Single-cell analysis identified lung progenitor cells in COVID-19 patients
Zixian Zhao, Yu Zhao, and Yueqing Zhou contributed equally to this work.
Abstract
Objectives
The high mortality of severe 2019 novel coronavirus disease (COVID-19) cases is mainly caused by acute respiratory distress syndrome (ARDS), which is characterized by increased permeability of the alveolar epithelial barriers, pulmonary oedema and consequently inflammatory tissue damage. Some but not all patients showed full functional recovery after the devastating lung damage, and so far there is little knowledge about the lung repair process. We focused on crucial roles of lung progenitor cells in alveolar cell regeneration and epithelial barrier re-establishment and aimed to uncover a possible mechanism of lung repair after severe SARS-CoV-2 infection.
Materials and methods
Bronchoalveolar lavage fluid (BALF) of COVID-19 patients was analysed by single-cell RNA-sequencing (scRNA-seq). Transplantation of a single KRT5+ cell-derived cell population into damaged mouse lung and time-course scRNA-seq analysis was performed.
Results
In severe (or critical) COVID-19 patients, there is a remarkable expansion of TM4SF1+ and KRT5+ lung progenitor cells. The two distinct populations of progenitor cells could play crucial roles in alveolar cell regeneration and epithelial barrier re-establishment, respectively. The transplanted KRT5+ progenitors could long-term engraft into host lung and differentiate into HOPX+ OCLN+ alveolar barrier cell which restored the epithelial barrier and efficiently prevented inflammatory cell infiltration.
Conclusions
This work uncovered the mechanism by which various lung progenitor cells work in concert to prevent and replenish alveoli loss post-severe SARS-CoV-2 infection.
1 INTRODUCTION
COVID-19 caused by SARS-CoV-2 virus infection is the major health concern worldwide. Pathological studies of COVID-19 post-mortem lungs have shown that the effect of mild virus infection is limited in upper airway and had little influence on the lung tissue integrity. However, severe virus infection leads to diffuse alveolar damage (DAD) characterized apoptosis, desquamation of alveolar epithelial cells and infiltration of inflammatory cells into alveolar cavity, which could eventually lead to hypoxaemia, pulmonary tissue fibrosis and death of patients. Some but not all patients showed full functional recovery after the devastating lung damage, and so far there is little knowledge about the lung repair process.1 Hyperplasia of type II alveolar cells (ATII) was also noted in most cases, which could suggest an undergoing regenerative process mediated by ATII lung progenitor cells.2-5
Recent animal studies demonstrated that the existence of multiple stem/progenitor populations in lung which have a potent effect to ameliorate pulmonary infection as well as inflammation and regenerate damaged bronchial and alveolar tissues. Previous reports have identified a rare population of Wnt-responsive ATII is regarded as the major facultative progenitors,6, 7 which can be specifically marked by TM4SF1 expression in human lung.8 Distal airway stem cells (DASCs) with potential in stem cell-based therapies for acute and chronic lung diseases have been identified,9-12 expressing SOX9, TP63 and KRT5, all known to play pivotal roles in the maintenance of stem/progenitor cell states and epithelial differentiation in multiple organ types both in development and during adulthood.13-17 These DASCs were able to respond to injury induced by virus infection and assist airway and alveolar epithelial regeneration.12 These properties suggest the mechanism of the repair process of COVID-19 patients by which multiple stem/progenitor populations work in concert.
2 MATERIALS AND METHODS
2.1 ScRNA-seq analysis of BALF cells
Public data sets (GEO: GSE145926)18 and (GEO: GSE128033)19 which contain scRNA-seq data from BALF cells from three patients with moderate COVID-19 (M1-M3), six patients with severe/critical COVID-19 (S1-S6), three healthy controls (HC1-HC3) and one fresh BALF (GSM3660650) from a lung transplant donor (HC4) samples were used for bioinformatic analysis. Seurat v.3 was used for quality control. The following criteria were then applied to each cell of all nine patients and four healthy controls: gene number between 200 and 6000, UMI count >1,000 and mitochondrial gene percentage <0.1. After filtering, a total of 66 452 cells were left for the following analysis. A filtered gene-barcode matrix of all samples was integrated with Seurat v.3 to remove batch effects across different donors. In parameter settings, the first 50 dimensions of canonical correlation analysis (CCA) and principal component analysis (PCA) were used.
The filtered gene-barcode matrix was first normalized using ‘LogNormalize’ methods in Seurat v.3 with default parameters. The top 2000 variable genes were then identified using the ‘vst’ method in Seurat FindVariableFeatures function. Variables ‘nCount_RNA’ and ‘percent.mito’ were regressed out in the scaling step, and PCA was performed using the top 2000 variable genes. Then, UMAP was performed on the top 50 principal components for visualizing the cells. Meanwhile, graph-based clustering was performed on the PCA-reduced data for clustering analysis with Seurat v.3. The resolution was set to 1.2 to obtain a finer result.
Epithelial cells were re-clustered with Seurat v.3. Epithelial cells of all samples were re-clustered using the same parameter mentioned above in the clustering step, and parameter resolution was set to 0.3. Immune cell clusters were removed, and the other cells were re-clustered using the same parameter mentioned above in the clustering step, and parameter resolution was set to 0.4.
MAST20 in Seurat v.3 (FindAllMarkers function) was used to perform differential gene expression analysis. For each cluster of epithelial cells, differentially expressed genes (DEGs) were generated relative to all of the other cells. A gene was considered significant with adjusted P < .05 (P-values were adjusted by false discovery rate in MAST).
For analysis of engrafted GFP+ cells, single cells were captured and barcoded in 10× Chromium Controller (10× Genomics). Subsequently, RNA from the barcoded cells was reverse-transcribed and sequencing libraries were prepared using Chromium Single-Cell 3'v3 Reagent Kit (10× Genomics) according to the manufacturer's instructions. Sequencing libraries were loaded on an Illumina NovaSeq with 2 × 150 paired-end kits at Novogene, China. Raw sequencing reads were processed using the Cell Ranger v.3.1.0 pipeline from 10× Genomics. In brief, reads were demultiplexed, aligned to the human GRCh38 genome, and UMI counts were quantified per gene per cell to generate a gene-barcode matrix. Data were aggregated and normalized to the same sequencing depth, resulting in a combined gene-barcode matrix of all samples. Post-processing, including filtering by number of genes and mitochondrial gene content expressed per cell, was performed using the Seurat v.3. Genes were filtered out that were detected in less than three cells. A global-scaling normalization method 'LogNormalize' was used to normalize the data by a scale factor (10 000). Next, a subset of highly variable genes was calculated for downstream analysis and a linear transformation (ScaleData) was applied as a pre-processing step. Principal component analysis (PCA) dimensionality reduction was performed with the highly variable genes as input in Seurat function RunPCA. The top 20 significant PCs were selected for two-dimensional t-distributed stochastic neighbour embedding (tSNE), implemented by the Seurat software with the default parameters. FindCluster in Seurat was used to identify cell clusters.
2.2 Gene functional annotation
Gene Ontology (GO) enrichment analysis and Gene Set Enrichment Analysis (GSEA) of differentially expressed genes were implemented by the ClusterProfiler R package.21 GO terms with corrected P-value < .05 were considered significantly enriched by differentially expressed genes. Dot plots were used to visualize enriched terms by the enrichplot R package. For hypoxia gene analysis, the hallmark gene sets in MsigDB22 were used for annotation.
2.3 Single-cell trajectory analysis
To construct single-cell pseudotime trajectory and to identify genes that change as the cells undergo transition, Monocle2 (version 2.4.0) algorithm23 was applied to our data sets. Genes for ordering cells were selected if they were expressed in ≥1% cells, their mean expression value was ≥0.3 and dispersion empirical value was ≥1. Based on the 'DDRTree ' method, the data were reduced to two dimensional, and then, the cells were ordered along the trajectory.
2.4 Correlation analysis of BALF cells and engrafted cells
The scHCL Model24 was used to assess the similarity between BALF cells and engrafted cells. The expression patterns of highly variable genes of each cluster of engrafted cells (eg mature alveolar barrier cells) were taken as reference signatures to annotate BALF cells. Pearson's correlation score was calculated between each cell type of scRNA-seq data from engrafted cells and each cell of scRNA-seq data from BALF cells. Final annotation of each BALF cell was based on the highest correlation score. Linear regression analysis was performed between ratio of FCN1+ macrophage cell numbers in BALF and ratio of the epithelial cells in BALF annotated as mature alveolar barrier cells (ABCs) with 'lm' method.
2.5 Cell culture
Mouse lung P63+ KRT5+ progenitor cells were isolated and cultured as previously described.12 Briefly, lung lobes were collected and processed into a single-cell suspension by protease, trypsin and DNaseI. Dissociated cells were passed through 70-μm nylon mesh, washed twice with cold F12 medium and then cultured onto feeder cells (irradiated 3T3-J2 feeder cells) in culture medium including DMEM/F12, 10% FBS (Hyclone), Pen/Strep, amphotericin and growth factor cocktail as previously described. Cells were grown in a humidified atmosphere of 7.5% (v/v) CO2 at 37°C. To generate monoclonal cell, cells were processed and diluted into single-cell suspension. One single cell was aspirated and isolated by pipette under microscopy and then transferred into 96-well plate to expand.
2.6 Animal experiments
C57/B6 mice (6-8 weeks) were purchased from Shanghai SLAC Laboratory Animal Co., Ltd. and housed in specific pathogen-free conditions within an animal care facility (Center of Laboratory Animal, Tongji University, Shanghai, China). All animals were cared for in accordance with NIH guidelines, and all animal experiments were performed under the guidance of the Institutional Animal Care and Use Committee of Tongji University. For the lung injury mouse model, bleomycin was intratracheally administrated to isoflurane-anaesthetized mice at a concentration of 3 U/kg seven days prior transplantation. GFP-labelled cells suspended in 40 μL DMEM (1 million cells per mouse) were intratracheally transplanted. At distinct time points, mice were sacrificed and their lung tissues were harvested to detect GFP signal by fluorescence stereomicroscope (MVX10, Olympus).
2.7 Histology
Tissues were fixed with 4% PFA for 2 hours at room temperature and at 4°C overnight, followed by embedding in OCT. Immunohistochemistry was performed following heat antigen retrieval methods and stained with the following antibodies: GFP (goat, Abcam, 1:1000), Krt5 (rabbit, Thermo Fisher, 1:200), P63 (mouse, abcam, 1:100) and CD45 (rabbit, abcam, 1:200). Primary antibody was incubated at 4°C overnight, and second antibody at room temperature for 2 hours.
2.8 FACS sorting of engrafted GFP+ single cells
Transplanted lung was collected and immersed in cold F12 medium with 5% FBS, followed by being minced into small pieces and digested with dissociation buffer (F12, 1 mg/mL protease, 0.005% trypsin and 10 ng/mL DNaseI) on shaker in 37 degrees for 1 hour. Dissociated cells were filtered through 100-μm cell strainer, and Red Blood Cell Lysis Buffer was used to remove erythrocyte. Cell pellets were resuspended in DMEM containing with 1% FBS following washing twice and then passed over 30-μm strainers. Sorting and subsequent quantification were performed on BD FACS Arial cytometers. GFP+ cells were gated using SSC-A vs FSC-A, FSC-H vs FSC-W and SSC-H vs SSC-W gates, followed by SSC-A vs FITC-A gate.
2.9 Statistics
Differences of median percentage between healthy controls, moderate and severe groups of all cell types, TM4SF1+ AGER+ cells in all TM4SF1+ cells and BALF cells annotated to mature ABCs were compared using a Student's t test (two-sided, unadjusted for multiple comparisons) with R ggpubr v.0.2.5. Differences of gene expression levels between healthy controls, moderate and severe groups were compared using MAST in Seurat v.3. A gene was considered significant with adjusted P < .05 (P-values were adjusted by false discovery rate in MAST).
3 RESULTS
In order to fully elucidate the epithelial damage and repair mechanism, we analysed the single-cell transcriptomic profile of lung BALF to quantify the major events post-infection and focused on structural epithelial cells. BALF is a useful technique for sampling the human lung, providing landscape information of the whole lower respiratory tract. The current study was based on public scRNA-seq data sets on BALF cells from three patients with moderate COVID-19 (M1-M3), six patients with severe/critical infection (S1-S6) and four healthy controls (HC1-HC4).18, 19
Firstly, we performed unsupervised clustering analysis on the whole data set to separate EPCAM+/TPPP3+/KRT18+ epithelial cells from other cells types (mostly immune cells) in the BALF (Figure S1A,B). Re-clustering analysis identified 12 epithelial cell clusters, among them four were identified to be co-expressing immune markers which could be epithelial cells engulfed by leucocytes (Figure S1C,D). The other eight distinct epithelial cell clusters composed of Club/goblet cells (Cluster 0. SCGB1A1+/MUC5AC+), various types of ciliated cells (Cluster 1-5. FOXJ1+) and alveolar cells (Cluster 6. HOPX+/SPC+). Most interestingly, a cluster of lung progenitor cells (Cluster 7. TM4SF1+/KRT5+/SOX9+) was identified, which will be analysed in details as below (Figures 1A, S2).
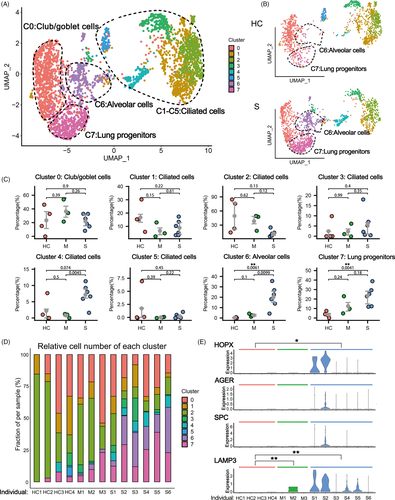
When we compared the HC group with the other two infected groups, we found significant higher proportion of alveolar cell clusters (Cluster 6) in the BALF of patients with severe infection (Figure 1B-D). Of note, the HOPX+/AGER+ type I alveolar cells (ATI) and SPC+/LAMP3+ ATII were almost undetectable in the BALFs of healthy control persons due to the tissue integrity of their lungs. In contrast, in the severe COVID-19 patients, both ATI and ATII cell markers were detected in the lavage fluid, probably due to the tissue collapse and desquamation of alveolar cells (Figure 1E). This phenomenon was not obvious in moderate COVID-19 patients, which was also consistent with previous pathological observation.25 Therefore, the number of alveolar cells (or the alveolar marker gene expression level) in BALFs could be clinically used to measure the structural integrity of lung, which could serve as an index of disease severity for COVID-19 patients.
In the BALFs of patients with severe infection, we also found significant higher proportions of progenitor cell clusters (Cluster 7) (Figure 1B-D). Multiple stem/progenitor cell populations have been reported to play critical roles in damage repair after various types of acute lung injury.26 Among them, a rare population of Wnt-responsive ATII is regarded as the major facultative progenitors,6, 7 which can be specifically marked by TM4SF1 expression in human lung.8 In the current study, we found that in the patients of severe group, the number of TM4SF1+ cells increased remarkably, which implicated the rapid activation of such progenitor cells by tissue damage (Figure 2A,B). Consistently, we observed co-expression of TM4SF1 and mature alveolar cell markers, AGER (also known as RAGE) and SPC, in a substantial proportion of TM4SF1+ cells (7.45% in average) in patients of severe group (Figure 2C). These results suggested that the TM4SF1+ progenitor cells had the potential to differentiate into mature alveolar cells and regenerate the damaged alveoli of COVID-19 patients.
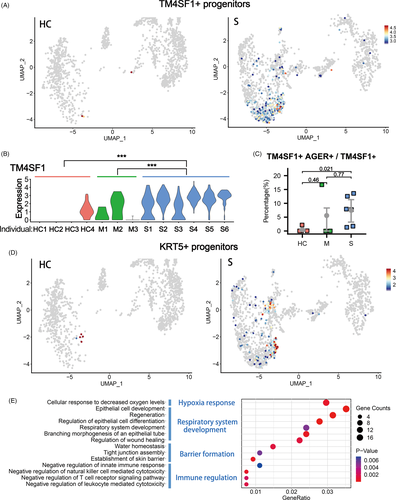
KRT5+ cells are also reported to have lung stem/progenitor characteristics. Such cells are originated from various primitive progenitors in proximal or distal airways and could expand/migrate to inflamed damaged lung parenchymal region to form ‘KRT5 pods’ once activated by various types of tissue injury including influenza virus infection.9, 12, 27-30 Recent studies showed that the expanded KRT5 cells could give rise to new pulmonary epithelium, which was now believed to have important epithelial barrier function to protect the lung tissue from further damage.8, 30, 31 Specific ablation of the newly expanded KRT5+ cells resulted in persistent hypoxaemia, confirming the contribution of these cells in recovery of lung function.12 In the current study, we found that in the patients of severe group, the number of KRT5+ progenitor cells increased remarkably, in together with the elevated expression of another related progenitor marker gene SOX910, 32 (Figure 2D, S2C).
Then, we examined the function of genes whose expression level was significantly up-regulated in KRT5+ cells by Gene Ontology analysis. The results showed that KRT5+ cells were responsive to the low oxygen condition of severe COVID-19 patients and actively participated in the development and generation of respiratory epithelial system. More importantly, such cells highly expressed multiple tissue integrity genes including Claudin1, Claudin4, TJP1, Stratifin, AQP3 and Scnn1A, which were associated with epithelial barrier establishment, tight junction assembly, maintenance of fluid homeostasis and prevention of leucocyte mediated cytotoxicity (Figure 2E). These functions of KRT5+ cells were rather important for a damaged lung as reconstitution of tight alveolar barrier between atmosphere and fluid-filled tissue is required for recovery of normal gas exchange, while persistent disruption of the alveolar barrier could result in catastrophic consequences including alveolar flooding, ‘cytokine storm’ attack from the circulating leucocytes and subsequent fibrotic scarring.33
In order to examine the process whereby KRT5+ progenitor cells restore mature alveolar barrier in injured lung, we isolated the mouse KRT5+ progenitor cells (previously also named distal airway stem cells)12 for transplantation assay as described in Figure 3A. Briefly, the cell population was trypsinized into single-cell suspension and a single-cell-derived pedigree clone was propagated, followed by GFP labelling by lentiviral infection for further analysis. Immunostaining showed that all cultured GFP+ KRT5+ progenitor cells expressed KRT5 and P63 marker genes (Figure 3B). Then, we transplanted the cultured KRT5+ progenitor cells into the bleomycin-injured mouse lung by intratracheal instillation. Transplanted lungs were evaluated at 30 and 90 days afterwards. The result showed substantial persistent engraftment of the GFP+ cells into the host lung, which takes up 2.27% and 2.44% of total lung cells on Day 30 and 90 post-transplantation, respectively (Figure 3C,D). Cryo-sectioning and immunostaining of the host lung demonstrated that some transplanted GFP+ KRT5+ progenitor cells differentiated into alveolar barrier cells (ABCs) in lung parenchyma, establishing a large area of sealed cavities next to consolidated regions, which efficiently prevented CD45+ immune cell infiltration into such area (Figure 3E, S3A).
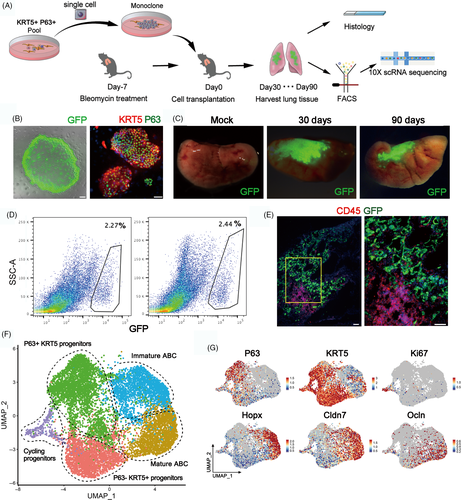
Next, we harvested the 30-day and 90-day transplanted lungs and sorted the engrafted GFP+ single cells for scRNA-seq analysis. Clustering analysis of the sequencing data identified three clusters of KRT5 + progenitor cells, including the most immature P63 + KRT5+ progenitors, the P63-KRT5+ progenitors and the actively cycling Ki67+ KRT5+ progenitors. We also identified two KRT5-differentiated ABCs which both highly expressed early alveolar marker HOPX and paracellular adhesion marker Claudin7. One of the two ABC clusters highly expressing tight junction marker Occludin (OCLN) was supposed to be more mature than the other one (Figure 3F,G). Gene ontology analysis demonstrated that the P63+ KRT5+ progenitors highly expressed multiple genes whose function was related to cell stemness maintenance, chemotaxis and inhibition of cell apoptosis. In contrast, the mature ABC highly expressed multiple genes (including HOPX, SPD, OCLN, CDH1, Claudin7, Claudin4, AQP3, etc) whose function was related to lung morphogenesis, tight junction assembly and water homeostasis (Figure S3B,C).
To further dissect the lineage relationship between different clusters of engrafted cells, we performed the Monocle pseudotime analysis based on the scRNA-seq data. The result indicated that the P63+ KRT5+ progenitors could differentiate into P63− KRT5+ progenitors and immature ABCs, which eventually give rise to OCLN+ mature ABCs (Figure 4A,B). Consistent with the pseudotime analytical data, we noticed that compared to the 30-day engrafted cells, the 90-day engrafted cells had relatively more mature ABCs, less immature ABCs and less P63-KRT5+ progenitors (Figure 4C). Altogether such data revealed that the tight alveolar barrier would be gradually established by KRT5+ progenitor cell differentiation.
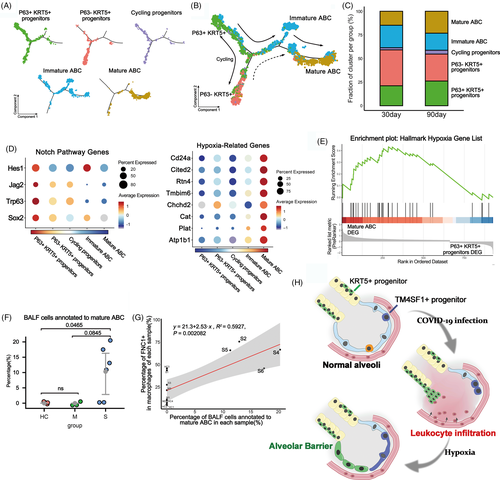
Next, we asked which molecular signalling pathways were involved in the establishment of alveolar barrier. Previous studies indicated that Notch signalling is critical for activation of P63+ KRT5+ progenitors in lung, but persistent Notch signalling prevents further differentiation of cells.29 Consistently, here we found that the expression of multiple Notch pathway component genes was up-regulated in P63+ KRT5+ progenitors but gradually down-regulated when the cells were differentiating to mature ABC (Figure 4D). In addition, sense of low oxygen level through hypoxia pathway is known to be critical for the expansion of KRT5+ progenitors.34 Here, we found that the hypoxia pathway component gene expressions were relatively low in P63+ KRT5+ progenitors but were gradually up-regulated when the cells were differentiating to ABC (Figure 4D). Further gene set enrichment analysis (GSEA) also demonstrated that the expression of the hallmark hypoxia gene list in Molecular Signatures Database (MSigDB) was significantly enriched in mature ABC (P = .018) (Figure 4E). Altogether, these data showed that Notch and hypoxia pathways were important for the regulation of progenitor cell fate.
Lastly, we mapped our scRNA-seq data of transplanted progenitor cells back to the COVID-19 BALF scRNA-seq data to investigate whether any mature alveolar barrier has been established in patients. We extracted the mature ABC gene expression signature and evaluated the signature signal in COVID-19 patients. The result showed that approximately 10% of the epithelial cells in BALF of severe patients could be annotated as mature ABC, and such ABC only existed in four severe patients (S2, S4, S5 and S6) but not in healthy persons or other patients (Figure 4F). So why the four patients have much more mature ABC than others? Interestingly, we found that generally the individuals' mature ABC cell numbers were positively correlated with their FCN1+ macrophage cell numbers in BALF (P = .002), and the patient S2, S4, S5 and S6 had much more FCN1+ macrophages in BALF than most of the other individuals (Figure 4G). FCN1+ macrophages were reported to be highly pro-inflammatory and responsible for the tissue damage in COVID-19 patients.18 Therefore, it seems that the establishment of new alveolar barrier was closely associated with severity of tissue damage and inflammation at individual level.
4 DISCUSSION
Altogether, our current studies uncovered a possible mechanism of lung repair after severe SARS-CoV-2 infection. In those severe patients, the virus infection led to alveolar cell death and leakage of epithelial barrier, which resulted in massive flood of proteins-enriched fluids and leucocytes into alveolar cavity, which finally led to pulmonary oedema and tissue hypoxia. In this situation, as repair backups, KRT5+ and TM4SF1+ progenitor cell could be activated by the hypoxia and other multiple microenvironment signals to expand, migrate and differentiate into new functional cells. Eventually, the KRT5+ progenitor-derived ABCs could rapidly restore new epithelial barriers to cover the denuded alveoli and seal the leakage. Simultaneously, the TM4SF1+ progenitor cells could gradually regenerate new functional ATII and ATI cells. The synergic act of two types of progenitor cells could make timely repair of alveoli in an acute injury scenario (summarized in Figure 4H). Of course, there could be more resident or circulating stem/progenitor cells working in concert with them to achieve maximal repair. Of note, our current studies were based on limited sample data. Future study within a larger patient cohort could further facilitate our understanding of the repair process of COVID-19 patients, and development of potential progenitor cell-based therapeutic strategies.
ACKNOWLEDGEMENTS
This work was funded by the National Key Research and Development Program of China (2017YFA0104600 to W. Zuo), National Science Foundation of China (81770073 to W. Zuo), China-Germany Bilateral Collaborative Grant in COVID-19 Related Research (C-0025 to W. Zuo), Shanghai Science and Technology Talents Program (19QB1403100 to W. Zuo), Tongji University (Basic Scientific Research Interdisciplinary Fund and 985 Grant to W. Zuo) and Guangzhou Medical University annual grant to W. Zuo. We thank Prof. Zheng Zhang group for sharing their original COVID-19 BALF scRNA-Seq data set to public. We salute to medical workers who sacrificed their lives in fight against the COVID-19 pandemic.
CONFLICT OF INTEREST
All authors declare no conflicts of interests.
AUTHOR CONTRIBUTIONS
WZ and TZ designed the study. ZXZ, YZ, YQZ and XFW involved in data collection and analysis. ZXZ, YZ, YQZ and WZ prepared the manuscript.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.