Narrow-band imaging (NBI) magnifying endoscopic classification of colorectal tumors proposed by the Japan NBI Expert Team
Abstract
Many clinical studies on narrow-band imaging (NBI) magnifying endoscopy classifications advocated so far in Japan (Sano, Hiroshima, Showa, and Jikei classifications) have reported the usefulness of NBI magnifying endoscopy for qualitative and quantitative diagnosis of colorectal lesions. However, discussions at professional meetings have raised issues such as: (i) the presence of multiple terms for the same or similar findings; (ii) the necessity of including surface patterns in magnifying endoscopic classifications; and (iii) differences in the NBI findings in elevated and superficial lesions. To resolve these problems, the Japan NBI Expert Team (JNET) was constituted with the aim of establishing a universal NBI magnifying endoscopic classification for colorectal tumors (JNET classification) in 2011. Consensus was reached on this classification using the modified Delphi method, and this classification was proposed in June 2014. The JNET classification consists of four categories of vessel and surface pattern (i.e. Types 1, 2A, 2B, and 3). Types 1, 2A, 2B, and 3 are correlated with the histopathological findings of hyperplastic polyp/sessile serrated polyp (SSP), low-grade intramucosal neoplasia, high-grade intramucosal neoplasia/shallow submucosal invasive cancer, and deep submucosal invasive cancer, respectively.
Introduction
Narrow-band imaging (NBI) was initially developed by Sano et al. under the supervision of Dr Shigeaki Yoshida at the National Cancer Center Hospital East in 1999.1, 2 A prototype short-wavelength narrow-band red/green/blue (RGB) filter was successfully created in 2001 (monochrome NBI),1, 2 and the microvascular architecture of the gastrointestinal tract and tumor surface structure were successfully visualized in color using 415- and 540-nm short- and medium-wavelength filters in 2003.3 Subsequently, various improvements, such as noise reduction, light amount adjustment and color adjustment, were made, and OLYMPUS EVIS LUCERA SPECTRUM (Olympus Medical Systems Corp., Tokyo, Japan) was launched in the market as the final mass production model in 2006.
Sano et al. reported the usefulness of observing the pit pattern and the usefulness of vascular classification using NBI in 2004,3 and Sano et al. reported the first classification of the capillary pattern using NBI magnifying colonoscopy in 2006.4 Thereafter, the Magnifying Endoscopy Study Groups of the Ministry of Health, Labour and Welfare (Kudo, Sano, and Inoue groups) discussed the usefulness of NBI classification based on the findings of NBI magnifying endoscopy, which led to the proposal of new classifications (Hiroshima, Showa, and Jikei classifications) based on the capillary pattern classification from several institutions.
Sano, Hiroshima, Showa, and Jikei Classifications Based on the Findings of NBI Magnifying Endoscopy
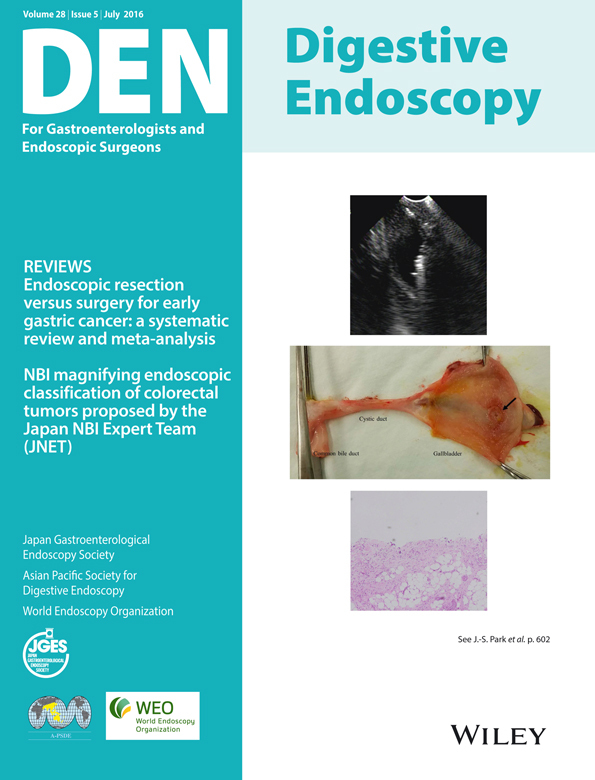
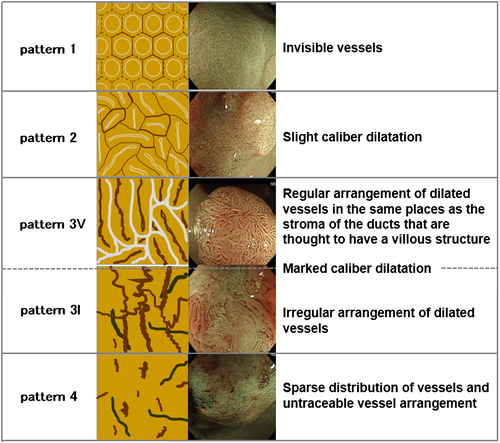
Sano classification
The Sano classification (Fig. 1) was the first published NBI magnifying endoscopic classification, in 2006. This classification is based on the vascular findings. Validation studies have reported its usefulness in qualitative and quantitative diagnosis, its learning curve etc.5-8
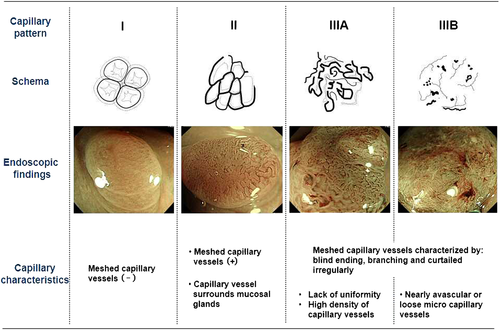
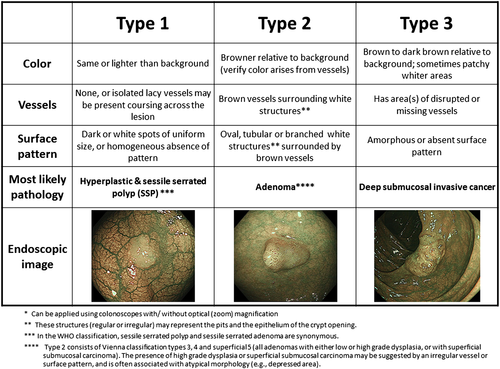
Hiroshima classification
The Hiroshima classification (Fig. 2), published in 2008, is based on the surface pattern in addition to the vascular findings on NBI magnifying endoscopy.9, 10
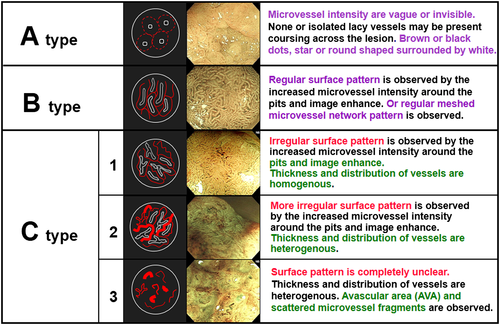
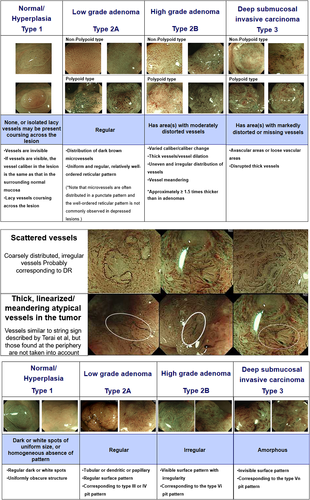
Showa classification
The Showa classification (Fig. 3) was proposed in 2009 as a classification mainly based on the vascular findings on NBI magnifying endoscopy.11
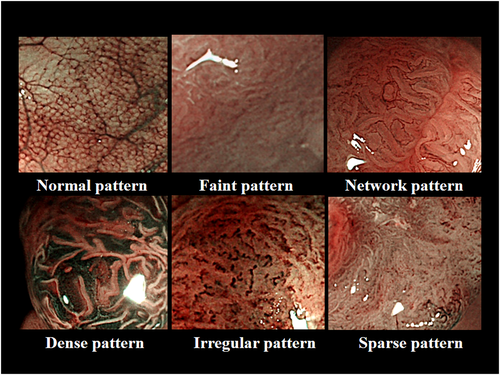
Jikei classification
The Jikei classification (Fig. 4) was also proposed in 2009 as a classification based mainly on the vascular findings on NBI magnifying endoscopy.12
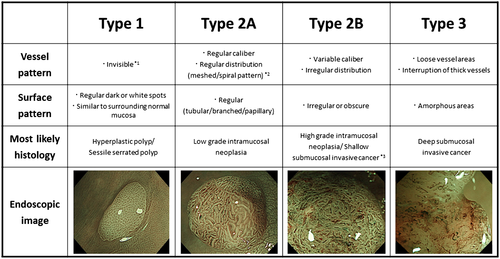
NBI International Colorectal Endoscopic (NICE) Classification Of Tumors
Tanaka et al. constituted the Colon Tumor NBI Interest Group (CTNIG) in 2009, with the aim of creating a simple NBI endoscopic classification of colorectal tumors that can be used internationally. The CTNIG consist of the following six members: Chair, S Tanaka, Hiroshima University (Japan); Y Sano, Sano Hospital (Japan); DK Rex, Indiana University (USA); RM Soetikno, Stanford University (USA); T Ponchon, Edouard Herriot Hospital (France); and BP Saunders, St Mark's Hospital (UK). The CTNIG proposed the NBI International Colorectal Endoscopic (NICE) classification in 2009, which can also be used in assessment using non-magnifying endoscopy, and is based on the color, vessels, and surface pattern on endoscopy (Fig. 5).Naming of the NICE classification was proposed by Sano in London in February 2010 and was approved by the members of the CTNIG. International validation studies of the NICE classification have also proved useful in qualitative and quantitative diagnosis based on non-magnifying endoscopy.13, 14
Clinical Problems in Japan and Some Experts in the West
- Existence of multiple terms for the same or similar magnifying findings.
- Necessity of including the surface patterns in magnifying endoscopic classifications.
- Differences in the NBI magnifying findings in elevated and superficial lesions.
To resolve the aforementioned problems, the necessity of developing a universal classification is discussed.
Universal NBI Magnifying Endoscopic Classification of Colorectal Tumors: Japan NBI Expert Team (JNET) Classification
To establish a universal NBI magnifying endoscopic classification of colorectal tumors, the Japan NBI Expert Team (JNET), consisting of 38 members, mainly specialists in colonoscopy from throughout Japan, was formed within the Research Group of the National Cancer Center Research and Development Fund (Yutaka Saito Group) in 2011.
First, it was necessary to establish common evaluation criteria, and a working group mainly consisting of young but experienced researchers (Shoichi Saito, Yoshiki Wada, Hiroaki Ikematsu, Hiroshi Kawano and Shiro Oka, Chairs; Takahisa Matsuda and Yutaka Saito) from six institutions, including the institution to which the member who first proposed establishment of a classification belonged, was organized to hold discussions. Consequently, normal/hyperplastic lesions/sessile serrated polyp were classified as Type 1, low-grade intramucosal neoplasia including intramucosal cancer with low-grade structural atypia as Type 2A, high-grade intramucosal neoplasia/shallow submucosal invasive cancer as Type 2B, and deep submucosal invasive cancers as Type 3, and a magnifying NBI scale including the vascular and surface patterns was created (Fig 6 ).15
To scientifically evaluate the NBI scale and determine the NBI findings and diagnostic criteria used in the universal classification, a web image interpretation study (UMIN000010292: Multicenter study for developing universal NBI magnifying endoscopic classification of colorectal tumors in Japan, principal investigator: Yasushi Sano) was conducted by 25 specialists in colonoscopy belonging to the JNET in 2013. Twenty-five specialists in colonoscopy evaluated NBI findings and histology with 100 NBI still images on the web. Univariate and multivariate analyses and analysis of the diagnosability from five candidate NBI findings such as: (i) loose vessel areas; (ii) interruption of thick vessels; (iii) scattered vessels; (iv) thick, linearized/meandering atypical vessels in the tumor; and (v) amorphous areas of surface patterns, identified findings (i), (ii) and (v) for the diagnosis of Type 3. In addition, from among five candidate findings such as: (i) variable caliber of vessels; (ii) thick vessels; (iii) irregular distribution of vessels; (iv) vessel meandering; and (v) irregular or obscure surface pattern, findings (i), (iii) and (v) were selected for the diagnosis of Type 2B.
The Yutaka Saito Group meeting on 6 June 2014 reached a consensus on the universal NBI magnifying endoscopic classification of colorectal tumors based on scientific grounds using a modified Delphi method, followed by its proposal by the JNET (Fig. 7).
The JNET classification unifying previous classifications will give us common diagnostic criteria to promote academic progress of NBI. Now we need to standardize the interpretation of each NBI finding through various discussions and validate the JNET classification itself.
Future Perspectives
Fifteen years have passed since the introduction of NBI (14 December 1999), and a consensus was reached on the original Japanese universal NBI magnifying endoscopic classification of colorectal tumors (JNET classification). At present, validation studies for the JNET classification are proposed to be conducted by the Research Group of the National Cancer Center Research and Development Fund (Yutaka Saito Group) and a study group of the Japan Gastroenterological Endoscopy Society (a study group for the standardization and dissemination of the magnifying colonoscopic diagnostic criteria, representative organizer: Takahisa Matsuda). Modifications may be made through these studies, but it should be kept in mind that the classification will be continuously updated by many new findings and innovations in endoscopy. Moreover, it is an urgent task to disseminate this classification in many clinical settings in Japan and to scientifically prove that this is useful in qualitative and quantitative diagnosis, which can determine the therapeutic strategy for colorectal tumors.
Acknowledgement
This study was financially supported, in part, by the National Cancer Center Research and Development Fund (25-A-12) to Dr Saito.
Conflicts of Interest
Authors declare no conflicts of interest for this article.