Two-devices-in-one-channel method for minor papilla cannulation
Abstract
Watch a video of this article.
BRIEF EXPLANATION
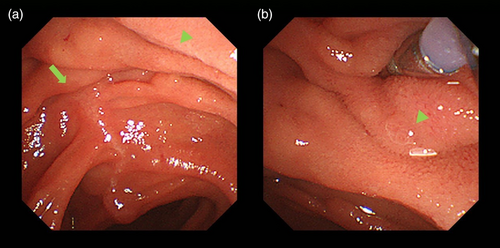
Minor papilla cannulation is performed in patients with pancreas divisum and acute recurrent pancreatitis1; however, it can be a technically challenging procedure.2 We demonstrated the two-devices-in-one-channel method for minor papilla cannulation. A 50-year-old man was admitted to our hospital for recurrent pancreatitis. Pancreas divisum was suspected to be the cause of the recurrent pancreatitis. Subsequently, the patient underwent endoscopic treatment, during which a duodenoscope (model TJF 290 V; Olympus, Tokyo, Japan) was advanced to the minor duodenal papilla. We initially attempted wire-guided cannulation; we were unsuccessful because of the small size of the minor papilla, its loose fixation, and susceptibility to respiratory variability (Fig. 1). Therefore, we attempted minor papilla cannulation using the two-devices-in-one-channel method (Video S1). A slim catheter (model PR-110Q; Olympus), loaded with a 0.025 inch guidewire (Radifocus; Terumo, Tokyo, Japan) and small biopsy forceps (Radial Jaw4P; Boston Scientific, Marlborough, MA, USA) were inserted into the same channel of the duodenoscope. The forceps were then used to grasp the anal side of the minor papilla and pull it towards the scope to retract the catheter tip into the minor papilla. Following this procedure, we fixed the minor papilla and aligned the catheter with the pancreatic duct axis. After successful cannulation, sphincterotomy was performed, followed by the placement of a 7F, 5 cm pancreatic stent (Advanix; Boston Scientific). During the wire-guided cannulation, the endoscopist pushed the cannula with force, which can cause the pancreatic duct axis to bend easily if the minor papilla is inadequately fixed. However, using the two-devices-in-one-channel method and pulling the minor papilla toward the scope can help adjust the axis of the catheter to the pancreatic duct as it straightens the bend in the pancreatic duct. This method is, therefore, an effective technique not only for biliary cannulation3, 4 but also for minor papilla cannulation.
Authors declare no conflict of interest for this article.