the entire South-West region
Peer review of the entire South-West region was undertaken using the 10 service provisions shown in Table 1 as standards to score each service. The region can be divided into 14 diabetes foot care service providers–health economies, which comprise a district general hospital, a community podiatry service and linked general practices. Peer reviews assessed diabetes foot care service provision by each of these diabetes foot care service providers in 2013 and the review process was repeated in 2015.
These data were then correlated with major diabetes-related amputation incidence rates for the periods 2009–2012 and 2012–2015. The 2015 service provision was also correlated with major amputation incidence in the calendar year 2015 only. Major amputation incidence was taken from HES (major amputation statistics in England are extracted by the Yorkshire and Humber Public Health Observatory from payment for hospital episode statistics using coding formulae: X093: amputation of leg above knee; X094: amputation of leg through knee; X095: amputation of leg below knee; X098: other specified amputation of leg; X099: unspecified amputation of leg). In the New Devon and Bristol CCGs, HES data do not distinguish outcomes from separate service providers within these CCGs. Major amputation incidence rates were calculated separately for those provider areas (North Devon, West Devon, East Devon, North Bristol Hospital Trust and United Bristol Hospital). For these service providers, major amputation incidence rates were measured using methods commensurate with HES data acquisition by CCGs.
The podiatry services, CCGs and District General Hospitals participating in the reviews are listed in Appendix S2.
Format of peer reviews
Initial reviews
The initial reviews in 2013 were conducted by two diabetologists, two lead podiatrists and an NHS England quality improvement lead. Amputation incidence, hospital and podiatry staffing levels, care and referral pathways were all available to the peer review team in advance. Hospital foot clinic facilities were assessed and staff interviewed. The service was also discussed with diabetes foot clinic attendees, the community podiatry service provider, the CCG general practice diabetes lead and orthotist. Evidence of care plans were sought in the hospital notes of foot clinic attendees. Recommendations for consolidation and enhancement of services were made within 2 weeks of the peer review visit.
Repeat reviews
As in 2013, in advance of the 2015 peer reviews, all service providers were asked to make available preliminary information on total population, the number of people aged >17 years registered with diabetes, podiatry providers and staffing levels. Each review panel included two diabetologists, two lead podiatrists, a vascular surgeon, an NHS quality improvement lead and an orthopaedic/podiatric surgeon. Reviewing clinicians were not directly involved in the services that they reviewed. The second review process also included 10 formal patient record reviews and four structured patient interviews at each visit. Contacts made in the peer reviews are shown in Table 2.
| Contacts made for peer reviews and staff in attendance | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Provider service | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | Total |
| Amputee interviews | 4 | 4 | 4 | 3 | 6 | 5 | 3 | 3 | 2 | 4 | 4 | 3 | 4 | 3 | 50 |
| Notes reviews | 6 | 6 | 10 | 6 | 12 | 7 | 10 | 7 | 10 | 10 | 10 | 3 | 10 | 10 | 122 |
| Practice leads | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 15 |
| CCG diabetes leads | 2 | 1 | 1 | 1 | 2 | 3 | 1 | 1 | 1 | 1 | 2 | 1 | 2 | 1 | 19 |
| Community podiatry | 2 | 2 | 1 | 2 | 2 | 1 | 2 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 19 |
| Hospital podiatry | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 1 | 1 | 2 | 2 | 2 | 1 | 22 |
| Orthotists | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 11 |
| Diabetes specialists | 1 | 3 | 1 | 2 | 2 | 1 | 2 | 1 | 1 | 1 | 3 | 1 | 1 | 2 | 21 |
| Vascular surgeons | 0 | 4 | 1 | 1 | 2 | 1 | 2 | 1 | 1 | 1 | 4 | 0 | 0 | 2 | 19 |
| Orthopaedic surgeons | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 2 | 1 | 11 |
| A&C support | 0 | 1 | 1 | 0 | 0 | 1 | 2 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 8 |
| Hospital management | 2 | 2 | 3 | 3 | 4 | 4 | 2 | 2 | 3 | 2 | 2 | 1 | 3 | 1 | 34 |
- A&C support, administrative and clerical support; CCG, Clinical Commissioning Group.
Timetable of review visit
The review visit included the following:
- a 1-h initial discussion with all reviewers and service providers, including completion of a checklist to verify which diabetes foot care services were provided in the area;
- in-depth recorded interviews of four current multidisciplinary foot clinic attendees which were identified by convenience sampling and for which consent was obtained before the review day (recordings were destroyed after transcription and data anonymized);
- a review of 10 randomly selected sets of multidisciplinary foot clinic and podiatry user records;
- separate discussions with general practitioners, CCG diabetes leads, community and hospital podiatrists, multidisciplinary team physicians, surgeons and orthotists;
- a feed-back session at the end of the day;
- a report format which reflected the status of 10 key services provisions in the area;
- recommendations for consolidation of good practice and future improvements;
- a standardized formal report with recommendations, which was sent to Trust Chief Executives, CCG Chairs and providers within 21 days of each visit.
Statistics
Major (above-ankle) lower extremity amputation rates (HES) were analysed using the 10-year data from the South Devon provider service, and for correlations with service provision across the region. A general linear model, including log number of people with diabetes, was used to test significance of change in amputation incidence with time using programme ‘R’. The CIs for 3-year major amputation incidence in each service provider area in 2009–2012 and 2012–2015 were taken from HES reports and HES methodology-compatible searches of foot care activity profiles for individual service providers in the New Devon and Bristol CCGs. The CIs for 1-year (2015) major amputation incidences were calculated from the combined variances of numbers of people with diabetes in each provider area and amputation numbers in each area. The relationship between amputation incidence and service provision was tested by least squares mean regression.
Results
Figure 2 summarizes the audit of case records and results of structured interviews.
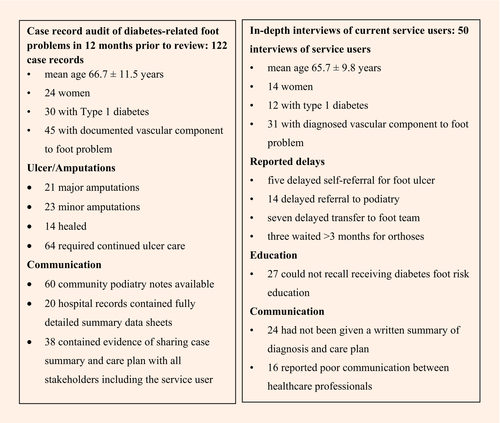
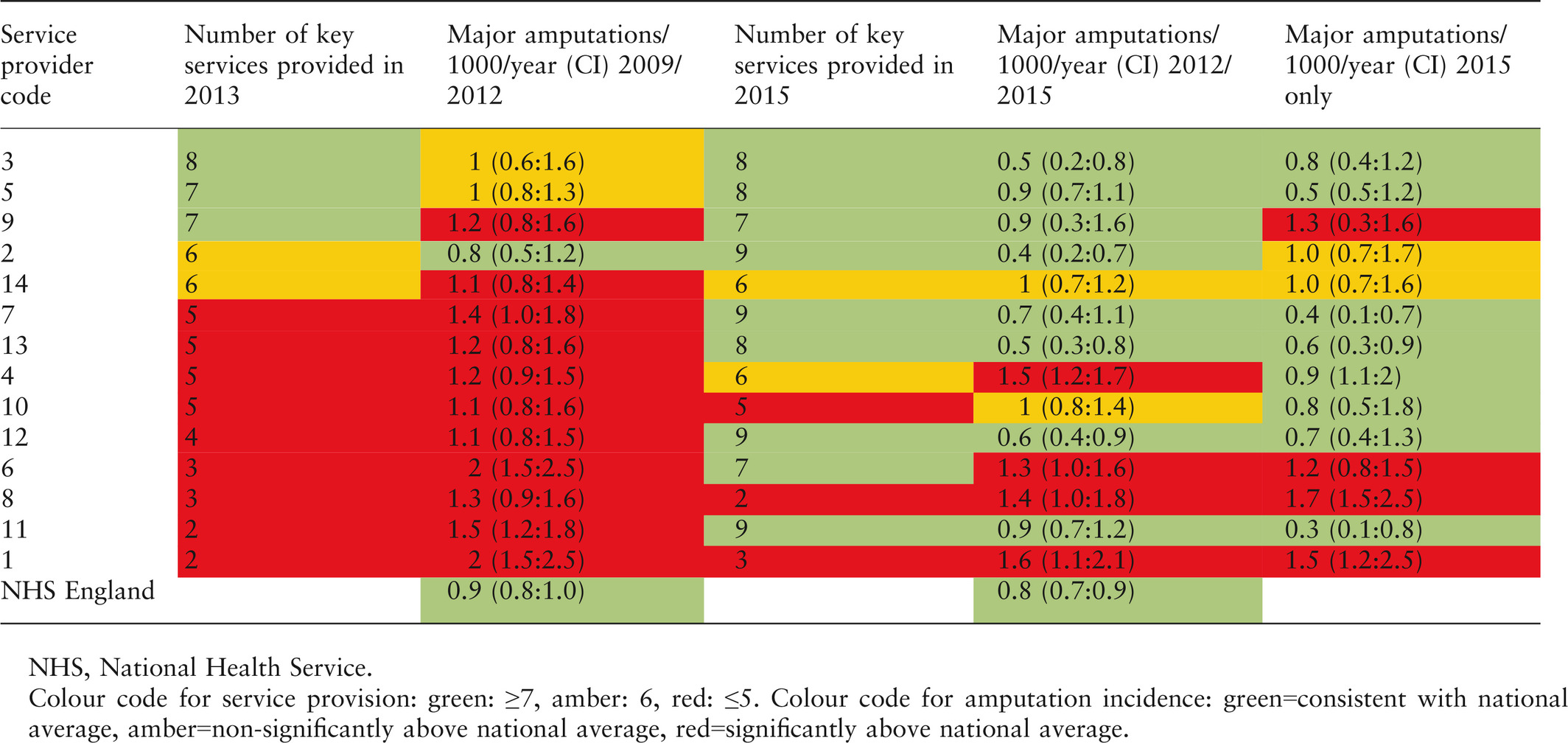
Table 3 shows the foot care service provisions in place before 2013 and in 2015 among the 14 service providers.
| Commissioning recommendations key for effective diabetic footcare services | Diabetes foot care service provision in each provider service area in 2013 and in 2015 noted as 2013/2015 in each cell | Providers with each service | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Service provider code | 3 | 5 | 9 | 2 | 14 | 7 | 13 | 4 | 10 | 12 | 6 | 8 | 11 | 1 | 2013/2015 |
| Patient education at annual review | Y/Y | Y/Y | Y/Y | Y/Y | Y/Y | Y/Y | N/Y | Y/Y | N/N | N/Y | Y/Y | Y/Y | N/Y | N/Y | 9/13 |
| Regular community healthcare professional education | Y/Y | Y/Y | N/Y | N/N | N/N | N/Y | N/Y | N/Y | N/N | N/Y | N/N | N/N | N/Y | N/N | 2/8 |
| Adequate podiatry numbers, skill mix with rotation into MDFT | Y/Y | N/Y | N/N | N/Y | Y/Y | N/Y | Y/N | Y/N | N/N | N/Y | N/N | N/N | N/Y | N/N | 4/7 |
| Job planned MDFT weekly | Y/Y | Y/Y | Y/Y | Y/Y | Y/Y | Y/Y | Y/Y | N/Y | Y/Y | Y/N | N/Y | N/N | N/Y | N/N | 9/11 |
| Administrative support | Y/Y | Y/Y | Y/Y | Y/Y | Y/N | Y/Y | N/Y | Y/N | N/N | N/Y | N/N | N/N | Y/Y | N/N | 8/8 |
| Pathways and communication of plan of care to patient | Y/Y | Y/Y | Y/N | N/Y | Y/Y | Y/Y | N/N | N/Y | Y/Y | Y/Y | N/Y | N/N | N/Y | N/N | 7/10 |
| Identification of diabetic in-patients and their foot checks | N/N | N/N | N/N | N/Y | N/N | N/Y | Y/Y | N/N | N/Y | N/Y | N/N | N/N | N/N | N/N | 1/5 |
| Orthotist an integral part of MDFT | N/N | Y/Y | Y/Y | Y/Y | N/N | N/N | Y/Y | Y/Y | Y/Y | Y/Y | Y/Y | N/N | Y/Y | Y/Y | 10/10 |
| Urgent vascular opinion available to foot clinic staff | Y/Y | Y/Y | Y/Y | Y/Y | Y/Y | Y/Y | Y/Y | Y/Y | Y/Y | Y/Y | Y/Y | Y/Y | N/Y | Y/Y | 13/14 |
| Ulcer database and root cause analysis of all amputations | Y/Y | N/N | Y/Y | Y/Y | Y/Y | N/Y | N/Y | N/N | Y/N | N/Y | N/N | N/N | N/Y | N/N | 5/8 |
| Number of services available in each area | 8/8 | 7/8 | 7/7 | 6/9 | 7/6 | 5/9 | 5/8 | 5/6 | 5/5 | 4/9 | 3/5 | 2/2 | 2/9 | 2/3 | |
- MDFT, multidisciplinary diabetic foot team; N, not present; Y, verified as present.
The incidence of major amputation in the period 2009–2012 across the region was significantly negatively correlated with the number of key foot care service provisions available out of the 10 provisions in place at the 2013 peer reviews [P=0.0024, adjusted R2 = 0.51, F-statistic=14.6 (Fig. 3)]. This association was maintained when major amputation incidence in the period 2012 to 2015 was correlated with service provision in 2015 [P=0.0012, R2 =0.56, F-statistic = 17.16 (Fig. 4)]. As some provider services had made improvements in service provision only after 2014, a further correlation was made between major amputation incidence in 2015 only and service provision in 2015. A significant negative association was still observed [P≤0.0005, adjusted R2=0.62, F-statistic=22.1 (Fig. 5)]. Table 4 provides a traffic light colour-coded summary of service provision and major amputation rates by service provider.
Discussion
The diabetes foot care peer reviews reported in the present study relied on full collaboration of teams across the South-West region, bringing together a diverse group of 100 clinicians from multiple providers, all seeking to improve clinical outcomes for people with diabetes and diabetic foot disease. Scoring of the adequacy of diabetes foot care in each provider area was based on those services introduced from 2008 in South Devon. The introduction of the 10 key services shown in Table 1 was accompanied by a sustained reduction in major diabetes-related amputation incidence. There was also a trend towards a reduction in diabetic foot ulcer incidence in the South Devon CCG. The foot ulcer prevalence of 24/1000 is consistent with other UK figures 18. Future reductions in diabetes-related foot ulcer incidence in successful service provider areas would indicate that the service provisions recommended were effective in ulcer prevention as well as in reduction in major amputation incidence.
The strong correlation between service provision and major amputation incidence was validated in the first peer review and confirmed in the second.
A reduction in major amputation incidence has occurred within 2 years of improvement in diabetic foot care service provision in seven provider services. In two provider areas only two and three of the 10 recommended diabetes foot services, respectively, have been sustained, and this has been accompanied by a continued high incidence of major amputation.
The recent economic analysis of the cost of diabetic foot ulcers in England has estimated the cost of treatment of diabetic foot ulcers in the community to be £0.97–1.1 m per annum in England. Ulcer severity measured by SINBAD score (severity of ulcer by depth, infection, size, ischaemia, neuropathy and site)affects the cost of treatment. Total annual cost for diabetic foot ulcers with SINBAD score ≤2 is £126–157m, compared to £503–629m where SINBAD score if ≥3 19. This underlines the need for integration of all diabetes foot care services in order to reduce the incidence and severity of foot ulceration as well as prevent avoidable amputations. This report also confirms the major cost savings that result from reductions in diabetes-related major lower limb amputation. The cost of major amputation averaged per person living with diabetes reduced from £22.1 to £4.5 per annum when major amputation incidence reduced from 1.1 to 0.6/1000 in South Devon. Some of the shortfalls in diabetic foot care services in the South-West region are readily remedied without additional costs. In particular, referral pathways, job planning, coordination via effective pathways, better commissioning of orthotics and rotation of community podiatrists into the multidisciplinary diabetes foot team. Training of practice staff in diabetic foot examination and care can be carried out free online 20-22. Commissioning of podiatry services may incur significant costs to meet the need for review of high-risk individuals, but this expenditure is offset by the reduction in costs associated with amputations 19. The provision of vascular services for diabetes-related foot disease associated with ischaemia has become focused in arterial centres. Seven-day-per-week availability of emergency care for critically ischaemic diabetic foot problems can be offered by an arterial centre for more than one provider area (district general hospital, community podiatry and associated general practices). The vascular surgical staff at the arterial hub can also support non-arterial centre multidisciplinary foot clinics 23.
The peer reviews reported in the present study have shown that the introduction of a range of key foot care services can reduce the incidence of major diabetes-related lower limb amputation. As has been seen with stroke, cardiovascular and cancer services, administrative support is essential to record and analyse performance 24. The very wide variation in diabetic foot care services among providers in the South-West region demonstrates the need for commissioning guidelines.
A strength of the present study was the inclusion of all those involved with the care of those living with diabetes and diabetic foot-related problems. Contemporary data were used to match service provision against major amputation incidence. A potential weakness of the study is that 95% of the population of the region was white British. It is possible that our findings may not apply to areas where the population with diabetes is predominantly South Asian or Afro Caribbean. The robustness and reproducibility of the data used in the present report are important if they are to be used to guide diabetes foot care commissioning. The independent variable in our analyses was quality of service provision scored out of 10. We accepted adequacy of each particular service provision if case notes, service user feedback, and reviewee's evidence confirmed its effective delivery. These criteria are outlined in Table 1. All the reviewers collaborated in writing peer review recommendations including the decision to accept or not the effectiveness of services. In the case of administrative support there should be dedicated administrative and clerical staff to support community and hospital clinicians and coordinate care. The podiatry service should be fully staffed with an appropriate skill mix for the population living with diabetes. A NICE compliant multidisciplinary diabetic foot clinic should take place weekly, be job planned and have no waiting list for urgent referrals. Pathways should be widely known, accessible and easy to use with reliable response from an administrator via the telephone numbers cited in the document. It is not possible for us to quantify the contribution of each separate service provision to reduction in major amputation incidence; however, the provision of a multidisciplinary foot clinic with less than five of the other key services was not sufficient to reduce high major amputation incidence. The quality of service score out of 10 was reflected in each case by the recommendations made to commissioners at each peer review. The dependent variable was incidence of major diabetes-related lower limb amputation. Amputation incidence in each service provider area was calculated using the number of people living with diabetes according to general practice records as the denominator. This figure may be an underestimate of true prevalence of diabetes, but did not show unexpectedly large variation in the South-West region during this study.
The National Diabetes Foot Audit, commenced in 2015, is a key step in focusing on causative factors which have led to potentially avoidable diabetes-related lower limb amputation 25. Participation in this audit is an essential part of an adequately commissioned service. This can be developed further by root cause analysis of diabetes-related lower limb amputations 26. The protocol of peer review presented in this work may well be applicable to other clinical services. Clinically led peer reviews have previously proved effective in improving stroke services 27.
In conclusion, peer reviews of diabetic foot services in the South-West region have shown a powerful negative correlation between major amputation incidence and service provision. Based on these findings we strongly recommend robust commissioning to provide and coordinate 10 key service provisions for diabetic foot care in all CCGs.
Funding sources
This study was supported by the South-West Regional Cardiovascular Disease Network. Clinical reviewers gave their time free of charge.
Competing interests
None declared.
Acknowledgements
We would like to thank service users and staff of the South-West region of England for their help. The HES data team, Shane Coe, Paul Noonan (New Devon CCG), Neil Greening (Kernow CCG), Julia Thomas (Musgrove Park Hospital), Denise Walker (South Devon Healthcare) and Asha Sahni (Bristol Vascular Centre) provided amputation data. Thanks also to Rosamund Paisey for preparation of the manuscript, Christopher Paisey and Paul Hewson for statistical advice and Melvin Cowie for graphic design. The Torbay and South Devon foot service is led by Ruth Gornall, Robert McCarthy, Ian Jakin, James Davis and Gill Spyer.