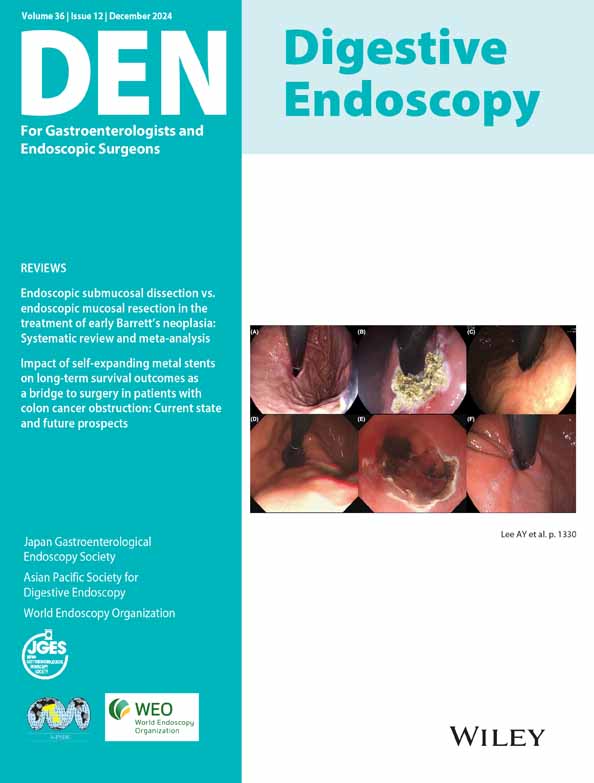
Modified gel immersion method during endoscopic ultrasonography and injection sclerotherapy for esophageal varices
Abstract
Watch a video of this article.
BRIEF EXPLANATION
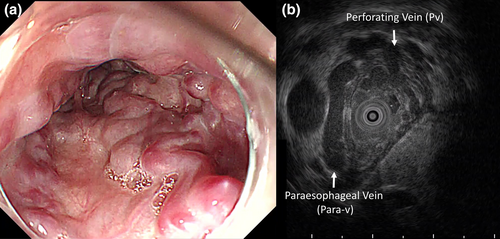
Ruptured esophageal varices (EVs) lead to life-threatening events. Endoscopic injection sclerotherapy (EIS) can help prevent bleeding. Endoscopic ultrasound (EUS) is essential for evaluating EV hemodynamics to ensure their effective management. The gel immersion method (GIM), which is crucial for accurate diagnosis and management, provides a clear and stable medium in the gastrointestinal system.1 Compared with traditional water immersion techniques, the GIM provides superior image quality and reduces the risk of aspiration and other complications.2 A 75-year-old Japanese woman presented with an EV with enlarged and red color signs at risk of bleeding (Fig. 1a). Two consecutive EUS and EIS procedures were performed using the modified GIM (mGIM-EUS/EIS). During esophagoduodenoscopy, after general evaluation of the EV and deaeration of the stomach, gel (Viscoclear; Otsuka Pharmaceutical Factory, Tokushima, Japan) was injected into the esophagus. The EV was identified and the esophageal wall vessels (perforating veins) were penetrated using a 20 MHz ultrasonic mini probe (Fig. 1b) before mGIM-EIS. This method enabled a detailed hemodynamic evaluation of EV, including the assessment of perforating veins, to help estimate the difficulty of EIS.2, 3 mGIM-EIS was conducted without interruption. Filling the esophagus with intermittent gel supplementation prevented visual defects due to bleeding and improved procedural safety (Fig. 2a). The gel facilitated precise needle placement, effective delivery, and visualization of sclerosant agents into the varices, using balloon deployment to reduce the risk of aspiration (Fig. 2b–d, Video S1).3 The gel was injected through the working channel during the procedure. The absence of air in the esophagus and stomach reduced the patient burden. The gel used can be securely held in the esophagus, enabling mGIM-EUS/EIS procedures to be performed continuously and without stress. This method minimizes the risk of aspiration and ensures accurate and safe management during mGIM-EIS. Therefore, mGIM-EUS/EIS is more effective and safer than previous methods.
Authors declare no conflict of interest for this article.