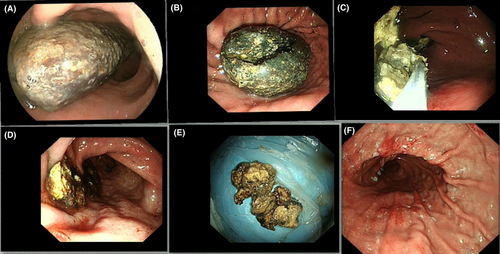
New application of dual knife: Easier removal of a giant gastric bezoar
Abstract
Watch a video of this article
Brief Explanation
A 70-year-old man was admitted to our emergency department for hematemesis. On 2 November 2018, he underwent gastroscopy (GIF450; Fujinon, Tokyo, Japan) that revealed a giant bezoar occupying the thoracic portion of the stomach (Fig. 1A). Initial attempts to remove the bezoar with a snare were unsuccessful. Then, the patient consumed Coca-Cola for 1 week. On 10 November 2018, a repeat endoscopy (GIFH260; Olympus, Tokyo, Japan) revealed that the bezoar had persisted. We then cut the hard surface of the bezoar and split it into parts with a dual knife (KD-650Q; Olympus). We used the Erbe VIO 200 D (Erbe China, Shanghai, China) high-frequency generator. The electrosurgical unit setting for using the dual knife during this procedure were ENDO CUT Q (Erbe China) and the forced coagulation mode, in which the parameters were: effect 3, cutting width 2, cutting time interval 4, peak-power 50 W and peak point voltage 1100 Vp. (Fig. 1B, Video S1). Next, we cut the giant gastric bezoar into pieces with a snare (Mednova Technology China, Hangzhou, China) and extracted the parts (Fig. 1C–E; Video S1). The procedure required approximately 1 h; slight gastric mucosal injury occurred. A follow-up gastroscopy on 14 November 2018 revealed no bezoar (Fig 1F). Gastric bezoar can be treated by drinking Coca-Cola, endoscopic removal and surgical removal.1 Methods of endoscopic removal include improved snare,2 biopsy or alligator forceps, basket catheter, argon plasma coagulation device and electrohydraulic device. However, for a giant hard gastric bezoar, surgical removal is the best choice.1 To our knowledge, this is the first report on removal of a gastric bezoar using a dual knife, although a dual knife has been used to remove an embedded self-expandable metallic stent.3 The dual knife can break the hard surface and divide the bezoar into parts, facilitating easy removal and eliminating the need for surgery.
Authors declare no conflict of interests for this article.
Acknowledgments
This study was funded by the China Postdoctoral Science Foundation (grant no. 2018M630112) and The Project of Scientific Research and Development of North Sichuan Medical College (grant no. CBY17-A-ZD16). We thank the patient and his sons for agreeing to this video presentation.