Endoscopic radiofrequency biliary ablation treatment: A comprehensive review
Corresponding Author
Alberto Larghi
Digestive Endoscopy Unit, Fondazione Policlinico Universitario A. Gemelli, IRCCS, Rome, Italy
Corresponding: Alberto Larghi, Digestive Endoscopy Unit, Dipartimento Scienze Gastroenterologiche, Endocrino-Metaboliche e Nefro-Urologiche, Fondazione Policlinico Universitario A. Gemelli, IRCCS, Largo A. Gemelli 8, 00168 Rome, Italy. Email: [email protected]Search for more papers by this authorMihai Rimbaș
Gastroenterology Department, Colentina Clinical Hospital, Carol Davila University of Medicine, Bucharest, Romania
Search for more papers by this authorAndrea Tringali
Digestive Endoscopy Unit, Fondazione Policlinico Universitario A. Gemelli, IRCCS, Catholic University, Rome, Italy
Search for more papers by this authorIvo Boškoski
Digestive Endoscopy Unit, Fondazione Policlinico Universitario A. Gemelli, IRCCS, Rome, Italy
Search for more papers by this authorGianenrico Rizzatti
Digestive Endoscopy Unit, Fondazione Policlinico Universitario A. Gemelli, IRCCS, Rome, Italy
Search for more papers by this authorGuido Costamagna
Digestive Endoscopy Unit, Fondazione Policlinico Universitario A. Gemelli, IRCCS, Catholic University, Rome, Italy
IHU-USIAS, University of Strasbourg, Strasbourg, France
Search for more papers by this authorCorresponding Author
Alberto Larghi
Digestive Endoscopy Unit, Fondazione Policlinico Universitario A. Gemelli, IRCCS, Rome, Italy
Corresponding: Alberto Larghi, Digestive Endoscopy Unit, Dipartimento Scienze Gastroenterologiche, Endocrino-Metaboliche e Nefro-Urologiche, Fondazione Policlinico Universitario A. Gemelli, IRCCS, Largo A. Gemelli 8, 00168 Rome, Italy. Email: [email protected]Search for more papers by this authorMihai Rimbaș
Gastroenterology Department, Colentina Clinical Hospital, Carol Davila University of Medicine, Bucharest, Romania
Search for more papers by this authorAndrea Tringali
Digestive Endoscopy Unit, Fondazione Policlinico Universitario A. Gemelli, IRCCS, Catholic University, Rome, Italy
Search for more papers by this authorIvo Boškoski
Digestive Endoscopy Unit, Fondazione Policlinico Universitario A. Gemelli, IRCCS, Rome, Italy
Search for more papers by this authorGianenrico Rizzatti
Digestive Endoscopy Unit, Fondazione Policlinico Universitario A. Gemelli, IRCCS, Rome, Italy
Search for more papers by this authorGuido Costamagna
Digestive Endoscopy Unit, Fondazione Policlinico Universitario A. Gemelli, IRCCS, Catholic University, Rome, Italy
IHU-USIAS, University of Strasbourg, Strasbourg, France
Search for more papers by this authorAbstract
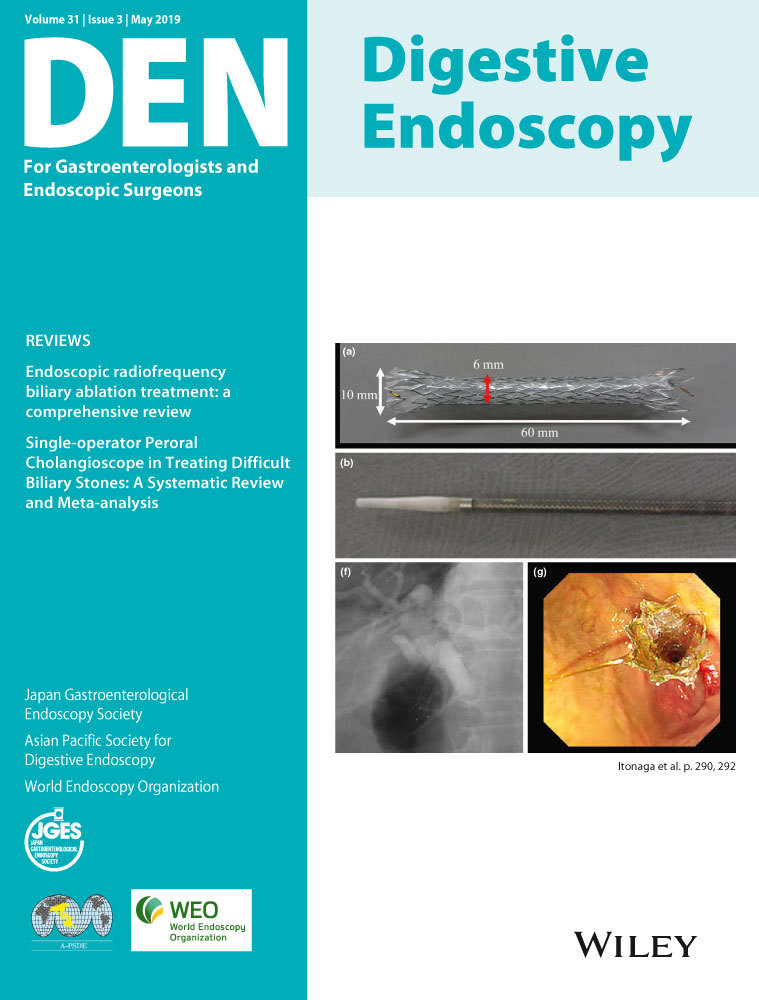
Radiofrequency ablation (RFA) functions by delivering thermal energy within tissue, the result of a high-frequency alternating current released from an active electrode, leading to coagulative necrosis and cellular death. Recently, a biliary catheter working on a guidewire has been developed and a number of studies have so far been carried out. The present article provides a comprehensive review of the literature on the results of the use of RFA for the clinical management of patients with unresectable malignant biliary strictures, benign biliary strictures, and residual adenomatous tissue in the bile duct after endoscopic papillectomy. Available data show that biliary RFA treatment is a promising adjuvant therapy in patients with unresectable malignant biliary obstruction. The procedure is safe, well tolerated and improves stent patency and survival, even though more studies are warranted. In patients with residual endobiliary adenomatous tissue after endoscopic papillectomy, a significant rate of neoplasia eradication after a single RFA session has been reported, thus favoring this treatment over surgical intervention. In these patients, as well as in those with benign biliary strictures, dedicated probes with a short electrode able to focus the RF current on the short stenosis are needed to expand RFA treatment for these indications.
Conflicts of Interest
Authors declare no conflicts of interest for this article.
References
- 1O'Neal D, Cohen T, Peterson C et al. Contrast-enhanced ultrasound-guided radiofrequency ablation of renal tumors. J. Kidney Cancer VHL 2018; 5: 7–14.
- 2Pescatori LC, Torcia P, Nicosia L et al. Which needle in the treatment of thyroid nodules? Gland Sur. 2018; 7: 111–6.
- 3Yin Z, Jin H, Ma T et al. A meta-analysis of long-term survival outcomes between surgical resection and radiofrequency ablation in patients with single hepatocellular carcinoma < 2 cm (BCLC very early stage). Int. J. Surg. 2018; 56: 61–7.
- 4Boss A, Clasen S, Kuczyk M et al. Image-guided radiofrequency ablation of renal cell carcinoma. Eur. Radiol. 2007; 17: 725–33.
- 5Plasencia Martínez JM. Pulmonary radiofrequency ablation (Part 1): current state. Radiologia 2015; 57: 275–86.
- 6Schueller G, Kettenbach J, Sedivy R et al. Heat shock protein expression induced by percutaneous radiofrequency ablation of hepatocellular carcinoma in vivo. Int. J. Oncol. 2004; 24: 609–13.
- 7Haen SP, Pereira PL, Salih HR et al. More than just tumor destruction: immunomodulation by thermal ablation of cancer. Clin. Dev. Immunol. 2011; 2011: 160250.
- 8Rai R, Richardson C, Flecknell P et al. Study of apoptosis and heat shock protein (HSP) expression in hepatocytes following radiofrequency ablation (RFA). J. Surg. Res. 2005; 129: 147–51.
- 9Ali MY, Grimm CF, Ritter M et al. Activation of dendritic cells by local ablation of hepatocellular carcinoma. J. Hepatol. 2005; 43: 817–22.
- 10Khorsandi SZD, Vavra P. The modern use of radiofrequency energy in surgery, endoscopy and interventional radiology. Eur. Surg. 2008; 40: 204–10.
- 11Itoi T, Isayama H, Sofuni A et al. Evaluation of effects of a novel endoscopically applied radiofrequency ablation biliary catheter using an ex-vivo pig liver. J. Hepatobiliary Pancreat. Sci. 2012; 19: 543–7.
- 12Steel AW, Postgate AJ, Khorsandi S et al. Endoscopically applied radiofrequency ablation appears to be safe in the treatment of malignant biliary obstruction. Gastrointest. Endosc. 2011; 73: 149–53.
- 13Figueroa-Barojas P, Bakhru MR, Habib NA et al. Safety and efficacy of radiofrequency ablation in the management of unresectable bile duct and pancreatic cancer: a novel palliation technique. J. Oncol. 2013; 2013: 910897.
- 14Dolak W, Schreiber F, Schwaighofer H et al. Endoscopic radiofrequency ablation for malignant biliary obstruction: a nationwide retrospective study of 84 consecutive applications. Surg. Endosc. 2014; 28: 854–60.
- 15Sharaiha RZ, Natov N, Glockenberg KS et al. Comparison of metal stenting with radiofrequency ablation versus stenting alone for treating malignant biliary strictures: is there an added benefit? Dig. Dis. Sci. 2014; 59: 3099–102.
- 16Tal AO, Vermehren J, Friedrich-Rust M et al. Intraductal endoscopic radiofrequency ablation for the treatment of hilar non-resectable malignant bile duct obstruction. World J. Gastrointest. Endosc. 2014; 6: 13–9.
- 17Sharaiha RZ, Sethi A, Weaver KR et al. Impact of radiofrequency ablation on malignant biliary strictures: results of a collaborative registry. Dig. Dis. Sci. 2015; 60: 2164–9.
- 18Kallis Y, Phillips N, Steel A et al. Analysis of endoscopic radiofrequency ablation of biliary malignant strictures in pancreatic cancer suggests potential survival benefit. Dig. Dis. Sci. 2015; 60: 3449–55.
- 19Laquière A, Boustière C, Leblanc S et al. Safety and feasibility of endoscopic biliary radiofrequency ablation treatment of extrahepatic cholangiocarcinoma. Surg. Endosc. 2016; 30: 1242–8.
- 20Wang F, Li Q, Zhang X et al. Endoscopic radiofrequency ablation for malignant biliary strictures. Exp. Ther. Med. 2016; 11: 2484–8.
- 21Schmidt A, Bloechinger M, Weber A et al. Short-term effects and adverse events of endoscopically applied radiofrequency ablation appear to be comparable with photodynamic therapy in hilar cholangiocarcinoma. United European Gastroenterol. J. 2016; 4: 570–9.
- 22Laleman W, van der Merwe S, Verbeke L et al. A new intraductal radiofrequency ablation device for inoperable biliopancreatic tumors complicated by obstructive jaundice: the IGNITE-1 study. Endoscopy 2017; 49: 977–82.
- 23Yang J, Wang J, Zhou H et al. Efficacy and safety of endoscopic radiofrequency ablation for unresectable extrahepatic cholangiocarcinoma: a randomized trial. Endoscopy 2018; 50: 751–60.
- 24Hu B, Sun B, Cai Q et al. Asia-Pacific consensus guidelines for endoscopic management of benign biliary strictures. Gastrointest. Endosc. 2017; 86: 44–58.
- 25Dawwas MF, Oppong KW, Webster GJ. Endoscopic assessment and management of biliary strictures. Frontline Gastroenterol. 2016; 7: 170–5.
- 26Smith AC, Dowsett JF, Russell RC et al. Randomised trial of endoscopic stenting versus surgical bypass in malignant low bile duct obstruction. Lancet 1994; 344: 1655–60.
- 27Zorrón PuL, de Moura EG, Bernardo WM et al. Endoscopic stenting for inoperable malignant biliary obstruction: a systematic review and meta-analysis. World J. Gastroenterol. 2015; 21: 13374–85.
- 28Loew BJ, Howell DA, Sanders MK et al. Comparative performance of uncoated, self-expanding metal biliary stents of different designs in 2 diameters: final results of an international multicenter, randomized, controlled trial. Gastrointest. Endosc. 2009; 70: 445–53.
- 29Inoue T, Ito K, Yoneda K. Antegrade radiofrequency ablation and stenting for biliary stricture through endoscopic ultrasound-guided hepaticogastrostomy. Dig. Endosc. 2018; 30: 793–4.
- 30Inoue T, Ito K, Yoneda K. Radiofrequency ablation combined with multiple biliary metal stent placement using short-type single-balloon endoscope in patients with surgically altered anatomy. Dig. Endosc. 2018; 30: 395–6.
- 31Sofi AA, Khan MA, Das A et al. Radiofrequency ablation combined with biliary stent placement versus stent placement alone for malignant biliary strictures: a systematic review and meta-analysis. Gastrointest. Endosc. 2018; 87: 944–51.
- 32Kadayifci A, Atar M, Forcione DG et al. Radiofrequency ablation for the management of occluded biliary metal stents. Endoscopy 2016; 48: 1096–101.
- 33Nayar MK, Oppong KW, Bekkali NLH et al. Novel temperature-controlled RFA probe for treatment of blocked metal biliary stents in patients with pancreaticobiliary cancers: initial experience. Endosc. Int. Open 2018; 6: E513–7.
- 34Yoon WJ, Kim YT, Daglilar ES et al. Evaluation of bipolar radiofrequency ablation for occluded self-expandable metal stents in the bile duct: in vivo and in vitro study. Endoscopy 2015; 47: 1167–70.
- 35Ogura T, Onda S, Sano T et al. Evaluation of the safety of endoscopic radiofrequency ablation for malignant biliary stricture using a digital peroral cholangioscope (with videos). Dig. Endosc. 2017; 29: 712–7.
- 36Costamagna G, Shah SK, Tringali A. Current management of postoperative complications and benign biliary strictures. Gastrointest. Endosc. Clin. N. Am. 2003; 13: 635–48.
- 37Parsi MA. Common controversies in management of biliary strictures. World J. Gastroenterol. 2017; 23: 1119–24.
- 38Costamagna G, Pandolfi M, Mutignani M et al. Long-term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents. Gastrointest. Endosc. 2001; 54: 162–8.
- 39Costamagna G, Tringali A, Mutignani M et al. Endotherapy of postoperative biliary strictures with multiple stents: results after more than 10 years of follow-up. Gastrointest. Endosc. 2010; 72: 551–7.
- 40Dumonceau JM, Tringali A, Blero D et al. Biliary stenting: indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy 2012; 44: 277–98.
- 41Khan MA, Baron TH, Kamal F et al. Efficacy of self-expandable metal stents in management of benign biliary strictures and comparison with multiple plastic stents: a meta-analysis. Endoscopy 2017; 49: 682–94.
- 42Costamagna G, Familiari P, Tringali A et al. Multidisciplinary approach to benign biliary strictures. Curr. Treat. Options Gastroenterol. 2007; 10: 90–101.
- 43Hu B, Gao DJ, Wu J et al. Intraductal radiofrequency ablation for refractory benign biliary stricture: pilot feasibility study. Dig. Endosc. 2014; 26: 581–5.
- 44Mehendiratta V, Desilets DJ. Use of radiofrequency ablation probe for eradication of residual adenoma after ampullectomy. Gastrointest. Endosc. 2015; 81: 1055–6.
- 45Valente R, Urban O, Del Chiaro M et al. ERCP-directed radiofrequency ablation of ampullary adenomas: a knife-sparing alternative in patients unfit for surgery. Endoscopy 2015; 47: E515–6.
- 46Tian Q, Wang G, Zhang Y et al. Endoscopic radiofrequency ablation combined with fully covered self-expandable metal stent for inoperable periampullary carcinoma in a liver transplant patient: a case report. Medicine (Baltimore) 2017; 96: e5790.
- 47Rustagi T, Irani S, Reddy DN et al. Radiofrequency ablation for intraductal extension of ampullary neoplasms. Gastrointest. Endosc. 2017; 86: 170–6.
- 48Camus M, Napoléon B, Vienne A et al. Efficacy and safety of endobiliary radiofrequency ablation for the eradication of residual neoplasia after endoscopic papillectomy: a multicenter prospective study. Gastrointest. Endosc. 2018; 88: 511–8.
- 49Mavrogenis G, Deprez PH, Wallon J et al. Bile duct adenoma causing recurrent cholangitis: diagnosis and management with targeted Spyglass access and radiofrequency ablation. Endoscopy 2012; 44: E290–1.