Endoscopic ultrasound-guided hepaticogastrostomy for intraductal papillary neoplasm of bile duct with obstructive jaundice and cholangitis due to mucus overproduction
Abstract
Watch a video of this article
1 Brief Explanation
An 84-year-old woman was diagnosed with intraductal papillary neoplasm of bile duct (IPNB) in the right intrahepatic bile duct (IHBD) three years previously. She received best supportive care due to her age.
She was admitted to our hospital after repeated episodes of cholangitis over a one-year period. Blood tests revealed elevated hepatobiliary enzymes, bilirubin and carcinoembryonic antigen.
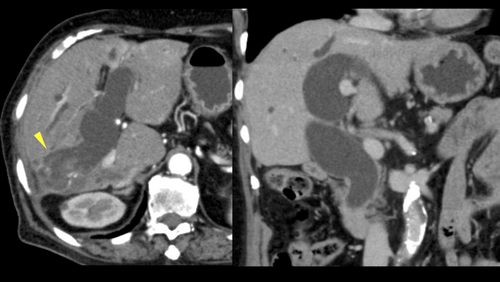
Abdominal computed tomography showed a tumor with contrast effect in the right IHBD and dilatation of the common bile duct (CBD; Fig. 1). No obvious stenosis was observed in the CBD or IHBD. We considered that the obstructive jaundice was due to mucus overproduction.
Endoscopic retrograde cholangiopancreatography (ERCP) revealed that the CBD to right bile duct was filled with mucus, which was not observed on imaging. The left IHBD was significantly dilated (Fig. 2).

Covered metallic stents were placed in the unaffected bile duct using the side-by-side method after removing the mucus using a balloon catheter. The stent was insufficiently fixed in the bile ducts due to the absence of biliary stricture and spontaneously slipped out of the bile duct into the intestine after a few days. ERCP and percutaneous transhepatic cholangiodrainage were not effective treatments. Thus, we performed EUS-HGS of the left IHBD using a partially covered self-expanding metal stent (10 mm, 10 cm; Video S1).
The cholangitis and jaundice improved within a few days after EUS-HGS and the patient was discharged after one week, without adverse events. EUS-HGS is an alternative to biliary drainage for treating malignant biliary strictures for which transpapillary approaches have failed.1-3 IPNB often causes obstructive jaundice and cholangitis due to mucus overproduction.4, 5
This is the first report demonstrating the utility of EUS-HGS for IPNB with obstructive jaundice due to mucus overproduction without malignant biliary stricture.
Authors declare no conflicts of interest for this article.