Pneumocystis jiroveci in solid organ transplantation: Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice
Corresponding Author
Jay A. Fishman
Medicine, Transplant Infectious Diseases and Transplant Center, Massachusetts General Hospital and Harvard Medical School, Boston, Massachusetts
Correspondence
Jay A. Fishman, MGH Transplant Center WH510A, 55 Fruit Street, Boston, MA 02114.
Email: [email protected]
Search for more papers by this authorHayley Gans
Medicine, Pediatric Infectious Diseases Program for Immunocompromised Hosts, Stanford University, Stanford, California
Search for more papers by this authorthe AST Infectious Diseases Community of Practice
Search for more papers by this authorCorresponding Author
Jay A. Fishman
Medicine, Transplant Infectious Diseases and Transplant Center, Massachusetts General Hospital and Harvard Medical School, Boston, Massachusetts
Correspondence
Jay A. Fishman, MGH Transplant Center WH510A, 55 Fruit Street, Boston, MA 02114.
Email: [email protected]
Search for more papers by this authorHayley Gans
Medicine, Pediatric Infectious Diseases Program for Immunocompromised Hosts, Stanford University, Stanford, California
Search for more papers by this authorthe AST Infectious Diseases Community of Practice
Search for more papers by this authorAbstract
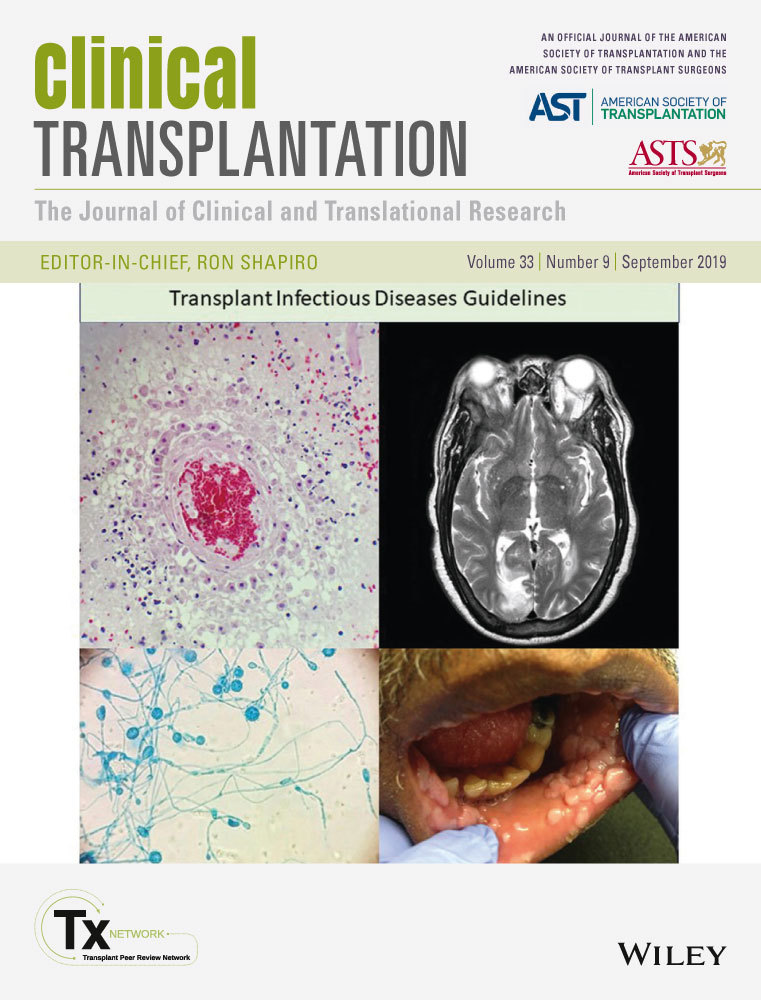
These updated guidelines from the Infectious Diseases Community of Practice of the American Society of Transplantation review the diagnosis, prevention, and management of Pneumocystis jiroveci fungal infection transplant recipients. Pneumonia (PJP) may develop via airborne transmission or reactivation of prior infection. Nosocomial clusters of infection have been described among transplant recipients. PJP should not occur during prophylaxis with trimethoprim-sulfamethoxazole (TMP-SMX). Without prophylaxis, PJP risk is greatest in the first 6 months after organ transplantation but may develop later. Risk factors include low lymphocyte counts, cytomegalovirus infection (CMV), hypogammaglobulinemia, treated graft rejection or corticosteroids, and advancing patient age (>65). Presentation typically includes fever, dyspnea with hypoxemia, and cough. Chest radiographic patterns generally reveal diffuse interstitial processes best seen by CT scans. Patients generally have PO2 < 60 mm Hg, elevated serum lactic dehydrogenase (LDH), and elevated serum (1 → 3) β-d-glucan assay. Specific diagnosis uses respiratory specimens with direct immunofluorescent staining; invasive procedures may be required. Quantitative PCR is a useful adjunct to diagnosis. TMP-SMX is the drug of choice for therapy; drug allergy should be documented before resorting to alternative therapies. Adjunctive corticosteroids may be useful early. Routine PJP prophylaxis is recommended for at least 6-12 months post–transplant, preferably with TMP-SMX.
CONFLICT OF INTEREST
None.
REFERENCES
- 1Cordonnier C, Cesaro S, Maschmeyer G, et al. Pneumocystis jirovecii pneumonia: still a concern in patients with haematological malignancies and stem cell transplant recipients. J Antimicrob Chemother. 2016; 71: 2379-2385.
- 2Gryzan S, Paradis IL, Zeevi A, et al. Unexpectedly high incidence of Pneumocystis carinii infection after lung-heart transplantation. Implications for lung defense and allograft survival. Am Rev Respir Dis. 1988; 137: 1268-1274.
- 3Lufft V, Kliem V, Behrend M, Pichlmayr R, Koch KM, Brunkhorst R. Incidence of Pneumocystis carinii pneumonia after renal transplantation. Impact of immunosuppression. Transplantation. 1996; 62: 421-423.
- 4Maini R, Henderson KL, Sheridan EA, et al. Increasing Pneumocystis pneumonia, England, UK, 2000r-2010. Emerg Infect Dis. 2013; 19: 386-392.
- 5Rodriguez M, Fishman JA. Prevention of infection due to Pneumocystis spp. in human immunodeficiency virus-negative immunocompromised patients. Clin Microbiol Rev. 2004; 17: 770-782.
- 6Vanek J, Jirovec O. [Parasitic pneumonia. Interstitial plasma cell pneumonia of premature, caused by pneumocystis Carinii]. Zentralbl Bakteriol Parasitenkd Infektionskr Hyg. 1952; 158: 120-127.
- 7Stringer JR, Cushion MT, Wakefield AE. New nomenclature for the genus Pneumocystis. Proceedings of the Seventh International Workshops on Opportunistic Protists. J Eukaryot Microbiol. 2001; 48: 184s-189s.
10.1111/j.1550-7408.2001.tb00512.x Google Scholar
- 8Walzer PD, Linke MJ. A comparison of the antigenic characteristics of rat and human Pneumocystis carinii by immunoblotting. J Immunol. 1987; 138: 2257-2265.
- 9Ma L, Chen Z, Huang DW, et al. Genome analysis of three Pneumocystis species reveals adaptation mechanisms to life exclusively in mammalian hosts. Nat Commun. 2016; 7: 10740.
- 10de Boer M, Bruijnesteijn van Coppenraet L, Gaasbeek A, et al. An outbreak of Pneumocystis jiroveci pneumonia with 1 predominant genotype among renal transplant recipients: interhuman transmission or a common environmental source? Clin Infect Dis. 2007; 44: 1143-1149.
- 11Pifer LL, Hughes WT, Stagno S, Woods D. Pneumocystis carinii infection: evidence for high prevalence in normal and immunosuppressed children. Pediatrics. 1978; 61: 35-41.
- 12Kovacs JA, Gill VJ, Meshnick S, Masur H. New insights into transmission, diagnosis, and drug treatment of Pneumocystis carinii pneumonia. JAMA. 2001; 286: 2450-2460.
- 13Schmoldt S, Schuhegger R, Wendler T, et al. Molecular evidence of nosocomial Pneumocystis jirovecii transmission among 16 patients after kidney transplantation. J Clin Microbiol. 2008; 46: 966-971.
- 14Hocker B, Wendt C, Nahimana A, Tonshoff B, Hauser PM. Molecular evidence of Pneumocystis transmission in pediatric transplant unit. Emerg Infect Dis. 2005; 11: 330-332.
- 15Choukri F, Menotti J, Sarfati C, et al. Quantification and spread of Pneumocystis jirovecii in the surrounding air of patients with Pneumocystis pneumonia. Clin Infect Dis. 2010; 51: 259-265.
- 16Rostved AA, Sassi M, Kurtzhals J, et al. Outbreak of pneumocystis pneumonia in renal and liver transplant patients caused by genotypically distinct strains of Pneumocystis jirovecii. Transplantation. 2013; 96: 834-842.
- 17Sassi M, Ripamonti C, Mueller NJ, et al. Outbreaks of Pneumocystis pneumonia in 2 renal transplant centers linked to a single strain of Pneumocystis: implications for transmission and virulence. Clin Infect Dis. 2012; 54: 1437-1444.
- 18Veronese G, Ammirati E, Moioli MC, et al. Single-center outbreak of Pneumocystis jirovecii pneumonia in heart transplant recipients. Transpl Infect Dis. 2018; 20: e12880.
- 19Phipps LM, Chen S-A, Kable K, et al. Nosocomial Pneumocystis jirovecii pneumonia: lessons from a cluster in kidney transplant recipients. Transplantation. 2011; 92: 1327-1334.
- 20Fishman JA. Prevention of infection due to Pneumocystis carinii. Antimicrob Agents Chemother. 1998; 42: 995-1004.
- 21Stern M, Hirsch H, Cusini A, et al. Cytomegalovirus serology and replication remain associated with solid organ graft rejection and graft loss in the era of prophylactic treatment. Transplantation. 2014; 98: 1013-1018.
- 22Hosseini-Moghaddam SM, Shokoohi M, Singh G, et al. A multi-center case-control study of the effect of acute rejection and cytomegalovirus infection on Pneumocystis pneumonia (PCP) in solid organ transplant recipients. Clin Infect Dis. 2018.
- 23Iriart X, Belval TC, Fillaux J, et al. Risk factors of Pneumocystis pneumonia in solid organ recipients in the era of the common use of post transplantation prophylaxis. Am J Transplant. 2015; 15: 190-199.
- 24Yale SH, Limper AH. Pneumocystis carinii pneumonia in patients without acquired immunodeficiency syndrome: associated illness and prior corticosteroid therapy. Mayo Clin Proc. 1996; 71: 5-13.
- 25Roux A, Canet E, Valade S, et al. Pneumocystis jirovecii pneumonia in patients with or without AIDS. France. Emerg Infect Dis. 2014; 20: 1490-1497.
- 26Gryzan S, Paradis IL, Hardesty RL, Griffith BP, Dauber JH. Bronchoalveolar lavage in heart-lung transplantation. J Heart Transplant. 1985; 4: 414-416.
- 27Kovacs JA, Hiemenz JW, Macher AM, et al. Pneumocystis carinii pneumonia: a comparison between patients with the acquired immunodeficiency syndrome and patients with other immunodeficiencies. Ann Intern Med. 1984; 100: 663-671.
- 28Fujii T, Iwamoto A, Nakamura T, Iwamoto A, Iwamoto A, Iwamoto A. Pneumocystis pneumonia in patients with HIV infection: clinical manifestations, laboratory findings, and radiological features. J Infect Chemother. 2007; 13: 1-7.
- 29Chou CW, Chao HS, Lin FC, Tsai HC, Yuan WH, Chang SC. Clinical usefulness of HRCT in assessing the severity of Pneumocystis jirovecii pneumonia: A Cross-sectional Study. Medicine (Baltimore). 2015; 94: e768.
- 30Vogel MN, Vatlach M, Weissgerber P, et al. HRCT-features of Pneumocystis jiroveci pneumonia and their evolution before and after treatment in non-HIV immunocompromised patients. Eur J Radiol. 2012; 81: 1315-1320.
- 31Vogel MN, Weissgerber P, Goeppert B, et al. Accuracy of serum LDH elevation for the diagnosis of Pneumocystis jiroveci pneumonia. Swiss Med Wkly. 2011; 141: w13184.
- 32 Pneumonia NIoH-UoCEPfCaATfP. Consensus statement on the use of corticosteroids as adjunctive therapy for pneumocystis pneumonia in the acquired immunodeficiency syndrome. The National Institutes of Health-University of California Expert Panel for Corticosteroids as Adjunctive Therapy for Pneumocystis pneumonia [see comments]. N Engl J Med. 1990; 323: 1500-1504.
- 33Akamatsu N, Sugawara Y, Kaneko J, Tamura S, Makuuchi M. Preemptive treatment of fungal infection based on plasma (1 –> 3)beta-D-glucan levels after liver transplantation. Infection. 2007; 35: 346-351.
- 34Costa JM, Botterel F, Cabaret O, Foulet F, Cordonnier C, Bretagne S. Association between circulating DNA, serum (1->3)-beta-D-glucan, and pulmonary fungal burden in Pneumocystis pneumonia. Clin Infect Dis. 2012; 55: e5-8.
- 35Karageorgopoulos DE, Qu JM, Korbila IP, Zhu YG, Vasileiou VA, Falagas ME. Accuracy of beta-D-glucan for the diagnosis of Pneumocystis jirovecii pneumonia: a meta-analysis. Clin Microbiol Infect. 2013; 19: 39-49.
- 36Damiani C, Le Gal S, Goin N, et al. Usefulness of (1,3) ss-D-glucan detection in bronchoalveolar lavage samples in Pneumocystis pneumonia and Pneumocystis pulmonary colonization. J Mycol Med. 2015; 25: 36-43.
- 37Tasaka S, Kobayashi S, Yagi K, et al. Serum (1 –> 3) beta-D-glucan assay for discrimination between Pneumocystis jiroveci pneumonia and colonization. J Infect Chemother. 2014; 20: 678-681.
- 38Procop GW, Haddad S, Quinn J, et al. Detection of Pneumocystis jiroveci in respiratory specimens by four staining methods. J Clin Microbiol. 2004; 42: 3333-3335.
- 39Cregan P, Yamamoto A, Lum A, VanDerHeide T, MacDonald M, Pulliam L. Comparison of four methods for rapid detection of Pneumocystis carinii in respiratory specimens. J Clin Microbiol. 1990; 28: 2432-2436.
- 40Damiani C, Le Gal S, Da Costa C, Virmaux M, Nevez G, Totet A. Combined quantification of pulmonary Pneumocystis jirovecii DNA and serum (1->3)-beta-D-glucan for differential diagnosis of pneumocystis pneumonia and Pneumocystis colonization. J Clin Microbiol. 2013; 51: 3380-3388.
- 41Fauchier T, Hasseine L, Gari-Toussaint M, Casanova V, Marty PM, Pomares C. Detection of Pneumocystis jirovecii by Quantitative PCR to differentiate colonization and pneumonia in immunocompromised HIV-positive and HIV-negative patients. J Clin Microbiol. 2016; 54: 1487-1495.
- 42Esteves F, de Sousa B, Calderón EJ, et al. Multicentre study highlighting clinical relevance of new high-throughput methodologies in molecular epidemiology of Pneumocystis jirovecii pneumonia. Clin Microbiol Infect. 2016; 22(566): e9-e19.
- 43Alanio A, Hauser PM, Lagrou K, et al. ECIL guidelines for the diagnosis of Pneumocystis jirovecii pneumonia in patients with haematological malignancies and stem cell transplant recipients. J Antimicrob Chemother. 2016; 71: 2386-2396.
- 44Botterel F, Cabaret O, Foulet F, Cordonnier C, Costa J-M, Bretagne S. Clinical significance of quantifying Pneumocystis jirovecii DNA by Using Real-Time PCR in bronchoalveolar lavage fluid from immunocompromised patients. J Clin Microbiol. 2012; 50: 227-231.
- 45Rohner P, Jacomo V, Studer R, Schrenzel J, Graf JD. Detection of Pneumocystis jirovecii by two staining methods and two quantitative PCR assays. Infection. 2009; 37: 261-265.
- 46Fan LC, Lu HW, Cheng KB, Li HP, Xu JF. Evaluation of PCR in bronchoalveolar lavage fluid for diagnosis of Pneumocystis jirovecii pneumonia: a bivariate meta-analysis and systematic review. PLoS ONE. 2013; 8: e73099.
- 47Lu Y, Ling G, Qiang C, et al. PCR Diagnosis of Pneumocystis pneumonia: a Bivariate Meta-Analysis. J Clin Microbiol. 2011; 49: 4361-4363.
- 48Montesinos I, Delforge M-L, Ajjaham F, et al. Evaluation of a new commercial real-time PCR assay for diagnosis of Pneumocystis jirovecii pneumonia and identification of dihydropteroate synthase (DHPS) mutations. Diagn Microbiol Infect Dis. 2017; 87: 32-36.
- 49Bollée G, Sarfati C, Thiéry G, et al. Clinical picture of Pneumocystis jiroveci pneumonia in cancer patients. Chest. 2007; 132: 1305-1310.
- 50Pareja JG, Garland R, Koziel H. Use of adjunctive corticosteroids in severe adult non-HIV Pneumocystis carinii pneumonia. Chest. 1998; 113: 1215-1224.
- 51Fishman JA. Prevention of infection caused by Pneumocystis carinii in transplant recipients. Clin Infect Dis. 2001; 33: 1397-1405.
- 52Fillatre P, Decaux O, Jouneau S, et al. Incidence of Pneumocystis jiroveci pneumonia among groups at risk in HIV-negative patients. Am J Med. 2014; 127(1242): e11-e17.
- 53de Boer MG, Kroon FP, le Cessie S, de Fijter JW, van Dissel JT. Risk factors for Pneumocystis jirovecii pneumonia in kidney transplant recipients and appraisal of strategies for selective use of chemoprophylaxis. Transpl Infect Dis. 2011; 13: 559-569.
- 54Kasiske BL, Zeier MG, Chapman JR, et al. KDIGO clinical practice guideline for the care of kidney transplant recipients: a summary. Kidney Int. 2010; 77: 299-311.
- 55Green H, Paul M, Vidal L, Leibovici L. Prophylaxis for Pneumocystis pneumonia (PCP) in non-HIV immunocompromised patients. Cochrane Database Syst Rev. 2007: 3; CD005590.
- 56Gordon S, LaRosa S, Kalmadi S, et al. Should prophylaxis for Pneumocystis carinii pneumonia in solid organ transplant recipients ever be discontinued? Clin Infect Dis. 1999; 28: 240-246.
- 57Ioannidis JP, Cappelleri JC, Skolnik PR, Lau J, Sacks HS. A meta-analysis of the relative efficacy and toxicity of Pneumocystis carinii prophylactic regimens. Arch Intern Med. 1996; 156: 177-188.
- 58Lee I, Barton TD, Goral S, et al. Complications related to dapsone use for Pneumocystis jirovecii pneumonia prophylaxis in solid organ transplant recipients. Am J Transplant. 2005; 5: 2791-2795.
- 59Argy N, Le Gal S, Coppée R, et al. Pneumocystis cytochrome b mutants associated with atovaquone prophylaxis failure as the cause of pneumocystis infection outbreak among heart transplant recipients. Clin Infect Dis. 2018; 67: 913-919.
- 60Thomas CF Jr, Limper AH. Current insights into the biology and pathogenesis of Pneumocystis pneumonia. Nat Rev Microbiol. 2007; 5: 298-308.
- 61Le Gal S, Damiani C, Rouille A, et al. A cluster of Pneumocystis infections among renal transplant recipients: molecular evidence of colonized patients as potential infectious sources of Pneumocystis jirovecii. Clin Infect Dis. 2012; 54: e62-71.
- 62Bartlett MS, Vermund SH, Jacobs R, et al. Detection of Pneumocystis carinii DNA in air samples: likely environmental risk to susceptible persons. J Clin Microbiol. 1997; 35: 2511-2513.
- 63Olsson M, Lidman C, Latouche S, et al. Identification of Pneumocystis carinii f. sp. hominis gene sequences in filtered air in hospital environments. J Clin Microbiol. 1998; 36: 1737-1740.
- 64Gianella S, Haeberli L, Joos B, et al. Molecular evidence of interhuman transmission in an outbreak of Pneumocystis jirovecii pneumonia among renal transplant recipients. Transpl Infect Dis. 2010; 12: 1-10.
- 65Urabe N, Ishii Y, Hyodo Y, et al. Molecular epidemiologic analysis of a Pneumocystis pneumonia outbreak among renal transplant patients. Clin Microbiol Infect. 2016; 22: 365-371.
- 66Edman JC, Kovacs JA, Masur H, Santi DV, Elwood HJ, Sogin ML. Ribosomal RNA sequence shows Pneumocystis carinii to be a member of the fungi. Nature. 1988; 334: 519-522.
- 67Lee CH, Lu JJ, Bartlett MS, et al. Nucleotide sequence variation in Pneumocystis carinii strains that infect humans. J Clin Microbiol. 1993; 31: 754-757.
- 68Liu Y, Rocourt M, Pan S, Liu C, Leibowitz MJ. Sequence and variability of the 5.8S and 26S rRNA genes of Pneumocystis carinii. Nucleic Acids Res. 1992; 20: 3763-3772.
- 69Stringer SL, Hudson K, Blase MA, Walzer PD, Cushion MT, Stringer JR. Sequence from ribosomal RNA of Pneumocystis carinii compared to those of four fungi suggests an ascomycetous affinity. J Protozoo. 1989; 36: 14S-S16.
- 70Fishman JA. Cross-reactive antigens of the rat and human Pneumocystis carinii. J Protozool. 1989; 36: 66S-S67.
- 71Fishman JA, Samia JA, Fuglestad J, Rose RM. The effects of extracellular matrix (ECM) proteins on the attachment of Pneumocystis carinii to lung cell lines in vitro. J Protozool. 1991; 38: 34S-S37.
- 72Furlong ST, Samia JA, Rose RM, Fishman JA. Phytosterols are present in Pneumocystis carinii. Antimicrob Agents Chemother. 1994; 38: 2534-2540.
- 73Garvy BA. Overcoming hurdles to development of a vaccine against Pneumocystis jirovecii. Infect Immun. 2017; 85(4): e00035-e00017. https://doi.org/10.1128/IAI.00035-17
- 74Byrd JC, Hargis JB, Kester KE, Hospenthal DR, Knutson SW, Diehl LF. Opportunistic pulmonary infections with fludarabine in previously treated patients with low-grade lymphoid malignancies: a role for Pneumocystis carinii pneumonia prophylaxis. Am J Hematol. 1995; 49: 135-142.
- 75Sepkowitz K, Schluger N, Godwin T, Armstrong D, Cerami A, Bucala R. DNA amplification in experimental pneumocystosis: characterization of serum Pneumocystis carinii DNA and potential P. carinii carrier states. J Infect Dis. 1993; 168: 421-426.
- 76Fishman JA. Infection in solid-organ transplant recipients. N Engl J Med. 2007; 357: 2601-2614.
- 77Martin SI, Marty FM, Fiumara K, Treon SP, Gribben JG, Baden LR. Infectious complications associated with alemtuzumab use for lymphoproliferative disorders. Clin Infect Dis. 2006; 43: 16-24.
- 78Oz HS, Hughes WT. Novel anti-Pneumocystis carinii effects of the immunosuppressant mycophenolate mofetil in contrast to provocative effects of tacrolimus, sirolimus, and dexamethasone. J Infect Dis. 1997; 175: 901-904.
- 79Azevedo LS, Castro MC, Paula FJ, Ianhez LE, David-Neto E. Mycophenolate mofetil may protect against Pneumocystis carinii pneumonia in renal transplanted patients. Rev Inst Med Trop Sao Paulo. 2005; 47: 143-145.
- 80Hardy AM, Wajszczuk CP, Suffredini AF, Hakala TR, Ho M. Pneumocystis carinii pneumonia in renal-transplant recipients treated with cyclosporine and steroids. J Infect Dis. 1984; 149: 143-147.
- 81Morelon E, Stern M, Kreis H. Interstitial pneumonitis associated with sirolimus therapy in renal-transplant recipients. N Engl J Med. 2000; 343: 225-226.
- 82Munoz P, Munoz RM, Palomo J, Rodriguez-Creixems M, Munoz R, Bouza E. Pneumocystis carinii infection in heart transplant recipients. Efficacy of a weekend prophylaxis schedule. Medicine (Baltimore). 1997; 76: 415-422.
- 83Arend SM, Westendorp R, Kroon FP, et al. Rejection treatment and cytomegalovirus infection as risk factors for Pneumocystis carinii pneumonia in renal transplant recipients. Clin Infect Dis. 1996; 22: 920-925.
- 84Lyytikainen O, Ruutu T, Volin L, et al. Late onset Pneumocystis carinii pneumonia following allogeneic bone marrow transplantation. Bone Marrow Transplant. 1996; 17: 1057-1059.
- 85Masur H, Ognibene FP, Yarchoan R, et al. CD4 counts as predictors of opportunistic pneumonias in human immunodeficiency virus (HIV) infection. Ann Intern Med. 1989; 111: 223-231.
- 86Messiaen PE, Cuyx S, Dejagere T, van der Hilst JC. The role of CD4- cell count as discriminatory measure to guide chemoprophylaxis against Pneumocystis jirovecii pneumonia in human immunodeficiency virus-negative immunocompromised patients: A systematic review. Transpl Infect Dis. 2017; 19: e12651.
- 87Werbel WA, Ison MG, Angarone MP, Yang A, Stosor V. Lymphopenia is associated with late onset Pneumocystis jirovecii pneumonia in solid organ transplantation. Transpl Infect Dis. 2018; 20: e12876.
- 88Castagnola E, Dini G, Lanino E, et al. CD4 lymphocyte count in a patient with P. carinii pneumonia after autologous bone marrow transplantation. Bone Marrow Transplant. 1995; 15: 977-978.
- 89Sepkowitz KA. Pneumocystis carinii pneumonia among patients with neoplastic disease. Semin Respir Infect. 1992; 7: 114-121.
- 90Mansharamani NG, Balachandran D, Vernovsky I, Garland R, Koziel H. Peripheral blood CD4+ T-lymphocyte counts during Pneumocystis carinii pneumonia in immunocompromised patients without HIV infection. Chest. 2000; 118: 712-720.
- 91Stover DE, Zaman MB, Hajdu SI, Lange M, Gold J, Armstrong D. Bronchoalveolar lavage in the diagnosis of diffuse pulmonary infiltrates in the immunosuppressed host. Ann Intern Med. 1984; 101: 1-7.
- 92Bondoc AY, White DA. Granulomatous Pneumocystis carinii pneumonia in patients with malignancy. Thorax. 2002; 57: 435-437.
- 93Studemeister A, Dass S. A patient with dyspnea, cough, and fever. Clin Infect Dis. 2006; 43(1461-2): 90-91.
- 94LaRocque RC, Katz JT, Perruzzi P, Baden LR. The utility of sputum induction for diagnosis of Pneumocystis pneumonia in immunocompromised patients without human immunodeficiency virus. Clin Infect Dis. 2003; 37: 1380-1383.
- 95Kovacs JA, Ng VL, Masur H, et al. Diagnosis of Pneumocystis carinii pneumonia: improved detection in sputum with use of monoclonal antibodies. N Engl J Med. 1988; 318: 589-593.
- 96Thomas CF Jr, Limper AH. Pneumocystis pneumonia: clinical presentation and diagnosis in patients with and without acquired immune deficiency syndrome. Semin Respir Infect. 1998; 13: 289-295.
- 97Sasso M, Chastang-Dumas E, Bastide S, et al. Performances of Four Real-Time PCR Assays for diagnosis of Pneumocystis jirovecii Pneumonia. J Clin Microbiol. 2016; 54: 625-630.
- 98Esteves F, Calé SS, Badura R, et al. Diagnosis of Pneumocystis pneumonia: evaluation of four serologic biomarkers. Clin Microbiol Infect. 2015; 21(379): e1-10.
- 99Fishman JA. Treatment of infection due to Pneumocystis carinii. Antimicrob Agents Chemother. 1998; 42: 1309-1314.
- 100Schmatz DM, Romancheck MA, Pittarelli LA, et al. Treatment of Pneumocystis carinii pneumonia with 1,3-beta-glucan synthesis inhibitors. Proc Natl Acad Sci USA. 1990; 87: 5950-5954.
- 101Powles MA, Liberator P, Anderson J, et al. Efficacy of MK-991 (L-743,872), a semisynthetic pneumocandin, in murine models of Pneumocystis carinii. Antimicrob Agents Chemother. 1998; 42: 1985-1989.
- 102Annaloro C, Della Volpe A, Usardi P, Lambertenghi DG. Caspofungin treatment of Pneumocystis pneumonia during conditioning for bone marrow transplantation. Eur J Clin Microbiol Infect Dis. 2006; 25: 52-54.
- 103Utili R, Durante-Mangoni E, Basilico C, Mattei A, Ragone E, Grossi P. Efficacy of caspofungin addition to trimethoprim-sulfamethoxazole treatment for severe pneumocystis pneumonia in solid organ transplant recipients. Transplantation. 2007; 84: 685-688.
- 104Mandujano JF, D'Souza NB, Nelson S, Summer WR, Beckerman RC, Shellito JE. Granulocyte-macrophage colony stimulating factor and Pneumocystis carinii pneumonia in mice. Am J Respir Crit Care Med. 1995; 151: 1233-1238.
- 105Hughes WT. Use of dapsone in the prevention and treatment of Pneumocystis carinii pneumonia: a review. Clin Infect Dis. 1998; 27: 191-204.
- 106El-Sadr WM, Murphy RL, Yurik TM, et al. Atovaquone compared with dapsone for the prevention of Pneumocystis carinii pneumonia in patients with HIV infection who cannot tolerate trimethoprim, sulfonamides, or both. Community Program for Clinical Research on AIDS and the AIDS Clinical Trials Group. N Engl J Med. 1998; 339: 1889-1895.
- 107Rodriguez M, Sifri CD, Fishman JA. Failure of low-dose atovaquone prophylaxis against Pneumocystis jiroveci infection in transplant recipients. Clin Infect Dis. 2004; 38: e76-e78.
- 108Barber BA, Pegram PS, High KP. Clindamycin/primaquine as prophylaxis for Pneumocystis carinii pneumonia. Clin Infect Dis. 1996; 23: 718-722.