Evaluation of the effectiveness of color intensity analysis using a second-generation autofluorescence imaging system for diminutive colorectal polyp differentiation
Abstract
Background and Aim
We previously reported the effectiveness of color tone intensity analysis using autofluorescence imaging (AFI) for distinguishing between colorectal neoplastic and non-neoplastic lesions. Moreover, a second-generation AFI system has become commercially available in Japan. In the present study, we assessed the effectiveness of color tone intensity analysis using a second-generation AFI system for evaluating diminutive colorectal lesions.
Methods
We retrospectively reviewed the cases of 35 consecutive patients with 101 diminutive colorectal lesions that were examined using a second-generation AFI system and resected at the Jikei University Hospital. We estimated the mean green-to-red (G/R) ratio – obtained by dividing the green color tone intensity by the red color tone intensity – of the lesions and compared the values of the neoplastic and non-neoplastic lesions. We also assessed the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the AFI system for neoplastic lesion identification.
Results
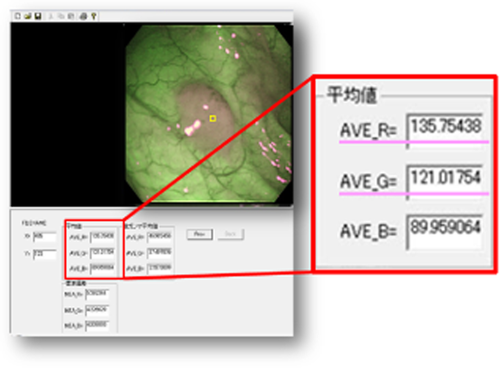
The mean G/R ratios of the non-neoplastic and neoplastic lesions were 1.06 and 0.87, respectively; the mean G/R ratio significantly differed between the neoplastic and non-neoplastic lesions. Using the second-generation AFI system, neoplastic lesions were identified with a sensitivity, specificity, PPV, and NPV of 94.2%, 91.8%, 92.5%, and 93.8%, respectively.
Conclusion
Color intensity analysis of diminutive colorectal polyps using the second generation AFI system could effectively distinguish between neoplastic and non-neoplastic lesions.
Introduction
Early detection and removal of colorectal adenomatous polyps are essential for reducing the mortality rate of colorectal cancer. Although several modalities are currently available for colorectal cancer screening, colonoscopy is considered to be the most effective procedure, as it enables direct visualization and on-site treatment of detected lesions.1, 2 Moreover, accurate endoscopic determination of the histology of colorectal polyps could prevent unnecessary polypectomies, and may enable physicians to make adequate surveillance recommendations. Furthermore, guidelines for real-time endoscopic assessment of the histology of diminutive colorectal polyps have been proposed by The American Society for Gastrointestinal Endoscopy. According to these guidelines, in order to not resect suspected diminutive rectosigmoid hyperplastic polyps, there should be ≥90% negative predictive value (NPV) for adenomatous histology.3 However, a report evaluating real-time optical biopsy analysis of polyps with narrow band imaging (NBI) indicated that only 25% of community-based gastroenterologists assessed polyps with >90% accuracy.4 Thus, an easy and objective method for distinguishing between colorectal neoplastic lesions and non-neoplastic lesions is required.
First- and second-generation AFI systems
First-generation AFI systems (EVIS LUCERA CLV-260SL, EVIS LUCERA CV-260S; Olympus Medical Systems, Tokyo, Japan) have certain technical problems. These include flickering and color splitting in endoscopic images as a result of a slower frame rate compared to white light imaging (WLI). Recently, a second-generation AFI system consisting of light sources (EVIS LUCERA ELITE CLV-290SL; Olympus Medical Systems) and video processors (EVIS LUCERA ELITE CV-290; Olympus Medical Systems) has been developed.
There are two main differences between the first- and second-generation AFI systems. One difference is that the second-generation AFI systems have a brighter lamp that allows for a higher frame rate, even though the overall brightness of endoscopic images is similar to that of the first-generation AFI systems. Therefore, a lesser amount of flickering and color splitting in endoscopic images has been observed. The second major improvement is in the image-processing algorithm, particularly in the noise reduction algorithm, which yields higher resolution images with less noise interference.
AFI systems for the detection of colorectal lesions
The effectiveness of first-generation AFI systems in colorectal polyp detection is still debatable. Several studies support the use of first-generation AFI systems to facilitate the effective detection of colorectal lesions.5-7 However, some studies report that first-generation AFI systems do not have a significant advantage over WLI in the detection of colorectal polyps.8-10
To our knowledge, the effectiveness of novel second-generation AFI systems for the detection of colorectal neoplasia has not been evaluated. However, a recent study reported that better visualization of colorectal neoplasia is achievable by using a second-generation AFI system compared to WLI, which may be useful for less-experienced endoscopists.11
AFI system for differentiation of colorectal lesions
Moriichi et al. reported that the dysplastic grade of lesions is the main factor that affects the fluorescence captured by AFI systems.12 Although this suggests that AFI systems may be useful for differentiating colorectal lesions, the effectiveness of such methodologies, based on the subjective evaluation of the grade of color tone visualization, remains controversial.9, 10, 13-15 We have previously reported the effectiveness of methods using first-generation AFI systems and software that enables the immediate calculation of color tone intensity for distinguishing between neoplastic and non-neoplastic colorectal lesions.16, 17 In our previous retrospective study of first-generation AFI systems, the sensitivity, specificity, NPV, and positive predictive value (PPV) for differentiating neoplastic lesions were found to be 98.8%, 86.4%, 96.4%, and 95.0%, respectively.16 Furthermore, in a prospective study on first-generation AFI systems, we reported values of 94.7%, 88.9%, 95.9%, and 85.2% for sensitivity, specificity, NPV, and PPV, in the differentiation of neoplastic lesions.17
Methods
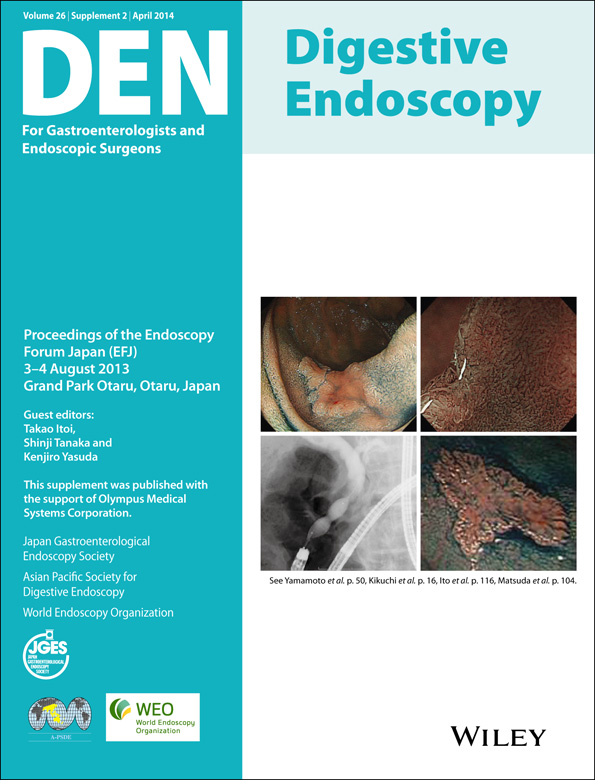
We retrospectively evaluated the cases of 35 consecutive patients with 101 diminutive colorectal lesions (≤5 mm in size) that were examined using a second-generation AFI system and resected at the Jikei University Hospital from December 2012 to April 2013 (Fig. 1).
Endoscopic image of diminutive colorectal lesions using novel light sources (EVIS LUCERA ELITE CLV-290SL; Olympus Medical Systems, Tokyo, Japan) and novel video processors (EVIS LUCERA ELITE CV-290; Olympus Medical Systems). Endoscopic images of a diminutive adenoma. (A) White light imaging; (B) narrow band imaging; and (C) autofluorescence imaging. Endoscopic images of a diminutive hyperplastic polyp. (D) White light imaging; (E) narrow band imaging; and (F) autofluorescence imaging.
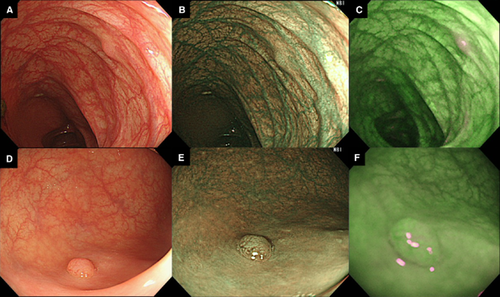
The regions of interest (ROI) in the AFI images were considered to be at the center of the diminutive lesion (Fig. 2). Endoscopists, who were blinded to the results of the pathological assessments, retrospectively conducted color intensity analysis for the ROI and estimated green-to-red (G/R) ratios. The mean G/R ratio was estimated by dividing the green color tone intensity values by the red color tone intensity values. Color tone intensity analysis was carried out with still images of the colorectal lesions using software developed by our group in collaboration with Olympus Medical Systems, Tokyo, Japan.
User interface of the software used for color tone analysis. The region of interest was chosen using the cursor (small yellow square on endoscopic image). The color tone intensities (large red square) are automatically analyzed and the green-to-red (G/R) ratio – estimated by dividing the green color tone intensity (AVE_G) by the red color tone intensity (AVE_R) – can be calculated.
Thereafter, we retrospectively reviewed the patients' electronic medical records to determine the endoscopic diagnoses. In these records, the differentiation of colorectal lesions into non-neoplastic and neoplastic lesions was based on the findings of WLI and NBI. In addition, the sensitivity, specificity, PPV, and NPV were estimated.
Results
The mean G/R ratios for non-neoplastic and neoplastic lesions obtained using a second-generation AFI system were 1.06 and 0.87, respectively; a significant difference in the mean G/R ratio was noted between these two groups (Fig. 3). Moreover, the area under the receiver operating characteristic (ROC) curve for the sensitivity and 1 – specificity of the G/R ratio in distinguishing between non-neoplastic and neoplastic lesions was 0.978. When a G/R ratio cut-off value of <0.95 was applied, neoplastic lesions were identified with a sensitivity, specificity, PPV, and NPV of 94.2%, 91.8%, 92.5%, and 93.8%, respectively (Fig. 4). According to medical records, endoscopists were able to distinguish neoplastic from non-neoplastic lesions based on WLI and NBI findings, with a sensitivity, specificity, PPV, and NPV of 94.2%, 93.9%, 94.2%, and 93.9%, respectively.
Distribution of the green-to-red (G/R) ratios. A significant difference between the mean G/R ratios in non-neoplastic and neoplastic lesions is observed (P < 0.001).
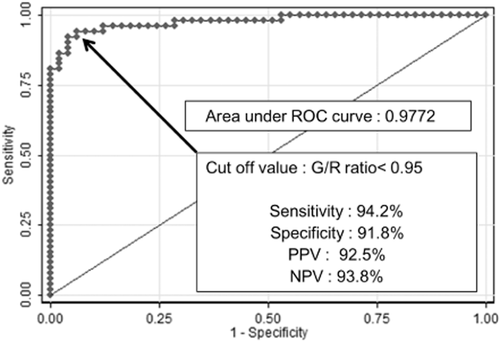
Receiver operating characteristic (ROC) curve analysis. For discriminating between hyperplastic polyps and neoplastic lesions, the area under the receiver operating characteristic curve (AUC) was 0.9772. G/R, green-to-red ratio; NPV, negative predictive value; PPV, positive predictive value.
Discussion
This present study demonstrates the utility of second-generation AFI systems and color tone intensity analysis for effective differentiation of diminutive colorectal lesions. Furthermore, as neoplastic lesions were identified with an NPV of ≥90%, this methodology satisfies the criteria proposed by the American Society for Gastrointestinal Endoscopy.3 Thus, color intensity analysis of diminutive colorectal polyps using second-generation AFI systems could be an effective modality for endoscopic assessment of the histology of diminutive colorectal polyps.
Conflict of Interests
Authors declare no conflict of interests for this article.