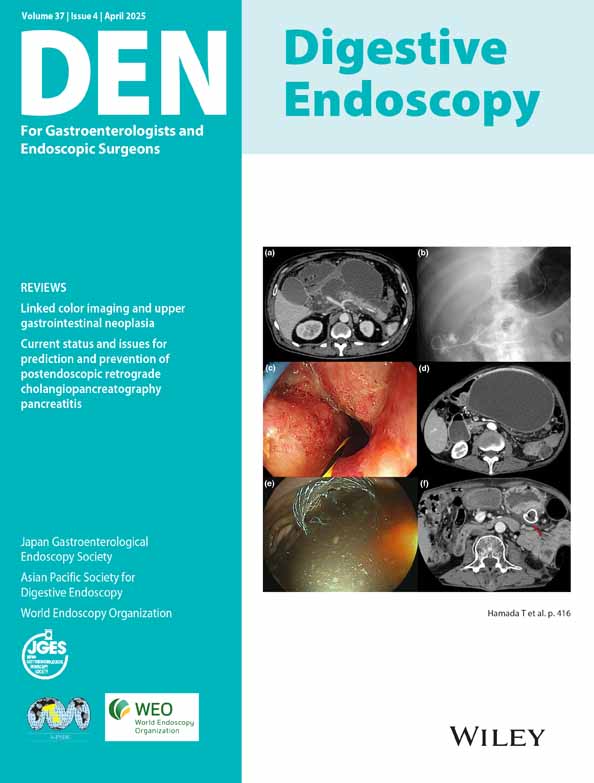
Endoscopic transpapillary gallbladder drainage using a novel cholangioscope
Abstract
Watch a video of this article.
BRIEF EXPLANATION
A 73-year-old man, recently treated with stent-graft insertion for an abdominal aortic aneurysm, developed acute cholecystitis from gallstones in a preshock state (Fig. 1a). Cholecystectomy was deemed high risk, and percutaneous transhepatic gallbladder drainage (PTGBD) was planned but considered unsafe due to Chilaiditi syndrome. Therefore, endoscopic transpapillary gallbladder drainage (ETGBD) was conducted. However, the cystic duct could not be visualized on cholangiography despite meticulous guidewire exploration for ~10 min, failing to identify its bifurcation. We then attempted to locate the cystic duct using a novel cholangioscope with a cytology brush sheath, as previously reported for confirming residual bile duct stones.1 This method utilizes only the reusable complementary metal oxide semiconductor (CMOS) camera unit of an ultrathin cholangioscope (DRES Slim Scope; Japan Lifeline, priced at 300,000 yen for ~10 uses) which is passed through the brush lumen of a double-lumen bile duct cytology brush (CytoMaxII; Cook Japan, Tokyo, Japan) (Fig. 1b,c). By replacing the original sheath, which costs 39,000 yen, with the CytoMaxII priced at 12,000 yen, the cost of using the cholangioscope is reduced to 42,000 yen per procedure. Moreover, this method allows the sheath to function similarly to an endoscopic hood, enabling reliable exploration of the cystic duct bifurcation (Fig. 1d). With this method, it became possible to safely advance the guidewire into the gallbladder, ultimately allowing for the placement of an ETGBD tube (Fig. 1e, Video S1).
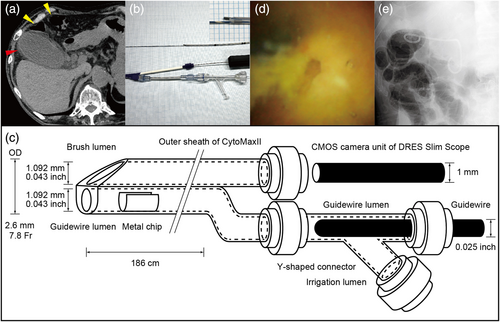
In cases where surgery or PTGBD is not feasible and ETGBD is necessary, inserting a guidewire into the cystic duct is essential but often challenging.2, 3 Using peroral cholangioscopy allows for safer and more reliable guidewire insertion compared to relying solely on X-ray images,4 yet cholangioscopes are expensive and less accessible. Our method balances cost and reliability in challenging ETGBD situations and also holds various other possibilities.
Authors declare no conflict of interest for this article.