Warning from artificial intelligence against inaccurate polyp size estimation
Polyp size, as well as the histology of colorectal polyps, is an essential factor in appropriate management. Western guidelines have recommended surveillance intervals according to the size, number, and histology of polyps.1, 2 In particular, adenomas with a diameter ≥10 mm are defined as advanced adenomas, and a shorter surveillance interval is recommended for patients with those adenomas. In Japan, the Colonoscopy Screening and Surveillance Guidelines of the Japan Gastroenterological Endoscopy Society have also recommended surveillance after 1 year for cases with lesions ≥20 mm.3 In addition, an endoscopic therapeutic strategy for colorectal polyps has been proposed based on polyp size. In the guidelines published by the Japanese Society of Gastroenterology,4 colorectal polyp size was used as a reference to determine the policy for endoscopic resection or follow-up observation and selection of the appropriate resection method, including cold snare polypectomy. Inaccurate size assessment can lead to incorrect surveillance intervals and treatment selection for polyps. Thus, accurate estimation of polyp size, as well as histological prediction, is required for all colonoscopists.
However, how accurately do we usually diagnose polyp size? Most endoscopists would probably not answer the question, as they have few opportunities to confirm the accuracy of their own estimation. Analyses of estimated polyp size using a database, including the Japan Endoscopy Database, showed a preference of endoscopists for specific numbers, such as a terminal digit of 0 or 5, unlike the expected actual distribution of polyp size.5, 6 Endoscopists often pay little attention to polyp size estimation despite its clinical importance. Therefore, the inaccuracy of polyp size estimation should be recognized, since even experienced endoscopists have been reported to make inaccurate measurements of polyp size.7
Measurement bias, which is present during the evaluation of both endoscopy and pathology, needs to be addressed for accurate polyp size estimation. Polyps at the periphery of the displayed image are distorted because the objective lens of the endoscope has a fisheye-like structure. Thus, polyps located in the periphery are smaller than those in the central parts of the display. Grasping, removal, and formalin fixation of polyps may cause tissue shrinkage and smaller measurements in pathology evaluation.8 Therefore, the use of tools, including biopsy forceps and endoscopic snares, has been suggested for accurate size estimation of colorectal polyps in vivo. These tools have been reported to facilitate more accurate estimation than subjective visual estimation. However, using an additional tool requires more time and effort, and these disposable tools are wasted, particularly when polyps are not removed. In addition, the polyp size estimated using such tools is not always accurate. For example, these tools sometimes cannot orient along the greatest dimension of the polyp. Depending on the distance of the endoscope from the polyp and how hard the devices are pushed against the colon wall, the measured polyp size may vary. To improve the accuracy of polyp size estimation for all endoscopists in a clinical situation, simple and convenient endoscopic tools with high accuracy and low inter/intraobserver variability should be developed.
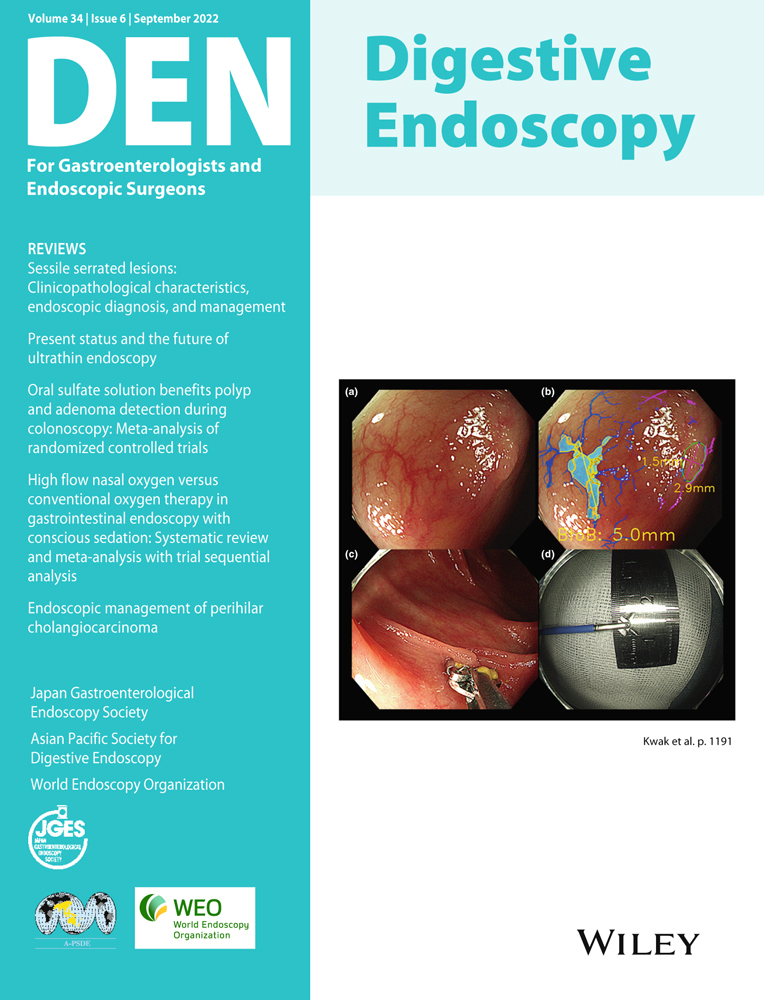
In this issue of Digestive Endoscopy, Kwak et al. demonstrated the usefulness of a newly developed computer-aided tool based on artificial intelligence (AI) for the accurate measurement of colorectal polyps.9 Although AI has already made significant progress in the automatic detection and characterization of colorectal polyps, this would be the first report to use AI for measuring polyp size. To accurately measure the polyp size in vivo, it is necessary to establish a reference distance. The bifurcation-to-bifurcation technique, which refers to the distances between the bifurcations of the main vessels seen in the background mucosa, allowed for higher accuracy and reliability than visual estimation by expert endoscopists and measurement using open-biopsy forceps. Moreover, AI performance did not vary according to polyp size, unlike the measurements made through visual estimation by endoscopists. This new high-performance method may allow for uniform and consistent surveillance intervals and therapeutic strategies. In addition, if AI is implemented in the endoscopic system, polyp size could be measured quickly without using other devices. Although new through-the-scope devices for accurate measurement, such as graduated injection needles, ruler snares, calibrated hoods, virtual tape measures, or structured light laser probes have been explored, AI measurement does not require additional devices and would be more ideal for measuring polyp size. In this regard, endoscopy with a virtual scale function reported by Yoshioka et al.,10 which calculates the length using the position of the laser spot from the endoscope, may also be convenient and useful.
However, the new AI measurement method has a glaring issue that needs to be resolved. Polyp size can vary depending on how it is measured and bowel conditions during colonoscopy, including the amount of insufflated air and the presence of peristalsis. Thus, a real in vivo accurate polyp size remains elusive, even if endoscopists use reliable measurement methods. Therefore, it is difficult to directly prove the accuracy of measurements using the AI method. This problem also applies to the development of other innovative tools for accurate polyp size measurement. To solve this problem, the definition of accurate polyp size should be clarified. As long as the definition of accurate polyp size is ambiguous, strategies for colorectal polyps based on polyp size, including the postcolonoscopy surveillance interval, policy for endoscopic resection or follow-up observation, and appropriate resection method would also be inaccurate and inconsistent. In contrast, new tools with high reliability, such as the AI method reported by Kwak et al., may provide accurate and standardized measurements for the definition of accurate polyp size. If polyp size can be measured using common methods with high accuracy and reliability, strategies based on polyp size can be appropriately considered.
The adaptation of a new, accurate, and easy method for polyp size estimation in a clinical situation will allow us to recognize the inaccuracy of current conventional methods for polyp size estimation. It is important to note the importance of accurate polyp size estimation. The emergence of new AI methods for polyp size estimation will not only improve its accuracy, but also draw attention to concerns regarding inaccurate polyp size estimation. In the future, based on the polyp size measured using reliable methods, including the AI method, endoscopists may need to reconsider polyp management.
CONFLICT OF INTEREST
Authors declare no conflict of interest for this article.
FUNDING INFORMATION
None.