Multimodal neurophysiologic and neuroanatomic assessment of brain connectivity in pediatric stroke
C8
S Nemanich, T Rich, B Mueller, A Opitz, B Gillick
University of Minnesota, Minneapolis, MN, USA
Background and Objective(s): Variability in motor function, underlying neuroanatomy, and neurophysiologic patterns among children with unilateral cerebral palsy (UCP) is high and may contribute to suboptimal outcomes following rehabilitation interventions. Here, we present a comprehensive characterization of brain structure and function before and after a combined neuromodulatory and rehabilitation intervention using novel multi-modal tools and assessments.
Study Design: Case-report, intervention study.
Study Participants & Setting: Case description of one female adolescent (age = 14 years) with UCP, who participated in an intervention consisting of 10 days of combined transcranial direct current stimulation (tDCS-20 minutes) and bimanual training (120 minutes). tDCS was applied at 1.5 mA intensity in a cathodal contralesional montage as an inhibitory neuromodulatory intervention.
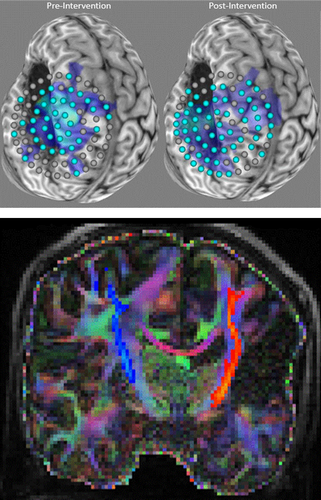
Materials/Methods: Assessments consisted of single-pulse transcranial magnetic stimulation (TMS), structural and diffusion-weighted magnetic resonance imaging (dMRI), and computational modeling of electric fields produced by neuromodulatory interventions. Using single-pulse TMS, cortical excitability was measured at pre-defined sites in each hemisphere to produce a motor map. TMS-derived cortical map volume (number of active sites) of motor-evoked responses was calculated. Probabilistic tractography was performed on dMRI data to estimate volume and mean diffusivity of the corticospinal tracts (CSTs) bilaterally (see Figure). An individualized model of head and brain anatomy was created using SimNI (Simulation of Non-invasive Brain Stimulation) based on individual neuroanatomy obtained from MRI. Electric fields were computed using the finite element method for the tDCS electrode montage used in the study.
Results: Lesioned hemisphere map volume increased by 46% (Pre-Test=39 sites, Post-Test=57 sites), and non-lesioned hemisphere map volume decreased by 19% (Pre-Test=16 sites, Post-Test=13 sites). This demonstrates a potential expansion of the motor representation in the lesioned hemisphere (see Figure). The observed asymmetry in CST volume was measured by dMRI (lesioned CST volume = 3.26 x 103 mm3, non-lesioned CST volume = 5.31 x 103 mm3). Mean diffusivity was greater in the lesioned CST (6.74 x 10−4 mm2/s) compared to the non-lesioned hemisphere (6.33 x 10−4 mm2/s), indicating a difference in white matter microstructure for the lesioned CST. Computational modeling of tDCS in the non-lesioned hemisphere revealed similar patterns to an individual without a brain lesion, wherein the peak electric field is located between each electrode.
Conclusions/Significance: Non-invasive assessments of the brain can reveal the neurophysiologic and neuroanatomic substrates that relate to behavioral changes after clinical interventions, and may predict who optimal responders to neuromodulation. Using a multi-modal approach with novel technology will advance our understanding of combined neuromodulation and neurorehabilitation allowing for targeted and individualized assessment and treatment.