Endoscopic submucosal dissection for multiple gastric superficial adenocarcinomas identified in patient with familial adenomatous polyposis
Abstract
Watch a video of this article
Brief Explanation
A 31-year-old female who was diagnosed as having familial adenomatous polyps (FAP) at 13 years of age, was introduced to our hospital to treat gastric neoplasms. She had approximately 1000 polyps in the colon, and also had many polyps in the upper two-thirds of stomach. Preoperative endoscopic examination revealed multiple flat elevated lesions in the greater curvature side (Fig. 1a,b). According to the features of magnifying narrow band imaging, these lesions were endoscopically diagnosed as gastric type adenocarcinoma (Fig. 1c,d). To avoid the occurrence of desmoid tumor (DT), endoscopic submucosal dissection (ESD) was conducted (Video S1). The procedure was performed under general anesthesia, using an upper gastrointestinal endoscope (GIF260J; Olympus, Tokyo, Japan). After the local injection of sodium hyaluronate solution, a circumferential incision was conducted to include all the lesions en-bloc. Submucosal dissection was performed using dual knife and IT knife 2 (Olympus). Counter traction method was applied to make a good endoscopic field of vision (Fig. 2a). The lesion was successfully resected en-bloc, without any adverse events, and the procedure time was 235 min (Fig. 2b). Polygycolic acid sheets and fibrin glue were applied to post-ESD ulcer floor to prevent delayed perforation (Video S2). The resected specimen included seven intramucosal adenocarcinomas corresponding to Vienna Classification Category 4, resulting in a curative resection (Fig. 2c,d).

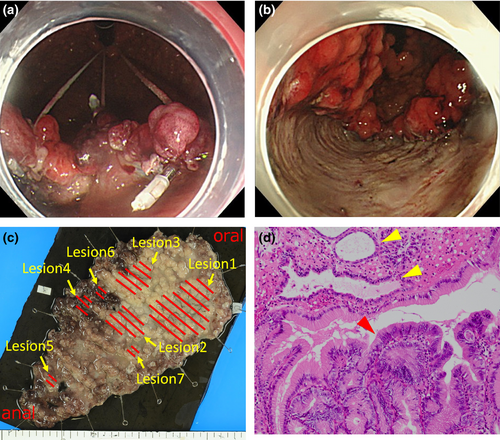
In patients with FAP, approximately 90% of DTs occur after abdominal surgery,1 and it is the second largest cause of death.2 Since the majority of DTs in FAP are characterized by the involvement of mesentery and abdominal wall,3 endoscopic treatment expected to reduce the risk of DT development, whose damage is limited to the submucosal layer. Using the counter traction technique,4, 5 we could successfully resect multiple gastric neoplasms located at greater curvature side where ESD application is technically challenging, indicating that endoscopic treatment seems to be the preferable treatment option for them.
Authors declare no conflict of interest for this article.