WEO Newsletter
Get Ready: The 103rd JGES Congress and ENDO 2022, May 13–15, 2022 in Kyoto, Japan
The JGES Congress and ENDO World Congress of GI Endoscopy are premier scientific and internationally renowned conferences for endoscopists from every corner of the globe, offering the latest endoscopic education and best practice.
Established in 1959, the first conference of JGES was the Gastro-camera conference. Today, JGES regularly organizes biannual congresses and educational seminars, as well as local conferences.
The first WEO World Congress of GI Endoscopy was held in 2017, and the second ‒ ENDO 2020 ‒ which was co-hosted by the Brazilian Society of Digestive Endoscopy (SOBED) and the cooperating society the Interamerican Society of Digestive Endoscopy (SIED), recently concluded in Rio de Janeiro with great success. These international events have strengthened WEO's position as an authority figure on GI endoscopy, serving as a platform to bring the global endoscopy community together, promote international exchange, and establish best practices.
Save the date in your calendar and broaden your knowledge of endoscopic techniques. Let outstanding practitioners show you the future of GI endoscopy.
For updates on ENDO 2022, stay tuned and go to the WEO website at http://www.worldendo.org/weo-congresses/
For more details on the 103rd JGES Congress, please view here https://www.jges.net/english.
Tips and Tricks: Endoscopic Cryoablation of Barrett’s Esophagus and Esophageal Cancer
By Dr Amitabh Chak, Brenda and Marshall B. Brown Master Clinician in Innovation and Discovery at University Hospitals, Cleveland, USA
- Cryoablation is part of an endoscopist’s armamentarium. It should be used in combination with mucosal resection, submucosal dissection, and radiofrequency ablation to manage dysplastic Barrett’s esophagus (BE) or early esophageal cancer. My approach to dysplastic Barrett’s at the initial endoscopy is usually to perform mucosal resection of small nodular areas or submucosal dissection of wider nodular areas. The advantage of resection techniques is the acquisition of a pathologic specimen. Identification of invasive cancer can change the approach to surgical esophagectomy. I perform cryoablation or radiofrequency ablation (RFA) at the first endoscopic session only if there is flat dysplasia. I still consider RFA my first “go to” ablative modality for eradicating flat dysplasia or residual BE because RFA has a stronger evidence base and is better established. In some instances I will choose cryoablation over RFA, for example, when I find the patient has considerable pain after RFA, fails to respond after an initial session of RFA (<50% restitution), or the esophagus is so tortuous that I do not feel the RFA probe will be able to make contact with the esophageal mucosa.
- I find cryoablation with liquid nitrogen to be useful in select cases of depressed ulcerated early cancers and to palliate nodular cancers that are not amenable to stents.
- Cryoablation is also a good option for local control in selected patients who have had local cancer recurrence after chemoradiation.
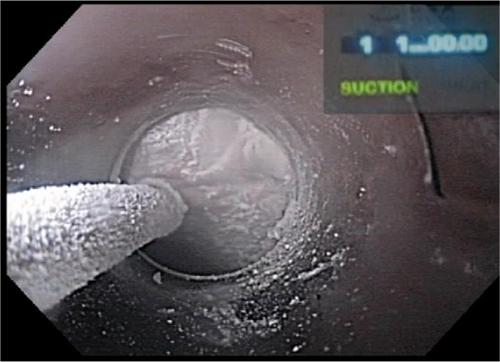
- The effectiveness of cryoablation is based on effective freezing and then complete thawing. Cell death occurs as a result of frozen ice crystals and then the formation of reactive oxygen species during reperfusion. Thus, it is important to ensure that the patient is given supplemental oxygen and equally important to allow frozen tissue to thaw in between freeze cycles.
- The trick with liquid nitrogen cryoablation is to ensure effective venting. The venting tube is designed to vent the entire stomach and should be working effectively before cryoablation is started. The stomach should be monitored by an assistant to ensure that it does not get distended. The dosimetry of cryoablation and the depth of tissue injury depends on freeze time. When using liquid nitrogen it is important to make sure that the delivery catheter has no kinks and the catheter has been primed. I turn the timer on only when I see the treated surface is completely frozen and then treat fully until the pre-programmed freeze time, generally 20-second freezes at a time.
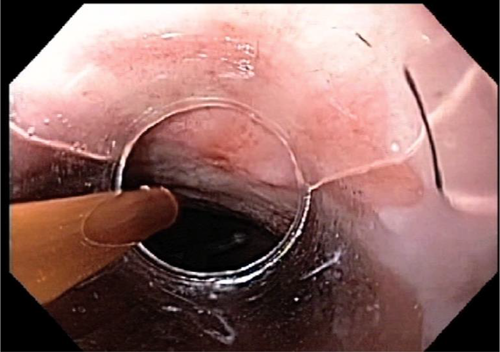
- I like using a clear transparent cap to deliver liquid nitrogen. The lens will fog over during the freeze, but a cap allows stable positioning and better visualization.
- I prefer balloon cryoablation with nitrous oxide to liquid nitrogen for flat dysplastic BE. It is important to have an assistant with experience when performing balloon cryoablation. An experienced assistant helps position the rotatable transducer exactly where needed.
- I prefer doing balloon cryoablation with a high definition therapeutic channel upper endoscope. The high definition scope provides a better view of the area to be ablated through the balloon.
- Balloon cryoablation can be tricky if there is a focal area of narrowing from a prior EMR. I dilate these areas prior to performing balloon cryoablation otherwise the balloon may jump back and forth across the narrowed focal stenosis.
- I prefer starting distally at the GE junction and treating circumferentially at the GE junction before addressing the more proximal areas of BE. The trick to minimizing overlap and avoiding strictures may be to work either clockwise or counterclockwise in one particular area without moving the endoscope.
- The response to cryoablation is difficult to predict. Some patients respond remarkably to the first session of ablation. Others take longer. I tell patients that it might take up to five sessions. I also meet all patients in the office and discuss ablative therapy with them in detail to make sure the patient and family understand that ablative therapies are not a one-session “cure.” I also call patients to make sure they return for ablation. A few patients who undergo ablation will progress to cancer. The few patients I have had who developed advanced cancers after endoscopic therapy were patients who refused to return for surveillance and were lost to follow-up.
AUTHOR: Dr Amitabh Chak, Brenda and Marshall B. Brown Master Clinician in Innovation and Discovery at University Hospitals, Cleveland, USA, began his endoscopic research in BE as a junior attending at UHC/Case Western Reserve University. Supported by an ASGE pilot grant, he discovered that BE and cancers aggregated in certain families. He then obtained funding from the National Institutes of Health to develop transnasal endoscopic screening and to study this new syndrome. He was also awarded a “K24” grant, which allowed him to mentor a number of clinical investigators who have gone on to independent academic careers at other institutions.
His major focus in BE and esophageal adenocarcinoma has been on the epidemiology and genetics of familial BE, with the discovery of VSIG10L as the first susceptibility gene for familial BE. This interest has expanded to other aspects of these diseases including early detection, the role of obesity and specifically of adipokines, and genetic biomarkers. He is currently the Principal Investigator of a Barrett’s Esophagus Translational Research Network (BETRNet) group that is developing translational applications by investigating the genetics, epigenetics and transcriptomics of BE and esophageal adenocarcinoma. They have developed a molecular biomarker-based method for the nonendoscopic detection of Barrett’s esophagus, that is currently undergoing clinical trial.
GAIN EXCLUSIVE ACCESS TO WEO EDUCATIONAL PROGRAMS
Sign up for WEO Individual Membership online
WEO is committed to developing and implementing quality education in digestive endoscopy, engaging endoscopists worldwide in active learning and in programs designed to foster high quality and safe endoscopy.
As an WEO individual member you receive exclusive access to WEO’s renowned educational programs, such as WEO International School of EUS (WISE) and WEO Fellowship Program which offer cutting-edge clinical and practice education with practical skills sessions, small-group discussions and workshops to develop your specialist knowledge.
Join WEO as an individual member now and take advantage of these valuable opportunities to enhance your professional career. WEO individual membership is open to physicians and professionals around the world who specialize in gastrointestinal endoscopy. Explore WEO educational programs and go to http://www.worldendo.org/education/.
To see all membership benefits, go to http://www.worldendo.org/individual-membership/membership-benefits/, follow the straightforward online application process and become part of WEO’s endoscopy community.
WEO Events Calendar
WEO upcoming events
- Colorectal Cancer Screening Committee Meeting 2020 – Europe October 9, 2020 – Amsterdam, The Netherlands
WEO-endorsed events
2020
- 3rd South Pacific International Congress of Gastroenterology and Endoscopy & 9th Live Endoscopy Course of IECED 2020 May 22–24, 2020 – Guayaquil, Ecuador
- 5th Athens International Symposium on Digestive Diseases 2020 July 3–4, 2020 – Athens, Greece
- International Digestive Endoscopy Network 2020 (IDEN 2020) NEW DATE: September 24–27, 2020 ‒ Seoul, Korea
- Ghent International Endoscopy Quality Symposium October 7–8, 2020 – Ghent, Belgium
- EDDW 2020: The 18th Annual Conference of the Egyptian Society for the Study of Endoscopy & Hepatogastroenterology NEW DATE: October 28‒30, 2020 – Cairo, Egypt
2021
- 38th GEEW (Gastroenterology and Endotherapy European Workshop) NEW DATE: June 20–22, 2021 – Brussels, Belgium
For more information, please visit http://www.worldendo.org/events.
For latest information on COVID-19 and how you should protect your self and care for your patients visit, please see http://www.worldendo.org/2020/03/24/weo-advice-on-digestive-endoscopy-and-the-covid-19-pandemic/