Cerebral sinovenous thrombosis associated with head/neck infection in children: Clues for improved management
Abstract
Aim
To compare paediatric patients with cerebral sinovenous thrombosis (CSVT) with and without head/neck infection to improve management of the condition.
Method
We conducted a bicentric retrospective study of consecutive children (neonates excluded) with radiologically confirmed CSVT, comparing children with a concurrent head/neck infection and children with other causes.
Results
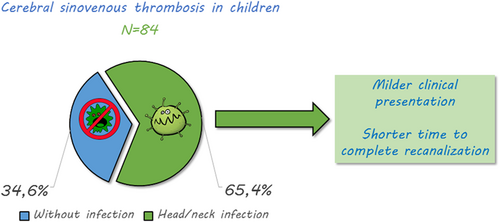
A total of 84 consecutive patients (46 males and 38 females) with a median age of 4 years 6 months (range 3 months–17 years 5 months) were included. Associated head/neck infection was identified in 65.4% of cases and represented the main identified CSVT aetiology. Children in the head/neck infection group displayed a milder clinical presentation and less extensive CSVT. Median time to complete recanalization was significantly shorter in this group (89 days [interquartile range 35–101] vs 112.5 days [interquartile range 83–177], p = 0.005). These findings were even more pronounced in the subgroup of patients with otogenic infection and no neurological sign.
Interpretation
As CSVT in the setting of an otogenic infection and no neurological sign seems to represent a milder condition with a shorter course, these results suggest adapting current recommendations: consider earlier control imaging in paediatric otogenic CSVT, and shorter anticoagulant treatment if recanalization is obtained.
What this paper adds
- Children with cerebral sinovenous thrombosis related to head/neck infections have a milder clinical presentation.
- They also have a shorter recanalization time, especially if there is otogenic infection without neurological symptoms.
What this paper adds
Abbreviations
-
- CSVT
-
- cerebral sinovenous thrombosis
-
- INF–
-
- no head/neck infection
-
- INF+
-
- head/neck infection
Cerebral sinovenous thrombosis (CSVT) occurrence is rare in children, with an incidence of about 0.67 cases per 100 000 children per year. This is probably underestimated as diagnosis is often delayed or missed.1, 2 It is a potentially severe condition, as children with CSVT are at risk for complications in the acute phase, such as intracranial hypertension, seizures, ischemic and/or haemorrhagic venous stroke, and for long-term sequelae, such as visual impairment, and motor or cognitive disabilities.1 Despite recent advances, diagnostic and therapeutic strategies for CSVT in children still suffer from lack of evidence, and consequent heterogeneity.1-3 Paediatric management recommendations are mostly adapted from adult literature.3, 4 Treatment in adults relies on anticoagulation therapy, initially with unfractionated heparin or low-molecular-weight heparin, followed by vitamin K antagonists or direct oral anticoagulants, regardless of the presence of intracranial haemorrhage if secondary to the thrombosis.2 Therapeutic studies are lacking in paediatric CSVT, especially randomized controlled trials. Despite concerns about age-related differences in the coagulation and neurological systems, a consensus has formed in favour of anticoagulation therapy in older children (i.e. excluding neonates) with CSVT.3, 5 A 3- to 6-month treatment has been proposed as the standard duration in most studies,3 and may be adapted to each situation and risk factor. While CSVT symptoms are quite similar in children and adults,6 the clinical context in which they appear may be different. Infection-related CSVT, mainly in the head and neck (ear, sinus, mouth, face, and neck), explains only 8.2% of adult cases, while it is much more common in paediatric cases (23%–49%).1, 2, 7-9 Although data from a few studies suggest a ‘less severe’ condition, with a lower risk of spontaneous recurrence,3, 10, 11 paediatric CSVT occurring in an infectious setting has not been compared to CSVT occurring in other settings. The present study focused on a comparison between paediatric patients with CSVT with and without head/neck infection to identify potential adaptations of management between groups.
METHOD
Patients
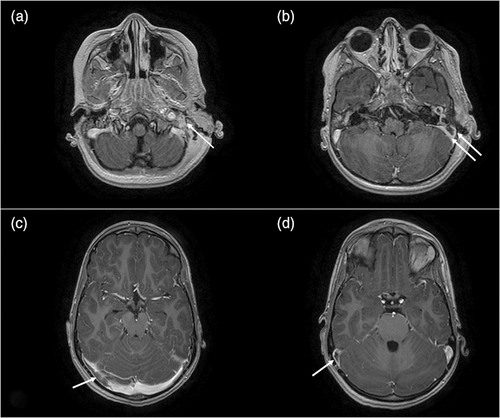
We conducted a bicentric retrospective study of consecutive paediatric patients with CSVT in two academic centres. Newly diagnosed CSVT cases aged from 1 month to 18 years who were admitted to the Arnaud de Villeneuve University Regional Hospital (Centre A), Montpellier, France or the University Hospital Necker-Enfants Malades (Centre B), Paris, France, during a 11 year and 6 year 4 month inclusion period respectively, were identified from electronic health records using adequate International Classification of Diseases, 10th Revision diagnostic codes. Patients were eligible if they had a radiologically confirmed CSVT affecting at least one of the following vessels: transverse sinus, sigmoid sinus, internal jugular vein, superior sagittal sinus, inferior sagittal sinus, straight sinus, cavernous sinus, and/or petrosal sinus during the inclusion period. Patients with either isolated cortical vein thrombosis, isolated jugular vein thrombosis in the presence of a central line, or thrombosis in the presence of a cardiopulmonary bypass were excluded. Imaging data were reviewed by paediatric neuroradiologists (NL, DG). Patients were included in the head/neck infection (INF+) group if they presented a concurrent otogenic (mastoiditis, otitis media) or non-otogenic (sinusitis, cervical infection, meningitis, etc.) head/neck infection at the time of CSVT diagnosis; they were included in the no head/neck infection (INF–) group if otherwise. Clinical, biological, and radiological data at presentation, and long-term clinical and radiological follow-up data were obtained from medical records.
Acute phase
Sex, age, and clinical presentation were recorded. CSVT-related neurological signs at diagnosis were defined as the presence of seizures, decreased level of consciousness (defined as Glasgow Coma Scale <12), focal symptoms including cranial nerve abnormalities, or intracranial hypertension (defined as headache associated with vomiting, elevated cerebrospinal fluid pressure if measured during a lumbar puncture, papilledema on fundoscopy, and/or elevated intracranial pressure observed by invasive intracranial pressure monitoring). Focal neurological signs, coma, and acute seizures were considered as potential markers of a parenchymal brain lesion, whereas diplopia or acute strabismus with sixth cranial nerve palsy were considered as intracranial hypertension symptoms. Imaging procedures performed at the acute phase, including computerized tomography (CT), magnetic resonance imaging (MRI), computerized tomography venography, and magnetic resonance venography were analysed. Extensive CSVT was defined as a CSVT affecting more than one venous segment. Parenchymal brain lesions on CT or MRI were recorded, including abscess, infarction, haemorrhage, and white matter anomalies. Other concurrent acute (notably anaemia, dehydration, head trauma, systemic infection) or chronic (notably sickle cell disease, nephrotic syndrome, systemic inflammatory disorder, neoplasia) conditions which are known as potential CSVT risk factors were also noted. The use of anticoagulant or antithrombotic therapy, type of drug (aspirin, low-molecular-weight heparin, unfractionated heparin, vitamin K antagonists), and treatment duration were recorded.
Thrombophilia workup
Results from biological screening for prothrombotic risk factors performed in the acute phase (first week after diagnosis) were analysed. The following results were considered as prothrombotic risk factors (positive thrombophilia workup): protein C activity less than 50%, protein S activity less than 60%, antithrombin activity less than 75%, presence of the prothrombin G20210A mutation, presence of the Factor V R506Q mutation, presence of a homozygous methylene-tetrahydrofolate-reductase gene mutation (C677T or A1298C) or plasma homocysteine dosage greater than 15 μmol/L, or presence of antiphospholipid antibodies (lupus anticoagulant, anticardiolipin, anti-β2GP1).
Outcomes
Radiological outcome studied the delay from diagnosis to complete recanalization, defined as an uninterrupted flow signal with a residual luminal narrowing of less than 50% in the previously affected venous segment(s).12 Clinical outcome at last visit, including fatality, was evaluated using the modified Rankin Scale adjusted for children, retrospectively estimated through the patient's record data. Significant events during follow-up, such as symptomatic haemorrhage during anticoagulant treatment, occurrence of heparin-induced thrombocytopenia, CSVT relapse, or occurrence of another venous thrombotic event, were collected.
Analyses
Descriptive analyses were performed to study data distribution among the children in the INF+ and INF– groups. Comparison between the groups was performed using the Kruskal–Wallis test for continuous variables, and Fisher's exact test for categorical variables. A Kaplan–Meier analysis with a log-rank test was performed to compare recanalization rate over time between groups. A p-value of 0.05 or less was retained for significance. Statistical analyses were performed using the R software version 4.0.5 and the R Studio development interface version 1.3.1093 (R Foundation for Statistical Computing, Vienna, Austria).
Local institutional review boards (Comité de Protection des Personnes Ile-de-France & Occitanie) approved the study and waived patient consent for this retrospective analysis of anonymized data.
RESULTS
A total of 84 consecutive patients (36 patients in centre A, 48 in centre B) verified the inclusion criteria. There were 46 males and 38 females (sex ratio 1.2), with a median age of 4 years 6 months (range 3 months–17 years 5 months). Most patients (n = 80, 95.2%) had an identified aetiology of their CSVT episode. An associated head/neck infection was found in 65.4% of all cases (INF+: n = 55), a similar proportion in both centres (72.2% vs 60.4%, non-significant), and represented the main identified CSVT aetiology. Infections were mainly otogenic (oto-mastoiditis n = 36, isolated otitis media n = 1). Other infections were meningitis (n = 10), sinusitis (n = 5), cervical adenophlegmon or parapharyngeal abscess (n = 4), and facial cellulitis (n = 1). Only 53% of patients with mastoiditis had bacterial identification, the most frequent germ being fusobacterium. Potential risk factors for CSVT were identified in almost every patient without head/neck infection (n = 27/29): 44.8% had a chronic or subacute prothrombotic condition, 27.5% had loco-regional non-infectious conditions, and 20.6% had a transient or acquired prothrombotic risk factor. Chronic or subacute prothrombotic condition included nephrotic syndrome (n = 4), Behcet disease (n = 4), systemic vasculitis (n = 1), sickle cell disease (n = 2), lupus associated with antiphospholipid syndrome and nephrotic syndrome (n = 1), and lymphoblastic acute leukaemia with L-asparaginase treatment (n = 1). Loco-regional non-infectious conditions included central nervous system tumour (n = 2), head trauma (n = 4), cerebrovascular malformation (n = 1), and acute disseminated encephalomyelitis (n = 1). Transient or acquired prothrombotic risk factors were anaemia (n = 2; iron deficiency and inflammatory anaemia), dehydration (n = 2), disseminated intravascular coagulation related to sepsis (n = 1), and recently introduced combined oestrogen/progestin oral contraception (n = 1). Of note, one patient with mastoiditis who also had sickle cell anaemia and one patient with meningitis occurring after a traumatic skull fracture were classified in the INF+ group as the infection was considered as the final trigger for CSVT.
Comparison between the INF+ and INF– groups
The INF+ group were significantly younger (median age 3 years 8 months vs 10 years 7 months old, p < 0.001), and more frequently had fever at presentation (96.4% vs 10.3%, p < 0.001) than the INF– group (Table 1). Patients in the INF+ group displayed a milder clinical presentation (no CSVT-related neurological signs in 30.9% vs 6.9%, p = 0.014) than the INF– group. They also had less frequent symptoms of intracranial hypertension (21.8% vs 64.3%, p < 0.001), or associated intracranial haemorrhage (1.8% vs 24.1%, p = 0.002). Diagnostic CT venography was performed in 82% of patients, magnetic resonance venography in 40%, and both modalities in 27%. CSVT associated with head/neck infection was less frequently extensive (27.3% vs 65.5%, p = 0.001) (Table 2, Figure 1). No patient required endovascular intervention. Anticoagulation treatment was comparable in the acute phase, with 81 out of 84 patients treated by unfractionated heparin or low-molecular-weight heparin. Of note, 76% of the INF+ patients (data available only for centre B) had surgical intervention; anticoagulation treatment was started shortly after surgery in these cases. Bridging to vitamin K antagonists was less frequent in the INF+ group (32.7% vs 58.6%, p = 0.034). Median anticoagulation treatment duration tended to be shorter in the INF+ group (3 vs 4 months, p = 0.08, non-significant). Most patients had a thrombophilia biological screening at the acute phase (78% and 96% in the INF+ and INF– groups respectively, non-significant). This workup was less frequently positive in the INF+ group (32% vs 44%, non-significant). In seven patients from the INF+ group with a positive antiphospholipid antibody result, a control test was performed several months later, which showed normalization of this parameter in all patients.
| INF+ | INF– | p | |
|---|---|---|---|
| n | 55 | 29 | |
| Median age, years:months (IQR) | 3:8 (1:11–6:7) | 10:7 (6:4–14:2) | <0.001 |
| Males | 32 (58.2) | 14 (48.3) | 0.490 |
| Acute phase | |||
| Fever | 53 (96.4) | 3 (10.3) | <0.001 |
| Intracranial hypertension | 12 (21.8) | 18 (64.3) | <0.001 |
| CSVT-related neurological symptoms | 38 (69.1) | 27 (93.1) | 0.014 |
| Associated intracranial haemorrhage | 1 (1.8) | 7 (24.1) | 0.002 |
| Associated ischaemic lesion | 1 (1.8) | 2 (6.9) | 0.273 |
| Outcomes | |||
| Median follow-up, months (IQR) | 7 (6–24) | 30 (12–51.5) | 0.002 |
| Median time to complete recanalization, days (IQR) | 89 (35–101) | 112 (83–177) | 0.005 |
| Complete recanalization at 3 months | 29 (65.9) | 8 (36.4) | 0.035 |
| Complete recanalization at end of follow-up | 44 (86.3) | 21 (77.8) | 0.355 |
| Anticoagulant treatment | 52 (96.3) | 29 (100.0) | 0.540 |
| Median anticoagulant treatment duration, months (IQR) | 3 (3–4) | 4 (3–6) | 0.080 |
| mRS = 0 in survivors | 45/52 (86.5) | 15/26 (57.7) | 0.009 |
- Data are n (%) unless otherwise stated. Bold type indicates statistical significance. Abbreviations: IQR, interquartile range; mRS: modified Rankin Score.
| INF+ | INF– | p | |
|---|---|---|---|
| n | 55 | 29 | |
| Affected sinus | |||
| Superficial venous system CSVT | |||
| Transverse sinus | 37 (67.3) | 21 (75.0) | 0.614 |
| Sigmoid sinus | 8 (14.5) | 1 (3.6) | 0.261 |
| Internal jugular vein | 17 (30.9) | 9 (32.1) | 1.000 |
| Superior sagittal sinus | 7 (12.7) | 13 (46.4) | 0.001 |
| Deep venous system CSVT | |||
| Inferior sagittal sinus | 0 (0) | 0 (0) | - |
| Straight sinus | 0 (0) | 0 (0) | - |
| Cavernous sinus | 3 (5.5) | 0 (0) | 0.547 |
| Petrosal sinus | 0 (0) | 0 (0) | - |
| Extensive CSVT | |||
| CSVT affecting several venous segments | 15 (27.3) | 19 (65.5) | 0.001 |
- Data are n (%) unless otherwise stated. Bold type indicates statistical significance.
Outcomes
Two patients in the INF+ group died because of a bacterial meningitis complicated by massive intracranial hypertension. Median follow-up duration for survivors was 12 months. Median time to complete recanalization was significantly shorter in the INF+ group (89 days vs 112.5 days, p = 0.005). Taking into account censored patients and different follow-up durations, the difference in the time to complete recanalization remained significant (p = 0.031, Figure 2). The rate of complete recanalization was significantly higher in the INF+ group at 3 months (65.9% vs 36.4%, p = 0.035) but not significantly different at the end of follow-up (86.3% vs 77.8%, p = 0.35). No heparin-induced thrombocytopenia or any symptomatic haemorrhage during anticoagulant treatment was reported. Three patients in the INF– group experienced a CSVT relapse during follow-up; two had Behcet disease and one had no identified condition. Clinical outcome in survivors was significantly better in the INF+ group, with an excellent outcome (modified Rankin Scale = 0) at last visit in 86.5% versus 57.7% in the INF– group (p = 0.009).
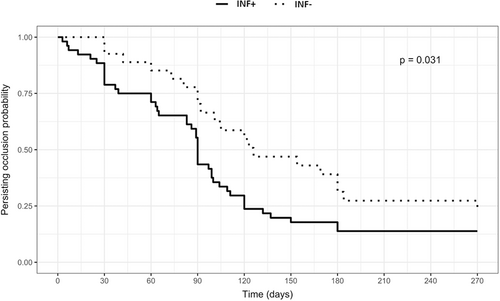
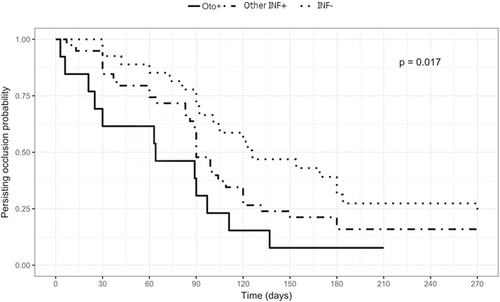
Patients with CSVT associated with otogenic infection and no neurological sign
Among the INF+ group, a subgroup of patients with otogenic infection (mastoiditis with or without otitis) without any neurological sign at the acute phase was specified. It represented 13 out of 36 otogenic infections. Children in this subgroup displayed the above-mentioned specific features in an even more pronounced way: they were significantly younger than the other patients with CSVT (median age 2 years 5 months vs 6 years 4 months, p = 0.003) and had an even shorter time to complete recanalization compared to the INF– group and the rest of the INF+ group (median 64 days vs 90 days, p = 0.026) (Figure 3).
DISCUSSION
This study compared children with CSVT with and without concurrent head/neck infection. The children in the INF– group resembled adults in terms of aetiology, clinical presentation, and evolution under anticoagulant treatment. Thus, current paediatric recommendations for CSVT, which are largely adapted from adult guidelines, seem appropriate for this subgroup. On the contrary, our study delineated a specific subpopulation of children with regional infection (INF+) with clinical, radiological, and outcomes specificities, for whom slightly different management strategies could be considered.
This study included one of the largest samples of patients with paediatric CSVT (n = 84) over a limited period in only two centres. Patients with concurrent head/neck infection outnumbered previous reports, which allowed a comprehensive study of this subpopulation and its comparison with paediatric CSVT from other causes. In our sample, most CSVTs (95.2%) were related to an underlying condition (previously diagnosed or revealed by the CSVT) or a precipitating event, as previously reported (95% in Dlamini et al.).13 Associated head/neck infection was the most frequent aetiology (65.5%), with a higher rate than reported in the years 2001 to 2005 (23%–49%).1, 6 Increased diagnosis of asymptomatic CSVT since the implementation of systematic CT imaging in mastoiditis workup14, 15 may account for this difference.
Children with CSVT associated with head/neck infection were younger and had milder clinical and radiological presentations than children with other causes. They also had better outcomes. In the literature, reported outcome in this setting is very heterogeneous, with variable measurement tools. A prevalence of 25% to 74% of long-term sequelae is reported,16 usually associated with a severe initial presentation and/or a persisting risk factor for recurrence.1 In our study, the prevalence of sequelae (modified Rankin Scale ≥1) was 23.1% in the whole sample, and significantly lower in the INF+ group, although two patients from this group had early fatal outcome related to severe bacterial meningitis. These results were more significant in the subgroup of children with CSVT associated with otogenic infection without neurological symptoms, in which all patients had a modified Rankin Scale score of 0 at the end of their follow-up.
Interestingly, children with CSVT associated with a head/neck infection displayed a significantly higher rate of venous recanalization at 3 months follow-up and a global quicker recanalization. In guidelines, assessing recanalization to support the decision of anticoagulant treatment weaning is often recommended at 3 months post-CSVT, and at 6 months if recanalization was not complete at the first control.3 In our study, CSVT management focused on these recommendations as most patients had control imaging at these predetermined delays. Actual recanalization delays may be shorter: in half of the patients with otogenic infection and no neurological symptom recanalization was complete 65 days after CSVT onset (Figure 2), that is, nearly 1 month before first recommended imaging control. One could suggest reimaging earlier in this setting, for example at 6 to 8 weeks from onset, and stopping anticoagulant treatment if recanalization was obtained and the initial infection cured. To our knowledge, some centres have already implemented this practical management, but no formal report or comparative study is available so far to estimate its efficiency (early patency diagnosis allowing shorter anticoagulation treatment vs no patency leading to supplemental reimaging). The role of anticoagulation treatment in the recanalization rate has been debated.3, 17 In this study most children in both groups had anticoagulation treatment – as recommended in Europe3 – suggesting that the observed difference in recanalization delay instead relates to the cause of CSVT. In our patients, anticoagulant therapy was well tolerated and no major treatment-related complication was reported, as suggested in previous paediatric reports.3
Concerning thrombophilia workup, we observed large variations in assessed parameters according to centres and over time. Globally, it was positive in 37% of patients, with a lower prevalence in the INF+ group. Previous studies reported positive thrombophilia screening in childhood CSVT in up to 60% of cases.16 It is currently unknown if these abnormalities are either causal, causal factors in association with other risk factors, or if they may be epiphenomena.16, 18 In mastoiditis complicated by CSVT, Coudert et al.19 reported a significant predominance of Fusobacterium necrophorum, found in 53.8% in this setting. Similarly, in our study, Fusobacterium necrophorum was the most prevalent germ, found in 57% of patients with an identified germ. Indeed, Fusobacterium necrophorum is known to particularly induce an inflammatory state, which becomes a prothrombotic state.20, 21 In our study, a late thrombophilia workup in a subgroup of patients with mastoiditis and positive initial workup showed the normalization of antiphospholipid antibody dosage after the infection episode, pointing to a risk of false-positive results at the acute phase of an infection. These findings suggest that the need for prolonged treatment may be infrequent in CSVT associated with head/neck infection and that thrombophilia workup could be delayed to 1 to 3 months after CSVT onset to avoid false-positives related to the acute inflammatory phase.
As mentioned above, specificities of children with CSVT and concurrent head/neck infection were even more pronounced in the subgroup of children with otogenic infection without neurological symptoms. As the number of patients in this subgroup was quite small (n = 13), we could not carry out further statistical analyses, but these results were consistent with a previous reported study on otogenic paediatric CSVT.10 These findings support the suggestion to adapt current recommendations concerning CSVT management in children, with earlier control imaging and delayed thrombophilia workup.
The major limitation of our study is its retrospective nature, with associated intrinsic biases. Participating centres were academic tertiary centres with highly specialized paediatric departments, including paediatric ear nose and throat and paediatric neurosurgery departments, which may have modified the repartition of CSVT causes. To evaluate outcomes, limited available data precluded the use of the dedicated Pediatric Stroke Outcome Measure scale, and we used the modified Rankin Scale adjusted for children, although it is less precise in this setting. Another limitation is related to anticoagulant treatment. In this sample, nearly all patients were treated. The above-mentioned suggestions for adapted management of CVST with regional infection are thus supported by data from treated patients only. This study does not address the issue of the anticoagulant treatment indication in paediatric otogenic CSVT, which is debated in the literature. Guidelines usually recommend anticoagulant treatment for non-neonatal paediatric CSVT,3, 16, 22 with a suggested individualized approach for some circumstances, including otogenic infection.16 Some authors suggest that adequate infection treatment (associating antibiotics and local surgery) may be sufficient,17, 23 whereas others suggest that anticoagulant treatment may prevent CSVT extension during the inflammatory prothrombotic acute phase. The tolerance of anticoagulant treatments in children is satisfactory in this setting, including for recent drugs.22, 24 But compliance may be difficult to obtain in case of repeated injections (low-molecular-weight heparin) or lab tests (vitamin K antagonists). Thus, alleviation of anticoagulant treatment burden, either by modifying galenic forms or by reducing treatment duration, remains an important goal to improve the patients' quality of life. Additional studies are encouraged to verify the relevance of the suggested measures.
CONCLUSION
The subgroup of children with CSVT associated with head/neck infection are younger patients, they have milder clinical presentations, a quicker venous recanalization, and better outcomes, especially in cases with otogenic infections. These findings suggest adapting current recommendations concerning CSVT management in children in the setting of otogenic infection without neurological symptoms. Under anticoagulant treatment, imaging control is suggested earlier than the usual 3 months delay, allowing anticoagulant treatment weaning if recanalization is obtained and the initial infection cured. Thrombophilia workup could be delayed after the CSVT acute phase because of the initial rate of false-positive results in the inflammatory period. These measures could help alleviate the burden of CSVT and anticoagulant treatment in these young children.
ACKNOWLEDGMENTS
The authors have stated that they had no interests that might be perceived as posing a conflict or bias.
Open Research
DATA AVAILABILITY STATEMENT
The authors have full access to all of the data, which will be made available to any researcher for purposes of reproducing the results.