Evaluation of current status and near future perspectives of capsule endoscopy: Summary of Japan Digestive Disease Week 2019
1 Introduction
Capsule endoscopy (CE) is now recommended for evaluating patients with overt or occult obscure gastrointestinal bleeding (OGIB), iron deficiency anemia, inflammatory bowel disease (IBD), and small intestinal tumors in patients with polyposis syndrome.1 Nearly 20 years have passed since its first application to humans; remarkable improvements have already been made to achieve a wider view and clear images in addition to the exclusively adaptive frame-rate technology, which adjusts the rate of image capture depending on the movement speed. At present, third-generation PillCam SB3 (Medtronic, Minneapolis, MN, USA), second-generation EndoCapsule EC-10 (Olympus Corporation, Tokyo, Japan) for small bowel, PillCam Crohn’s System (Medtronic) for small and large bowels, second-generation PillCam Colon 2 (Medtronic) for large bowel, MiroCam (IntroMedic, Seoul, Korea) for 3D image system, and several other devices manufactured in China are available for general use.
This editorial summarizes current topics of CE based on the reports presented at the Japan Digestive Disease Week 2019 International Session 8 titled “Evaluation of the Current Status and Near-future Perspectives of CE.” Table 1 presents the agenda of this session.
| Presenter | Title | |
|---|---|---|
| Keynote Lecture | Kenneth K. Wang | Evaluation of current status and near future perspectives of capsule endoscopy |
| Session 8–1 | Yun Jeong Lim | Evaluation of current status and near future perspectives of capsule endoscopy |
| Session 8–2 | Tatsushi Naito | Current capsule endoscopy Pillcam SB3 accurately predicts rebleeding of OGIB |
| Session 8–3 | Yasushi Sato | Capsule endoscopy for small intestinal surveillance in patients with familial adenomatous polyposis |
| Session 8–4 | Ryoichi Miyanaga | Pan-enteroscopic survey for post-allogeneic hematopoietic stem cell transplantation by using colon capsule endoscopy |
| Session 8–5 | Wai K. Leung | Evaluation of current status and near future perspectives of capsule endoscopy |
| Session 8–6 | Hiroto Hiraga | The usefulness of total intestinal survey using colon capsule endoscopy – An interim report on the TOTAL (Total Observation from intestine To Anal Lesion) study |
| Session 8–7 | Satoshi Osawa | Colon capsule endoscopy is a useful tool to assess mucosal healing in patients with ulcerative colitis in clinical remission |
| Session 8–8 | Takafumi Omori | Usefulness of flexible spectral image color enhancement of colon capsule endoscopy for the diagnosis of colorectal polyps and tumors |
| Special Remarks | Hisao Tajiri | Summary and future perspectives |
| Moderators | Haruhiko Ogata, Naoki Ohmiya | |
- JDDW, Japan Digestive Disease Week; OGIB, obscure gastrointestinal bleeding.
2 Evaluation of current status of video ce
2.1 Obscure gastrointestinal bleeding
The diagnostic yield of CE among patients with OGIB varies between 27% and 72%.1 In the Saurin classification, the lesions are grouped into the following three categories based on the risk of bleeding: P0, no potential bleeding; P1, uncertain hemorrhagic potentials such as red spot or small/isolated erosion; and P2, a high bleeding potential such as typical angiomas, large ulcerations, tumors, or varices. This classification is considered useful for evaluating OGIB with CE.2 In a systematic review and meta-analysis of studies using earlier models of CE (M2A, PillCam SB1/2, and MiroCam), Yung et al.3 reported that the pooled rate of rebleeding after negative CE was 19%, and they concluded that negative CE provides adequate evidence of subsequently low rebleeding risk.
Naito et al. (Session 8–2) compared the outcome between PillCam SB1/2, and PillCam SB3 in 73 patients with OGIB and reported that the rebleeding rate was significantly different among patients with P0/P1 lesions (SB1/2 35.7% vs. SB3 5.9%). The rebleeding rate in patients with P2 lesions was 50%. Subanalysis showed that patients who underwent PillCam SB1/2 had more overlooked cases of angioectasia than among those who underwent PillCam SB3. Thus, using the Saurin classification and PillCam SB3 can facilitate better prediction of rebleeding among patients with OGIB.
2.2 IBD
The diagnostic ability of colon CE (CCE) among patients with ulcerative colitis (UC) for assessing disease extent and severity has been evaluated in a few case series. A single-center study conducted in Hong Kong reported that although the capsule excretion rate was low (68%), second-generation PillCam Colon 2 yielded high accuracy in detecting mucosal lesions and determining disease severity among patients with UC, using colonoscopy as the reference.4
Osawa et al. (Session 8–7) also used the second-generation PillCam Colon 2 to analyze 55 examinations in patients with UC and reported that the rate of total colon observation (96.4%) and overall acceptability of patients were high. In addition, the disease activity according to the Mayo endoscopic subscore and UC endoscopic index of severity assessed by CCE correlated well with relapse-free survival. Therefore, CCE may be a useful and reliable tool for disease management in patients with UC.
2.3 Polyposis syndrome
Among patients with known polyposis syndrome, CE can be used to detect jejunal–ileal polyps. A small case series of CE among patients with familial adenomatous polyposis (FAP) reported that the presence of duodenal polyps is related to the presence of jejunal–ileal polyps.5
Sato et al. (Session 8–3) reported a high detection rate (89%) of small bowel polyps using CE in the largest number of patients with FAP (158 patients) to date. Furthermore, the prevalence of small intestinal polyps correlated with the Spigelman stage of the duodenum. Therefore, CE may be of clinical value in selected patients with FAP, especially those with progressed duodenal polyposis.
2.4 Colorectal polyps
Considering that colonoscopy has higher polyp detection rate and that polypectomy can be performed at the same time, routine substitution of CCE with colonoscopy is not recommended.1 However, for patients with a previous incomplete colonoscopy or those who are unable/unwilling to undergo colonoscopy, CCE may be a reasonable alternative; second-generation CCE has 82% sensitivity and 86% specificity in detecting any polyp.1
Omori et al. (Session 8–8) reported that the combination of flexible spectral image color enhancement (FICE) and CCE for detecting and diagnosing colorectal neoplasms yielded promising results. A systematic review and meta-analysis concluded that the use of the FICE mode did not significantly improve the delineation or detection rate of small-bowel CE;6 however, its efficacy in the field of CCE should be further evaluated.
3 Future perspectives of ce
3.1 Artificial intelligence
The application of artificial intelligence (AI) using deep learning-based CE has been reported for automatic detection of angioectasia, erosions, ulcerations, and tumors.7, 8 A computer-aided diagnosis algorithm would be a valuable asset with regard to the time-consuming task of reviewing multiple CE images. Such tools will aid physicians in facilitating and accelerating the CE reviewing process.9
3.2 Pan-enteric examination
Miyanaga et al. (Session 8–4) reported that a pan-enteric survey using PillCam Colon 2 was applicable in patients with post-allogeneic hematopoietic stem cell transplantation to assess the presence of graft-versus-host disease and/or cytomegalovirus infection. Hiraga et al. (Session 8–6) conducted a total colon observation from the intestine to anal lesion study (TOTAL study, UMIN ID: 000027621) to consider the usefulness of CCE. They reported that a high rate (95.4%) of the total colon observation was achieved using CCE and demonstrated high levels of safety and tolerability. To address the increasing demand of pan-enteric examination in patients with Crohn’s disease, Dr. Wai K. Leung (Session 8–5) suggested that PillCam Crohn’s capsule would be more useful because CCE is not designed for pan-enteric examination and a considerable proportion of small-bowel images were omitted. He and Dr. Yun Jeong Lim (Session 8–1) also mentioned that further refinement of technologies for steering the capsule, such as magnetic-controlled CEs,10 would facilitate pan-endoscopy for the whole gastrointestinal tract.
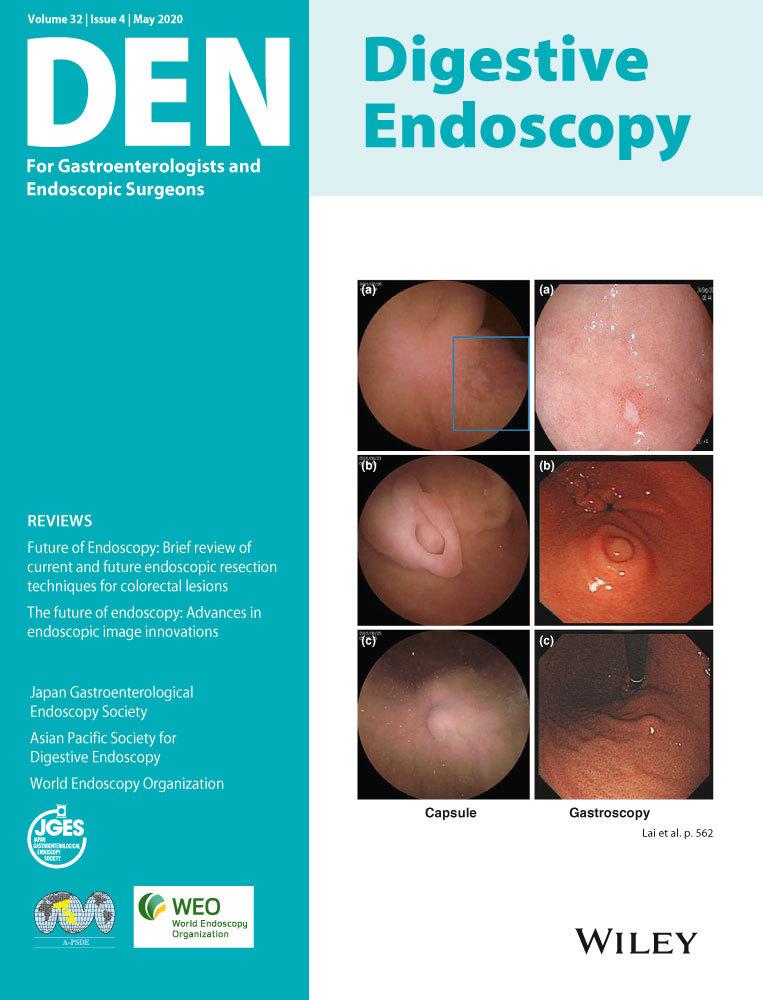
In addition, Dr. Yun Jeong Lim reported that the newly developed 3D image CE (MiroCam) would enable more accurate size estimation and localization of detected lesions.
3.3 Therapeutic applications
In the keynote lecture, Dr. Kenneth K. Wang introduced recent technologies of CE for therapeutic applications. The next generation “OdoCapsule” is a tracking capsule with accurate lesion localization and video stabilization capabilities. In combination with medical engineering, drug delivery systems, such as hemospray, within a capsule would allow for targeted treatment of bleeding sites. Capsules releasing nanorobots that could target neoplasia and bleeding sites would pave the way to a new era of intraluminal operations.
The development of CE has resulted in a widespread use of this tool for the diagnosis and treatment management of the GI tract. In fact, the field of CE is rapidly improving with 3D imaging, active control, and AI technology. The integration of medical engineering and nanotechnology would provide further evolution of therapeutic CEs, which will likely have profound effects on the improvement of patient care.
Conflict of Interest
Dr Naomi Kakushima is an associate editor of Digestive Endoscopy. Other authors declare no conflict of interests for this article.