Additional chromoendoscopy for colorectal lesions initially diagnosed with low confidence by magnifying narrow-band imaging: Can it improve diagnostic accuracy?
Abstract
Background and Aim
Magnifying chromoendoscopy has been one of the most reliable diagnostic methods for distinguishing neoplastic from non-neoplastic lesions. The aim of this prospective study was to clarify the clinical usefulness of magnifying chromoendoscopy for colorectal polyps initially diagnosed with low confidence (LC) by magnifying narrow-band imaging (NBI).
Methods
Consecutive adult patients who underwent total colonoscopic examination with magnifying NBI between July and December 2016 at Sano Hospital were prospectively recruited. Endoscopists were asked to carry out additional magnifying chromoendoscopy for cases that had been initially diagnosed as Japan NBI Expert Team (JNET) Type 1 or 2A with LC by magnifying NBI. We investigated the diagnostic performance of magnifying NBI for polyps diagnosed as JNET Type 1 or 2A with LC (first phase) and that of subsequent magnifying chromoendoscopy (second phase) in differentiating neoplasia from non-neoplasia.
Results
In 50 patients, we analyzed 53 polyps classified as JNET Type 1 or 2A with LC prediction. Accuracy and negative predictive value of magnifying NBI (first phase) were 58.5% (95% CI, 44.1–71.9%) and 66.0% (95% CI, 36.6–77.9%), and those of magnifying chromoendoscopy (second phase) were 66.0% (95% CI, 51.7–78.5%) and 61.1% (95% CI, 43.5–76.9%), respectively.
Conclusion
Regardless of the findings of additional chromoendoscopy, all polyps should be resected and submitted for histopathological examination when the confidence level in differentiating adenomatous from hyperplastic polyps by magnifying NBI is low.
Introduction
Accurate endoscopic differentiation of neoplasia from non-neoplasia in colorectal polyps is clinically important because it has the potential advantage of obviating the need for histopathological diagnosis and polypectomy.1 In their Preservation and Incorporation of Valuable Endoscopic Innovation (PIVI) statement, the American Society for Gastrointestinal Endoscopy (ASGE) has suggested key thresholds for real-time histological assessment of diminutive colorectal polyps: an agreement rate higher than 90% in determining the post-polypectomy surveillance interval and a negative predictive value (NPV) of 90% or higher for rectosigmoid polyps with an adenomatous histology.2
In recent years, the concept of confidence levels (high or low) has been applied to endoscopic prediction of polyp histology for more accurate diagnosis.1, 3 Previous studies have shown that narrow-band imaging (NBI)-based diagnosis with high confidence (HC) by an expert can achieve a NPV greater than 90%, whereas low-confidence (LC) diagnosis cannot.1, 4 Therefore, there is a need for more accurate NBI-based assessment of colorectal polyps diagnosed with LC. Magnifying chromoendoscopy has been one of the most reliable diagnostic methods used in Japan, yielding an accuracy of 92–99% for differentiating neoplasia from non-neoplasia in colorectal polyps.5-10 However, it is uncertain whether additional magnifying chromoendoscopy has superior diagnostic accuracy over initial magnifying NBI.
The aim of the present study was to clarify whether magnifying chromoendoscopy following magnifying NBI with LC improves diagnostic performance for differentiating neoplasia from non-neoplasia in colorectal polyps.
Methods
Patients
Consecutive adult patients aged 20 years or older who underwent total colonoscopy with NBI magnification between July and December 2016 at Sano Hospital were prospectively enrolled in this study. Exclusion criteria were: (i) history of inflammatory bowel disease, hereditary polyposis syndrome, or Lynch syndrome; (ii) poor bowel preparation; (iii) absence of polyps or presence of unevaluable materials; and (iv) presence of advanced cancer. Written informed consent was obtained from all patients before the examination. The study protocol was approved by the institutional review board of Sano Hospital, Kobe, Japan. The study was registered in a clinical trial registry (UMIN 000023135).
Materials and methods
The procedures were carried out by seven colonoscopists with extensive experience in magnifying colonoscopy with NBI (>1000 cases each). All were familiar with the Japan NBI Expert Team (JNET) classification.11, 12 Magnifying colonoscopes (CF-H260AZI, CF-HQ290I, PCF-Q260AZI, PCF-H290ZI) with LUCERA video processors (Olympus Medical Systems Corporation, Tokyo, Japan) were used. All polyps detected by white light imaging were diagnosed by NBI with magnification, in accordance with the JNET classification (Type 1, 2A, 2B, and 3). The polyps were also assigned a level of confidence (high or low) in terms of predictive accuracy. When endoscopists had more than 90% certainty, they diagnosed polyps with HC.13 Location, size, and shape (Paris classification) of all polyps were recorded.14 All polyps except diminutive polyps (≤5 mm) diagnosed as JNET Type 1 (indicative of hyperplastic or sessile serrated adenoma/polyp [SSA/P]) with HC in the rectosigmoid colon were resected and submitted for histopathological examination. However, endoscopists were allowed to discard any resected diminutive polyps except depressed lesions if they were diagnosed as JNET Type 2A (indicative of low-grade intramucosal neoplasia) with HC. Chromoendoscopy with 0.5% indigocarmine was added for all of the polyps classified as JNET Type 1 or 2A with LC, for diagnosis based on pit pattern. Polyps considered to show a Type II pit pattern (indicative of hyperplasia) were classified as non-neoplastic, and those with a Type III or IV pit pattern (indicative of low-grade intramucosal neoplasia) were classified as neoplastic.15, 16 When it was difficult to classify polyps as JNET Type 2A or 2B, endoscopists were told to diagnose them as JNET Type 2B with LC for the purposes of our study. An experienced gastrointestinal histopathologist (T.F.) blinded to the endoscopic diagnosis classified all specimens according to the World Health Organization classification.17
Variables
Primary outcome measure
Primary outcome was the diagnostic performance of magnifying NBI for polyps diagnosed as JNET Type 1 or 2A with LC (first phase) and that of subsequent magnifying chromoendoscopy (second phase) for differentiation of neoplasia from non-neoplasia. We assumed that chromoendoscopy in addition to NBI would be useful when the upper limit of the 95% confidence interval (CI) for accuracy and the NPV of magnifying chromoendoscopy were greater than 90% according to the PIVI thresholds. The significance of the difference in diagnostic performance between magnifying NBI and magnifying chromoendoscopy was not evaluated because this was not the aim of the present study.
Secondary outcome measure
Secondary outcome was the diagnostic performance of magnifying NBI for differentiating neoplasia from non-neoplasia with HC for diminutive and all colorectal polyps.
Statistical analysis
Our pilot study had shown that the accuracy of subsequent magnifying chromoendoscopy for polyps diagnosed as JNET Type 1 or 2A with LC was 66.7%. Assuming that the accuracy of subsequent magnifying chromoendoscopy was 66.7%, a sample size of 11 polyps diagnosed as JNET Type 1 or 2A with LC would have been required in order to verify that the upper limit of the 95% CI for that accuracy was lower than 90%. A sample size of 51 polyps would have assured that the upper limit of the 95% CI was lower than 80%. Therefore, we used a sample size of 51 polyps, and continuous variables were expressed as mean ± standard deviation (SD). In this study, the 95% CI for diagnostic performance was calculated.
Results
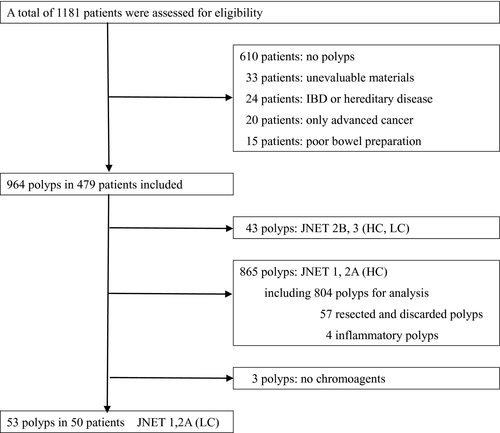
During the study period, 1181 patients underwent total colonoscopy using a magnifying endoscope with NBI. Of those patients, 702 were excluded on the basis of the exclusion criteria, and 479 patients with 964 polyps were enrolled. First, 43 polyps diagnosed as JNET Type 2B or 3 were excluded. Second, among 865 polyps diagnosed as JNET Type 1 or 2A with HC, 57 were resected and discarded, and four inflammatory polyps were omitted after histopathological evaluation. Fifty-six polyps (5.8%) were diagnosed as JNET Type 1 or 2A with LC. As no chromoagents were used, three polyps were omitted from the analysis. Finally, the diagnostic performance of both magnifying NBI and subsequent magnifying chromoendoscopy was evaluated for 53 polyps in 50 patients (Fig. 1).
Diagnostic performance of magnifying NBI for polyps diagnosed as JNET Type 1 or 2A with LC (first phase) and that of subsequent magnifying chromoendoscopy (second phase) for differentiating neoplasia from non-neoplasia
The characteristics of the eligible patients and resected polyps are shown in Table 1. Table 2 shows the diagnostic performance of magnifying NBI for polyps diagnosed as JNET Type 1 or 2A with LC (first phase) and that of subsequent magnifying chromoendoscopy (second phase) for differentiating neoplasia from non-neoplasia. In the first phase, accuracy, sensitivity, specificity, positive predictive value (PPV), and NPV of magnifying NBI were 66.0% (95% CI, 51.7–78.5%), 48.1% (95% CI, 28.7–68.1%), 84.6% (95% CI, 65.1–95.6%), 76.5% (95% CI, 50.1–93.2%), and 61.1% (95% CI, 43.5–76.9%), respectively. In the second phase, the corresponding figures for magnifying chromoendoscopy were 58.5% (95% CI, 44.1–71.9%), 63.0% (95% CI, 42.4–80.6%), 53.8% (95% CI, 33.4–73.4%), 58.6% (95% CI, 38.9–76.5%), and 58.3% (95% CI, 36.6–77.9%), respectively.
| Total patients, n | 50 |
| Male/female | 25/25 |
| Mean age, y (SD) | 62.9 ± 12.0 |
| Polyps, n | 53 |
| Mean size, mm (SD) | 5.4 ± 3.4 |
| Size (diminutive/small/large) | 35/11/7 |
| Location, right/left | 27/26 |
| Shape, protruding/flat/depressed | 8/45/0 |
| Histopathology | |
| HP/SSA/P | 23/3 |
| Adenoma | 27 |
- HP, hyperplastic polyp; SSA/P, sessile serrated adenoma/polyp.
| First phase | Second phase | |
|---|---|---|
| NBI (n = 53) (95% CI) | Chromoendoscopy (n = 53) (95% CI) | |
| Accuracy | 58.5% (44.1–71.9%) | 66.0% (51.7–78.5%) |
| Sensitivity | 63.0% (42.4–80.6%) | 48.1% (28.7–68.1%) |
| Specificity | 53.8% (33.4–73.4%) | 84.6% (65.1–95.6%) |
| PPV | 58.6% (38.9–76.5%) | 76.5% (50.1–93.2%) |
| NPV | 58.3% (36.6–77.9%) | 61.1% (43.5–76.9%) |
- CI, confidence interval; JNET, Japan NBI Expert Team; LC, low confidence; NBI, narrow-band imaging; NPV, negative predictive value; PPV, positive predictive value.
Diagnostic performance of magnifying NBI for polyps diagnosed as JNET Type 1 or 2A with HC
The diagnostic performance of magnifying NBI for JNET Type 1 or 2A polyps with HC was evaluated for 804 polyps in 422 patients, and the results are shown in Table 3. Accuracy, sensitivity, specificity, PPV, and NPV were 91.9% (95% CI, 89.8–93.7%), 99.1% (95% CI, 98.1–99.7%), 56.6% (95% CI, 47.9–65.1%), 91.8% (95% CI, 89.6–93.7%), and 92.8% (95% CI, 84.9–97.3%), respectively. When focused on 563 diminutive polyps, the corresponding figures were 90.1% (95% CI, 87.3–92.4%), 99.4% (95% CI, 98.2–99.9%), 33.8% (95% CI, 23.6–45.2%), 90.1% (95% CI, 87.2–92.5%), and 90.0% (95% CI, 73.5–97.9%), respectively.
| Diminutive polyps (n = 563) (95% CI) | All polyps (n = 804) (95% CI) | |
|---|---|---|
| Accuracy | 90.1% (87.3–92.4%) | 91.9% (89.8–93.7%) |
| Sensitivity | 99.4% (98.2–99.9%) | 99.1% (98.1–99.7%) |
| Specificity | 33.8% (23.6–45.2%) | 56.6% (47.9–65.1%) |
| PPV | 90.1% (87.2–92.5%) | 91.8% (89.6–93.7%) |
| NPV | 90.0% (73.5–97.9%) | 92.8% (84.9–97.3%) |
- CI, confidence interval; HC, high confidence; JNET, Japan NBI Expert Team; NBI, narrow-band imaging; NPV, negative predictive value; PPV, positive predictive value.
Discussion
In the present study, we evaluated the diagnostic performance of additional chromoendoscopy after magnifying NBI with LC for differentiation of neoplasia from non-neoplasia. To our knowledge, this is the first prospective study to have verified the diagnostic strategy for LC cases with magnifying NBI.
We found that the diagnostic performance of magnifying NBI for LC cases was much lower than that for HC cases, in agreement with earlier studies that did not use magnification.3 Furthermore, after additional chromoendoscopy of LC polyps for determination of adenoma or hyperplasia, the upper limit of the 95% CI for accuracy and NPV were clearly lower than the necessary PIVI thresholds, suggesting that it was still difficult to accurately diagnose polyps predicted with LC by magnifying NBI even with additional magnifying chromoendoscopy. Therefore, it seems necessary to resect diminutive polyps diagnosed as JNET Type 1 or 2A with LC and submit them for histopathological analysis.
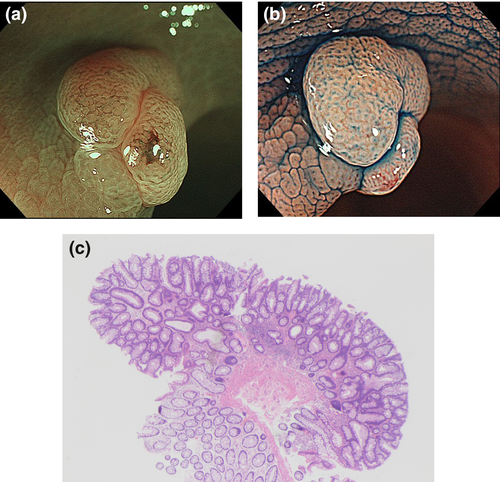
There are several possible explanations for the insufficient diagnostic performance of magnifying chromoendoscopy. First, some polyps predicted with LC had an unclear surface pattern by magnifying NBI and did not show the typical pit pattern even after chromoagents had been sprayed onto them. Figure 2 illustrates the basis of this reasoning. Second, as endoscopists were unable to obtain clear evaluable images as a result of factors such as colonic peristalsis and movements as a result of breathing and heartbeat, some polyps were diagnosed with LC. In such cases, even additional chromoendoscopy did not yield sufficiently clear images.
In HC cases, the diagnostic performance for both polyps overall and diminutive polyps met the thresholds of the PIVI statement for assessment of histology using endoscopic technology. This suggests that the endoscopists in our study had sufficient expertise and were able to distinguish between HC and LC cases appropriately.18, 19 Although the specificity in HC cases seemed to be much lower than other diagnostic performance parameters, the primary reason was the small number of JNET Type 1 polyps with HC. As we adopted a ‘diagnose-and-leave’ strategy for diminutive polyps predicted with HC, most of the JNET Type 1 polyps with HC in the rectosigmoid colon were not resected.
This study had some limitations. First, the findings of magnifying NBI may have influenced the diagnostic performance of magnifying chromoendoscopy. However, this bias would have been acceptable because our aim was to investigate the additional effect of magnifying chromoendoscopy after magnifying NBI in routine clinical practice. Second, not all polyps were analyzed because of our ‘resect-and-discard’ and ‘diagnose-and-leave’ strategies. However, these strategies were not applied to any of the LC polyps. In any event, it is expected that polyps treated on the basis of these strategies would be diagnosed with good agreement in general. Although such polyps were excluded from our analysis, the diagnostic performance of HC polyps was satisfactory. Third, all of the participating endoscopists had extensive experience of magnifying colonoscopy. It remains to be examined whether non-experts in magnifying endoscopy would be able to achieve similar results with additional magnifying chromoendoscopy. Finally, this clinical trial was carried out at a single institution, and therefore additional multicenter studies will be needed to confirm this result.
In conclusion, this study has shown that polyps diagnosed with LC as neoplastic and non-neoplastic by magnifying NBI on the basis of the JNET classification should be resected and submitted for histopathological examination, regardless of the result of additional magnifying chromoendoscopy.
Conflicts of Interest
Authors declare no conflicts of interest for this article.