Outcomes for children with acquired brain injury (ABI) admitted to acute neurorehabilitation
Abstract
Aim
To evaluate an innovative paediatric neurorehabilitation model in relation to improving quality of neurorehabilitation and reducing length of stay (LOS) for children with acquired brain injury.
Method
A process evaluation approach was conducted in line with Medical Research Council evaluation of complex interventions guidance. Analysis was conducted on routinely collected patient data from 2017 to 2018, including LOS and family feedback. Descriptive and inferential statistics were used for quantitative analysis and qualitative data was analysed thematically.
Results
Outcomes for 70 children (0–16y, median age 5y, IQR 1–11y, 46 males, 24 females) referred to the service indicated improved function and reduced complexity of need. The mean LOS was 10.6 days compared to baseline mean LOS of 41 days (2011–2012). High satisfaction from the families was recorded; however, ongoing needs and service gaps regarding long-term support were identified.
Interpretation
This service model is effective in delivering quality paediatric neurorehabilitation, demonstrating a sustained impact on LOS, and positive patient outcome data and family feedback for this group of patients.
What this paper adds
- Investment in early intensive neurorehabilitation and supported discharge impacts length of stay (LOS) for children with acquired brain injury.
- Early intensive neurorehabilitation and supported discharge is effective.
- This is demonstrated by a sustained reduction in LOS, positive patient outcomes, and family feedback.
What this paper adds
- Investment in early intensive neurorehabilitation and supported discharge impacts length of stay (LOS) for children with acquired brain injury.
- Early intensive neurorehabilitation and supported discharge is effective.
- This is demonstrated by a sustained reduction in LOS, positive patient outcomes, and family feedback.
This article is commented on by Lam Wai Shun, Swaine, and Bottari on page 764 of this issue.
Abbreviations
-
- ABI
-
- Acquired brain injury
-
- KOSCHI
-
- King's Outcome Scale of Childhood Head Injury
-
- LOS
-
- Length of stay
-
- RCS-E
-
- Rehabilitation Complexity Scale – Extended
-
- WTE
-
- Whole time equivalent
Each year in the UK, at least 40 000 children sustain an injury to their central nervous system such as an acquired brain injury (ABI) or spinal cord injury.1 Such injuries result from traumatic (fall, road traffic collision) or non-traumatic causes (stroke, infection, tumour).2 Internationally, traumatic brain injury is the leading cause of death and disability in children.3 Many of those who sustain more severe injuries experience significant neurological impairment and require neurorehabilitation which begins during the inpatient stay alongside post-acute care.1, 3 Since NHS England published service specifications for paediatric neurorehabilitation in 2013 and rehabilitation commissioning guidelines in 2016, there has been a national drive towards the provision of effective and equitable rehabilitation for children, led by the Paediatric Neuroscience Clinical Reference Group. Rehabilitation has been shown to improve outcomes and quality of life, with the potential to reduce health inequalities and make significant cost savings across the health and care system by unlocking children’s social, educational, and economic potential.4 Although there is evidence of the economic benefits of adult rehabilitation, more work is needed to fully explore this in the paediatric context.4
There is wide variation in paediatric neurorehabilitation service provision nationally, and literature investigating the complex process of paediatric neurorehabilitation is lacking, with little known about the ‘active’ ingredients involved, or the ‘dose’ required.3, 5 Identification of influential factors for recovery and their importance is limited, impacting on the development of an evidence base for interventions.6
The aim of this study was to comprehensively evaluate the impact of an innovative paediatric neurorehabilitation service. The objectives were: to establish if service improves patient outcomes and reduces length of stay (LOS) and to identify areas for service development. In doing so, this study will contribute to the evidence base for service models of paediatric neurorehabilitation.
METHOD
Design
A retrospective, descriptive, longitudinal, observational study using process evaluation was undertaken to understand and assess the quality of implementation, and the mechanisms of impact and contextual factors of this complex intervention.7, 8 As this was a service evaluation, full ethical approval was not required, but it was registered with the local clinical governance department (Project Number: 18-175C).
Service evaluation model
This paper represents the activity for the sole regional paediatric neuroscience centre in one health region in England, total population about 4 million (800 000 <18y). There are 17 such centres situated across the nine health regions in England. After an initial pump-priming pilot of the service model commencing October 2014, ongoing NHS England specialist services funding was agreed in March 2016.9 The service delivers early intensive neurorehabilitation and early supported discharge to all children (0–18y) admitted to a specialist regional centre with an ABI or other neurological injury (including spinal cord injury). The team consists of a 0.2 whole time equivalent (WTE) consultant neurodisability paediatrician, 1.5 WTE physiotherapists, 1.5 WTE occupational therapists, 0.5 WTE speech and language therapist, 0.4 WTE clinical psychologist, and 1 WTE therapy support worker.
The service evaluation model consisted of the following components: a detailed description of the intervention (service) and implementation; analysis of mechanisms of impact and contextual factors (routinely collected data and family feedback); evaluation of the effectiveness of the service from analysis of the data and identification of areas for service improvement.
Participants and setting
Routinely collected service data from 70 children referred to the service with ABI or central nervous system injury from April 2017 to March 2018 were included. Family, team member, and stakeholder feedback was collected via questionnaires and forums.
Process and reach
Children with a recognized ABI or central nervous system injury admitted to the hospital are referred to the service. Each child is assessed and assigned to one of five patient pathways according to neurological deficits. Rehabilitation as per pathway plan commences as soon as the child is medically stable (i.e. stable observations, including vital signs) and well enough to participate (Fig. 1).
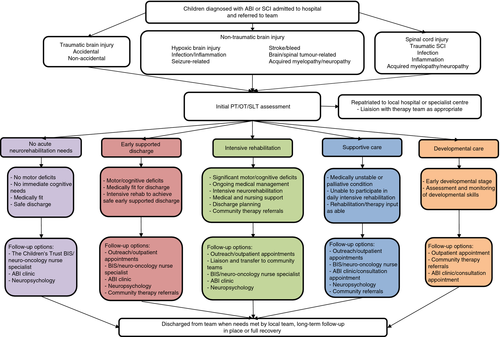
Rehabilitation is delivered through a combination of single profession and multi-professional sessions, as required. Intensive therapy is delivered daily (weekdays) during the inpatient stay (1–3h/d, more than one profession, depending on patients’ needs). After discharge from hospital, the team provide outreach therapy through a combination of outpatient appointments, and home and school visits, determined by need and geographical location (1–3 times a week). This continues until either the child has fully recovered or their care is transferred to the local community team. The team meets weekly, to discuss all children currently under the care of the service and to set goals. Attendance at neurology, neurosurgical, and neuro-oncology team meetings ensures collaboration with the wider multidisciplinary team. Multi-agency discharge planning meetings are arranged as required and continue at regular intervals during rehabilitation, and post-discharge where there are ongoing service provision needs.
Outcome measures
Patient demographics, ethnicity, geographical location, admission and discharge information, and LOS data are collected routinely for every child referred to the service. The service also routinely collects standardized outcome measures which are nationally recognized to evaluate outcome, patient complexity, and service satisfaction (Table 1).10-12
|
King's Outcome Scale of Childhood Head Injury (KOSCHI) Specific paediatric validated adaptation of the adult Glasgow Outcome Scale, providing a simple descriptor of outcome post-brain injury.10 Collected for all patients. |
|
Rehabilitation Complexity Scale – Extended (RCS-E) Patient complexity measure developed to allow coding of complexity to inform tariff banding in adult neurological rehabilitation services.11 Collected for patients on intensive rehabilitation pathway. |
|
Experience of Service Questionnaire (ESQ) Developed by the then Commission for Health Improvement (now the Health Care Commission) as a means of understanding family’s experiences of services through children (9–11y, 12–18y) and parent reports.12 The ESQ has been used by the team since 2014 to gather service user feedback data for audit purposes. Sent out by post after discharge home or from outreach service. Collected for patients on early supported discharge and intensive rehabilitation pathways. |
In addition, children seen by the team during 2017 and 2018, and their families, were invited to a family feedback forum through postal, telephone, or face-to-face invites. They were asked open-ended questions – ‘what went well’ and ‘even better if’ – to promote discussion.
Data analysis
Data for 2017 and 2018 were extracted, and checked for accuracy and completeness using hospital systems. There was no missing data; all children referred to the team were included, including those who died during admission. Data for 2017 to 2018 were also compared with previous years’ LOS data from service audits and baseline data collected in 2011 and 2012 during the business case development. All analyses were performed in Stata 15.0 (StataCorp 2015, College Station, TX, USA). Descriptive statistics were used to define the cohort in relation to demographics, including sex, age, ethnicity, region admitted from, and patient pathway. The geometric mean was used to model average LOS with more precision than the median for right-skewed count data, which facilitated analysis of the geometric mean ratio relative to a reference group. LOS in each year since service introduction were compared to LOS in 2011 and 2012, the pre-service period. The geometric mean LOS for 2017 to 2018 specifically was then assessed according to demographics, including patient pathway and diagnosis, with the geometric mean ratio. The geometric mean LOS values are plotted with 95% confidence intervals (CIs) providing the expected limits of the mean within the population. Comparisons were made between admission and discharge outcome measure scores ( King's Outcome Scale of Childhood Head Injury [KOSCHI], Rehabilitation Complexity Scale – Extended [RCS-E]). Wilcoxon signed-rank tests were used to assess differences in matched observations, median values are presented with interquartile range (IQR). A significance threshold of p<0.05 was applied throughout.
Qualitative data collected through the feedback forum and questionnaire were analysed using Braun and Clarke’s reflexive thematic analysis to identify key themes.13
RESULTS
Demographics
A total of 70 children were referred to the service between April 2017 and March 2018. The majority were male and 28 out of 70 (40%) were under 4 years of age. Twenty-six (37%) children had suffered non-traumatic brain injuries. There was a broad distribution across the region (Table 2). Half were admitted to the tertiary unit having been transferred from another regional hospital to access specialist services. From a total of 70 children, three (4%) died as inpatients because of the severity of their injuries; 60 out of 70 (86%) children required some therapy input, with 7 out of 70 (10%) having no acute rehabilitation needs. From those requiring therapy, 26 (37%) received intensive inpatient rehabilitation whilst an early supported discharge (with rehabilitation provided at home or as an outpatient) was provided for 14 out of 70 (20%). A further 14 out of 70 (20%) received supportive rehabilitation care whilst receiving oncological or other acute medical treatment and 6 out of 70 (9%) were young infants who received therapy to support their development.
| Demographic | n (%) | |
|---|---|---|
| Sex | Male | 46 (66) |
| Female | 24 (34) | |
| Age (y) | <4 | 28 (40) |
| 4–8 | 14 (20) | |
| 9–12 | 13 (19) | |
| >12 | 15 (21) | |
| Ethnicity | White | 54 (77) |
| Asian | 13 (19) | |
| Black | 2 (3) | |
| Not stated | 1 (1) | |
| Geographic location (home)a | County A | 22 (31) |
| County B | 19 (27) | |
| County C | 12 (17) | |
| County D | 9 (13) | |
| County E | 3 (4) | |
| Out of area | 5 (7) | |
| Diagnosis | ||
| Trauma | 22 (31) | |
| Brain tumour | 19 (27) | |
| Non-traumatic | Total | 26 (37) |
| Infection | 11 (15) | |
| Stroke | 8 (11) | |
| Hypoxia | 5 (7) | |
| Neuropathy | 1 (1) | |
| Myelopathy | 1 (1) | |
| Spinal cord injury/other | 3 (4) | |
| Admitted from | ||
| District general hospital | 35 (50) | |
| Emergency department | 25 (36) | |
| Elective admissions | 8 (11) | |
| Out of area admissions | 2 (3) | |
| Ward admitted to | ||
| Paediatric neurosciences ward | 41 (58) | |
| Paediatric critical care unit | 25 (36) | |
| Other wards | 4 (6) | |
| Patient pathway | ||
| No acute needs | 7 (10) | |
| Early supported discharge | 14 (20) | |
| Intensive rehabilitation | 26 (37) | |
| Supportive care | 14 (20) | |
| Developmental care | 6 (9) | |
| Died | 3 (4) | |
| Discharge destination (67 survivors) | ||
| Home (or temporary residence (e.g. foster care)) | 53 (79) | |
| Other out of area specialist hospital | 3 (5) | |
| Regional district general hospital | 11 (16) | |
| Post-discharge therapy (67 survivors) | ||
| Outreach service (home visits/outpatients) | 14 (21) | |
| Referred for local follow-up | 14 (21) | |
| None required | 25 (37) | |
| Inpatient transfer | 14 (21) | |
- a Geographical locations have been anonymized as County A, B, C, D, E.
Of the 67 survivors, 14 (21%) children were transferred to other hospitals for ongoing specialist care or repatriated to their local hospital, with the majority being discharged directly home (53/67; 79%). For those not repatriated, after discharge home, 14 out of 67 (21%) children received outreach from the team through home visits and outpatient appointments, before being transferred to local therapy teams or discharged; 14 out of 67 (21%) were referred directly to local therapy services for follow-up; and 25 out of 67 (37%) required no ongoing therapy.
Long-term follow-up was ensured for all children with the brain injury specialist (funded by The Children's Trust) and either the service’s consultant, local paediatrician, or other consultant and neuropsychologist, where required.
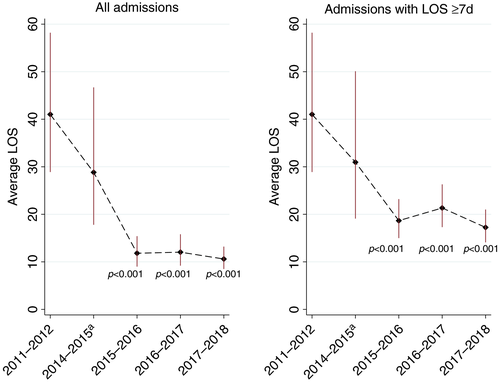
Analysis of LOS
The LOS for 2017 to 2018 was compared to 2011 to 2012 baseline data and the previous years’ data (2014–2017) (Fig. 2; Tables S1 and S2, online supporting information). In the cohort of 67 surviving individuals, between 2017 and 2018, mean LOS was 10.6 days (95% CI 8.5–13.2d). This was statistically lower than baseline data from 2011 to 2012 (41d, p<0.001), before the service was launched (October 2014). In previous years, local audits focussed on children who stayed 7 days or more (representing a higher complexity of rehabilitation need). Comparing the 2017 to 2018 data to previous years for those children who had a LOS equal to or greater than 7 days, the mean stay was 17.2 days (95% CI 14.1–21.0d), which was also statistically lower than baseline data (p<0.001). No overall associations were found within the 2017 to 2018 LOS data according to demographics of age, ethnicity, sex, region admitted from, admission type, or speciality.
Analysis of mechanisms of impact and contextual factors
KOSCHI
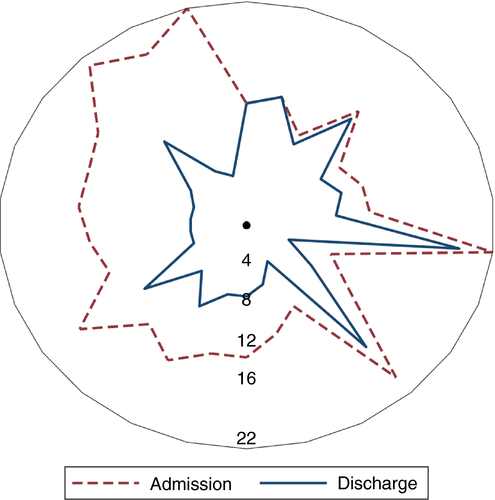
Where a score of 5B reflects full recovery, median score on admission for the 70 children included was 4A (IQR 3A–4B) and on discharge was 4B (IQR 4A–5A) (p<0.001); 26 children had the same KOSCHI score at admission and discharge, whilst 41 (59%) had an improvement in score. For children on the early supported discharge and intensive rehabilitation pathways who received higher levels of rehabilitation because of higher level needs (n=40), the median KOSCHI discharge score of 4B (IQR 4A–4B) was statistically higher than median admission score of 3B (IQR 3A–4A) (p<0.001). Eight (20%) children stayed the same, whilst 32 (80%) improved (Fig. 3).
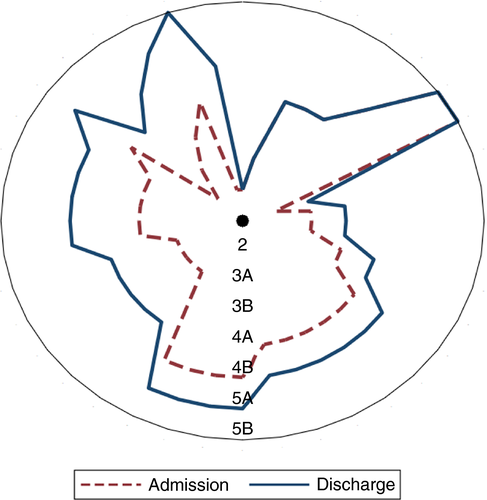
RCS-E
RCS-E scores for admission and discharge for the 26 children on the intensive inpatient rehabilitation pathway were analysed. Where a score of 0 indicates no rehabilitation required, median RCS-E scores at discharge (7, IQR 5–11) were statistically lower than admission scores (13.5, IQR 11–16) (p<0.001). Scores improved (reduced) in 24 out of 26 children and remained the same in 2 out of 26 children (Fig. 4).
Experience of Service Questionnaire
The service has gained consistently good feedback from parents/carers and children since it was launched. Postal questionnaires are routinely sent to families whose children had received intensive inpatient rehabilitation or early supported discharge. Between 2014 and 2018, 46% (57/125) of families responded, with over 80% of parents being highly satisfied with the overall service and care they received.
Patient and public involvement
A feedback forum was held with 11 participants attending: four children, five mothers, and two grandparents. From this data, three main themes were identified relating to support, participation, and information.
Support
Families were enthusiastic about the level and quality of rehabilitation and support they received whilst in hospital and during discharge home. Whilst families talked of the positives of being at home and ‘home being therapy’, parents also reported that more long-term support was required as the impact of the child’s ABI on the whole family was ‘exhausting’ and ‘never-ending’. Parents reported needing to ‘project manage’ day-to-day life, cope with ‘information overload’, and try to understand how the different health, social care, and education systems work. Families felt they lacked a long-term key point of contact (key worker) for help and support, particularly regarding accessing the support their child needed from all the services – ‘It's exhausting fighting for everything – ones who get are the ones who shout the loudest’.
Families felt that they needed long-term support from the whole specialist team. Psychological support was a particular gap. Whilst some families received support in their local area, most did not. The limited provision of psychology within the regional service (0.4 WTE) also meant that the families could not access the support for their child and wider family they felt they required. Parents and children also stated the need for peer support and the desire to be able to link up with other families through social media and in person.
Participation
Some children had experienced a slow return to school and parents/carers were concerned about the impact this had on them, particularly socially. Families also reported needing more support to enable return to other activities, especially sport. Two families had engaged private physiotherapists to enable this.
Information
Parents felt they needed to be provided with factual information (magnetic resonance imaging, reports, etc.) for a long time after the injury in order to access services their child needed. Children wanted detailed information in order to ‘fill in the gaps’ in their memory from the stages of accident/illness/recovery they could not remember. Some parents reported finding this hard to do and ‘not wanting to go back there’. The families discussed the importance of creating diaries and taking photographs, but also recognized the need for support from the team to do so. This was found to be particularly important in the early days after the injury, when their child was acutely unwell, but parents found it hard to take photographs and document events.
DISCUSSION
The aim of this study was to comprehensively evaluate and describe the ongoing impact of an innovative regional paediatric neurorehabilitation service on children with central nervous system injuries, their families, and other stakeholders. The study evaluated demographic information of the 2017 to 2018 cohort, their rehabilitation, and early outcomes. It also evaluated the impact the service has had on LOS since it was launched in 2014. The evidence provided by this study demonstrates that this level of early intervention is having lasting benefits in unselected cohorts of children. Specifically, evaluation of patient outcomes between admission and discharge, parent/patient satisfaction data, and the qualitative feedback demonstrate favourable outcomes.
The demographics of the 2017 to 2018 cohort are statistically similar with previous years’ data as previously described in Keetley et al.9 and other similar studies.3, 14 There is a wide geographical spread demonstrating the regional reach of this tertiary-level service, as stipulated in the NHS England Service Specifications for Paediatric Neurorehabilitation.1 With non-traumatic ABIs separated out into different aetiologies, trauma is the leading cause of ABI in this cohort; again, consistent with the wider literature where traumatic brain injury is the primary cause of morbidity and mortality in children nationally and internationally.2, 3
The patient outcome measures used by the service appear effective in measuring improvement in this population despite the relatively small numbers. Both the KOSCHI and RCS-E have been shown to be easy to use and can capture the degree of complexity and change in this patient group. The evaluation recommends the continued use of both measures; with the KOSCHI for all patients at admission, discharge home, and discharge from outreach to capture ongoing change post-discharge home, and the RCS-E for all patients on the early supported discharge, intensive rehabilitation, and supportive care pathways. Whilst the service has trialled various functional measures (e.g. Functional Independence Measure and Functional Assessment Measure), there is no one measure currently available to the team that is valid for all age groups. In the UK there are ongoing discussions regarding a core outcome measure set to capture function in children with ABI, with work needed to develop measures of rehabilitation in this population.15
The Experience of Service Questionnaire provides useful service user feedback through the scoring and free-text sections for audit purposes. Collecting service user feedback continues to be central to the person-centred care ethos of the service and ensuring children and families feel listened to and well supported, as detailed in the NHS Long Term Plan.16
Comparing the LOS from 2017 to 2018 to before the service was launched ( 2011–2012) and previous years’ data, it is evident that the service continues to have a sustained effect in reducing the LOS of this patient group, despite an increase in the number referred to the team. Patient and public involvement feedback and evidence of the benefits of services in the adult population with stroke9, 17 emphasize the positive impact of an earlier supported discharge. Such advantages must, however, be balanced with ensuring ongoing outreach rehabilitation and support is in place, delivered by either specialist or community services, before discharge.
Ongoing long-term needs identified through the patient and public involvement feedback were generally in line with those identified by the staff and service steering group and the wider literature, despite the low response rate.18 Several recommendations were identified to improve the patient pathway and support children and their families post-discharge and in the longer term. These included expansion of the outreach service and continuation of the key worker role to offer more support post-discharge, including increased psychological support, and development of a long-term multidisciplinary follow-up clinic to provide comprehensive longer-term care.
This real-life, pragmatic evaluation of a complex intervention has provided evidence of patient benefit and a reduced LOS with inherent acute cost savings in an unselected cohort of children with ABI and spinal cord injury. However, the study did have limitations. As it was not a randomized controlled trial, other time-dependent trends may have had a positive effect that we were unaware of a cluster randomized controlled trial of standard care compared with this model would be ideal, but may not be feasible because of service variation at different centres. A second limitation concerns outcome measures. First, there is currently no nationally agreed outcome measure set for this population. The results of this study are limited to the three measures used by the service which currently do not include comprehensive functional and quality of life outcomes. It is important to note that, although every effort was made to ensure data completeness and minimize bias, the clinical measures were completed by the clinical team. Future studies should include interrater reliability assessment. Furthermore, caution should be taken in interpreting the service user feedback because of the risk of bias.
Evidence for paediatric neurorehabilitation is sparse and there is a need for clinically relevant high-quality research to support service recommendations for commissioners and providers.19 This process evaluation has assessed this service model in terms of its implementation, mechanisms of impact, and contextual factors, providing evidence of its effectiveness whilst also identifying areas for further development. Further research is required to conduct an economic evaluation of this model in relation to health care utilization and cost-benefit analysis, and compare this model to others. Detailed investigation of the longer-term needs of this population is also indicated to ensure services can develop to meet the needs of children and their families after discharge from hospital.
Acknowledgements
This project was funded by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care East Midlands, now recommissioned as the NIHR Applied Research Collaboration East Midlands (ARCEM). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
We would like to thank all the families and team involved with this service for their assistance with this study.
Dr Joseph C Manning is current recipient of a National Institute for Health Research/Health Education England ICA Clinical Lectureship.
Open Research
DATA AVAILABILITY STATEMENT
Data available on request due to privacy/ethical restrictions