Long-term outcomes of open versus closed rectal defect after transanal endoscopic microscopic surgery
Abstract
Aim
Management of the rectal defect after transanal endoscopic microsurgery (TEM) is a matter of debate. Data are lacking on long term outcomes and continence of patients with open or closed rectal defect. We sought to analyse these in a retrospective cohort study.
Methods
Patients undergoing TEM via the Specialist Early Rectal Cancer (SERC) MDT between 2012 and 2019 were included from a prospectively maintained database. These were divided into two groups – open and closed, based on management of rectal defect. Patient demographics and outcomes, including pre- and postoperative oncological staging, morbidity, mortality, length of stay and faecal incontinence severity score (FISI) scores were assessed.
Results
A total of 170 matched patients were included (70-open, 100-closed rectal defects). Short-term complications (bleeding, infection, urinary retention and infection, length of stay and pain) were 18.8% with no significant difference between the two groups (22% vs. 16%). Most of the defects were well healed upon endoscopic follow-up; more unhealed/sinus formation was noticed in the open group (p = 0.01); more strictures were encountered in the closed group (p = 0.04). Comparing the open and closed defect groups, there was no difference in the functional outcome of patients in those who developed sinus (p = 0.87) or stricture (p = 0.79) but a significant difference in post-TEMS FISI scores in those with healed scar, with those in closed rectal defect group with worsening function (p = 0.02).
Conclusion
There are pros and cons associated with both rectal defect management approaches. Long-term complications should be expected and actively followed up. Patients should be thoroughly counselled about these and possible deterioration in continence post-TEM.
What does this paper add to the literature?
This is the first paper to address and show data for the long-term outcomes of rectal defect management after TEMS. We have shown that while there is no difference between leaving the defect open and suturing it to close to avoid short-term complications, significant impact on function and healing should be expected. We have demonstrated through judicious endoscopic surveillance that most of the rectal defects will heal, despite showing early sinus formation; however, long standing stricture formation was encountered in both groups, with closure of the defect more likely to result in luminal narrowing.
INTRODUCTION
The incidence of early rectal cancer (ERC), defined as lesions limited to bowel wall and not extending beyond submucosa (T1) or muscularis propria (T2) without lymph nodal involvement, has increased in the recent times, possibly due to widespread introduction of screening programmes and impressive improvements in diagnosis, staging and treatment modalities of rectal cancer over the last two decades. It is thought to constitute approximately 40% of all colorectal cancer diagnoses [1]. While the 5-year survival rate is approximately 95%, management of ERC remains controversial. TEM presents a less invasive alternative option with reported postoperative clinical morbidity rates of less than 10%, no genitourinary/sexual changes and a low mortality rate [2-4]. Lack of lymphadenectomy makes it only suitable for selected T1 cancers [5].
While more and more centres adopt the technique and develop expertise, endoluminal suturing of the rectal defect remains a particularly difficult skill to master and the data around leaving the defect unsutured or otherwise remain scanty. Recently, some studies, including randomised controlled trials, have shown no difference between leaving the defect open or sutured close for various short-term outcomes. However, no study has assessed long-term outcomes of these two approaches. We, therefore, aimed to look at long term outcomes in terms of recurrence, structural healing and impact on continence in patients who had rectal defect closed or left open after TEM.
METHODS
All patients undergoing full thickness rectal excision using TEMS from January 2012 to December 2019 referred from the Regional Specialist Early Rectal Cancer (SERC) MDT were included in the study. The SERC MDT serves the 2.5 million population catchment areas of Merseyside and Cheshire and receives referrals from six regional hospitals and beyond with an average of 350 referrals per year. The SERC cancer network encourages referral of all patients with stage 1 rectal cancer in line with the National Institute for Health and Care Excellence (NICE) recommendations and those of large and complex rectal polyps and T1 or T2 node negative rectal tumours that may be amenable to local therapies. Endoscopic mucosal resections (EMR) or endoscopic submucosal dissections (ESD) and TEM are all performed at our centre within 4 weeks of referral. Patients who are deemed suitable for surveillance are followed up using local agreed surveillance guidelines that include flexible sigmoidoscopy, carcinoembryonic antigen (CEA) and magnetic resonance imaging (MRI) biannually and a CT scan annually for 24 months in cases of malignant lesions and flexible sigmoidoscopy within 4–6 months and then 12 months followed by the British Society of Gastroenterology (BSG) polyp surveillance guidelines.
All TEM procedures in this study were performed by two dedicated TEM surgeons (SS and SA) working at the same trust. Both surgeons had formal training in local excisional surgery and had each performed over 100 TEM procedures. Transanal endoscopic microsurgery (TEM) and transanal endoscopic operation (TEO) platforms were used equally by both surgeons. The use of platform did not influence the surgeon’s decision to leave open or close rectal defects after full thickness rectal excision, which in turn was reliant on surgeon discretion, size of the defect and distance from anal verge and was independent of gender, age, pathology and staging. The rectal defect was closed with 2/0 vicryl sutures V323H, MH needle® by one surgeon throughout the study period; however, the second surgeon changed to V-Loc PBT barbed monofilament 45 cm length in December 2016 due to ease in handling. All except six patients had full mechanical bowel preparation. Two phosphate enemas were administered on the morning of the procedure for patients who were not suitable for full oral bowel preparation.
Data were extracted retrospectively from a prospective maintained electronic database after local hospital review board consent was sought. Patient demographics included age, gender, American Society of Anaesthesiology (ASA), fragility score, and any previous EMR were recorded. Short-term outcomes including postoperative bleeding, urine retention, infection, use of analgesia, length of stay, 30- and 90 day mortality, readmission and return to theatre were recorded. All patients had intra-operative intravenous antibiotics and were discharged home with a 5 day course of oral antibiotics and laxatives for one week.
Lesion characteristics including size, position and distance from anal verge were noted. Final histopathology, including grade of dysplasia (low/high) in benign cases and T stage and submucosal invasion (Sm1-3) in malignant lesions were recorded. Post-TEM first and subsequent flexible sigmoidoscopy reports were recorded. Findings from flexible sigmoidoscopy reports during surveillance were categorised into completely healed scar-site (group A), unhealed/sinus formation at scar-site (group B) and stricture/narrowing (group C) at scar-site. Faecal incontinence severity score (FISI) was recorded pre- and postoperatively (12 months) from patients and compared with their post-TEM scar-site findings.
FISI scores were expressed as median and interquartile range (IQR). Measurements prior to and after the TEM were mutually compared using the paired t-test. Statistical differences between patients in different groups were analysed by the v2 test of independence for categorical data and Student's t-test or the Mann–Whitney U test for continuous data between groups. A p-value less than 0.05 was considered statistically significant. Calculations were made using the SPSS statistics package for Windows (International Business Machines Corp.), version 25.0.
RESULTS
During the study period, 198 TEM procedures were carried out. Patients who required subsequent TME rectal resections post-TEM (n = 22) due to poor prognostic features on final histology (tumour > T1Sm3, poor differentiation, lymphovascular invasion, tumour budding and tumour at resection margins R1) and those who underwent salvage surgery were excluded. No patient had neoadjuvant chemoradiotherapy and those who had radiotherapy for prostate cancer before diagnosis of rectal polyps were also excluded. Five patients lost to follow-up and one patient who died within 90 days of TEM surgery were not included in the analysis. Data from 170 patients were available for the final analysis, with 70 patients in the open and 100 in the closed rectal defect groups.
The two groups were well matched with no differences in terms of gender, age, ASA, body mass index (BMI), frailty, size, distance from the anal verge, position of the tumours and malignant potential (p > 0.05). Patient demographics and distribution of rectal lesions in relation to position are summarised in Table 1.
| Open rectal defect | Closed rectal defect | p-value | |
|---|---|---|---|
| Number of patients | 70 | 100 | |
| Age (median and IQR) | 72 (27–81) | 70 (47–89) | >0.05 |
| Gender (M:F) | 58:19 | 61:32 | >0.05 |
| BMI (median and IQR) | 28.2 (21.5–44.5) | 27.5 (16.6–35.1) | >0.05 |
| ASA (median and range) | 2 (1–3) | 2 (1–3) | >0.05 |
| Fragility score (median and range) | 3 (1–5) | 3 (1–4) | >0.05 |
| Benign | 29 | 41 | >0.05 |
| Malignant | 41 | 59 | |
| Size of lesions (cm) (median and IQR) | 3.5 (1–10) | 3.0 (2–6.5) | >0.05 |
| Distance from anus (cm) (median and IQR) | 6 (1–8) | 5 (2–12) | >0.05 |
| Position of lesions | |||
| Anterior | 19 | 25 | >0.05 |
| Posterior | 26 | 39 | |
| Right lateral | 14 | 19 | |
| Left lateral | 8 | 17 | |
| Circumferential >60% lumen | 2 | 1 | |
Final histology revealed 44% of the total lesions to be benign (70/170) and the rest were found to be malignant (100/170). Of the 100 malignant lesions, the majority were identified as adenocarcinoma (92/100), with 82% staged as pT1 (Sm1 = 23/82, Sm2 = 27/82, Sm3 = 32/32/82). Eight malignant tumours were found to be pT2 and two were staged as pT3 on final histology. Table 2 lists the details of the tumour histology in both groups.
|
Open rectal defect (n = 70) |
Closed rectal defect (n = 100) |
p-value | |
|---|---|---|---|
| Malignant | 41 | 59 | >0.05 |
| T1 | 30 | 52 | |
| Sm1 | 8 | 20 | |
| Sm2 | 9 | 14 | |
| Sm3 | 13 | 18 | |
| T2 | 5 | 3 | |
| T3 | 1 | 1 | |
| Neuroendocrine | 4 | 2 | |
| Mucinous | 1 | 1 | |
| Benign | 29 | 41 | >0.05 |
| LGD | 11 | 15 | |
| LGD+HGD | 18 | 26 |
- Abbreviations: HGD, high grade dysplasia; LGD, low grade dysplasia.
Among the benign lesions, low grade dysplasia was found in 37% (26/70) of the lesions and 63% (44/70) were reported as low with high grade dysplasia. Among 100 malignant lesions, 59 rectal defects were closed and 41 were left open. Similarly, in 70 benign cases, 41 were closed and 29 were left open.
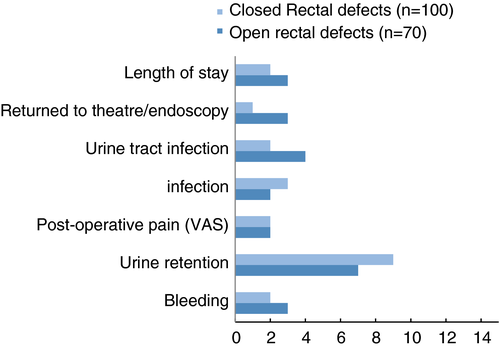
Overall, short-term complications for our patient cohort were 18.8% with no significant difference between the open and closed defect groups (22% vs. 16%; p > 0.05) in terms of postoperative bleeding, local infection, urinary retention, urinary tract infection, length of stay and postoperative pain using the visual analogue score (VAS) post TEM. This is illustrated in Figure 1. Four patients (3 in open, 1 in closed) returned to theatre or required endoscopy procedures for postoperative bleeding; there was no mortality in 30 days and one patient died within 90 days of TEM (benign lesion) due to myocardial infarction, which was unrelated to the procedure.
Three patients in the open rectal defect group (41/70 malignant lesions) developed local recurrence after TEM over a median follow-up of 3.5 years. Two out of the three were staged as T2 tumours postoperatively and therefore underwent adjuvant chemoradiotherapy. Local recurrence was identified at 18 and 21 months, respectively. The third patient had a T1Sm3 tumour and refused to have adjuvant therapy. He ended up with local recurrence at 12 months. All three patients underwent formal TME rectal surgery and had not shown any systemic recurrence at the time of submission of this manuscript.
In the closed rectal defect group, four local recurrences were identified (59/100 malignant lesions) over a median follow-up of 3.2 years. Out of these four, two patients had T1Sm2 and two had T1Sm3 histology. T1Sm2 patients did not have any adjuvant therapy and had local recurrence at 18 and 20 months, respectively. One patient with T1Sm3 had adjuvant radiotherapy and the other one did not and both had local recurrence at 11 and 6 months, respectively post-TEM. All patients had formal TME rectal cancer surgery for local recurrence.
Assessment of rectal defect after TEM was recorded using lower GI endoscopy. A total of 80% of patients had flexible sigmoidoscopy within 6 months of the initial procedure and 92% had lower GI endoscopy (flexible sigmoidoscopy/colonoscopy) within 12 months. Endoscopic findings from post-TEM assessment of rectal defect endoscopically were categorised into three categories: healed scar-site, unhealed/sinus formation and stricture/narrowing (Table 3). Whilst most of the defects in both groups were well healed upon follow-up, more unhealed/sinus formation was noticed in the open group. However, more strictures were encountered in the closed group.
| Rectal defects |
Healed scar-site (n = 142) |
Unhealed/sinus formation (n = 18) |
Stricture/narrowing (n = 10) |
|---|---|---|---|
| Open cavity (n = 70) | 55 | 12 | 3 |
| Closed cavity (n = 100) | 87 | 6 | 7 |
| p > 0.05 | p = 0.01 | p = 0.04 |
Among 18 patients with unhealed/sinus formation, 11 had healed completely at a median follow-up of 12 months (range 6–18 months). Six persisted as sinuses. Interestingly, more sinuses failed to heal in the open than the closed group (5 vs. 1). One patient was lost to follow-up. In all 10 patients who were found to have strictures, no further treatment was needed as the endoscopists were able to pass the scope through all of them.
Functional outcome in terms of pre- and postoperative FISI scores (at 12 months) were recorded and available for 151 patients. A total of 37 patients underwent adjuvant radiotherapy, as their final histology revealed poor prognostic features. These patients were not included for functional outcome analysis due to bias of radiotherapy induced incontinence and rectal sensitivity. Consequently, final analysis was done using data from 114 patients. Comparisons were made of pre- and postoperative FISI scores of patients with complete healed scar-site (Group A), unhealed/sinus at the site (Group B) and stricture (Group C). Overall, there was a significant difference in pre- and post TEM FISI scores in all three groups (p < 0.00001, p < 0.00001, p = 0.02). Comparing the open and closed defect groups, there was no difference in the functional outcome of patients in those who developed sinus or stricture but a statistically significant difference in post TEM FISI scores in group A, with those in the closed rectal defect group with worsening function (p = 0.02). These results are detailed in Table 4.
| Healed scar | Unhealed/sinus formation | Stricture/narrowing | |
|---|---|---|---|
| Numbers of endoscopic findings post-TEMS | 142 | 18 | 10 |
| FISI scores available | 92 | 13 | 9 |
| Open rectal defects (n = 46) | 33 | 9 | 4 |
| Closed rectal defects (n = 68) | 59 | 4 | 5 |
| Open rectal defects (n = 46) | |||
| Preoperative FISI median (range) | 2 (0–7) | 3 (0–7) | 2 (0–7) |
| Postoperative FISI median(range) | 5 (0–16) | 18 (0–25) | 5 (01–15) |
| Closed rectal defects (n = 68) | |||
| Preoperative FISI median (range) | 2 (0–5) | 2 (0–6) | 1 (0–5) |
| Postoperative FISI median (range) | 6 (0–18) | 15 (0–20) | 5 (0–18) |
| Pre-TEMS open rectal defects vs. closed rectal defects | p = 0.467 | p = 0.87 | p = 0.79 |
| Post TEMS open rectal defects vs. closed rectal defects | p = 0.02 | p = 0.42 | p = 0.939 |
- Values in bold are statistically significant.
DISCUSSION
This is the first study to look at the long-term outcomes of rectal defect management from TEM. We have shown that while there is no difference between leaving the defect open and suturing it closed in terms of short-term complications, significant impact on function and healing should be expected. We have demonstrated through judicious endoscopic surveillance that most rectal defects will heal, despite showing early sinus formation; however, long standing stricture formation was encountered in both groups, with closure of the defect more likely to result in luminal narrowing. Assessment of function and relationship to the rectal defect was demonstrated to be more complex and there seems to be a significant deterioration in function, as shown by FISI scores, in patients who undergo TEM, regardless of how the rectal defect is managed. Deterioration in continence seemed to be largely independent of how the defect was managed, or development of a complication (sinus formation/stricture) as groups A, B and C all demonstrated a significant difference in FISI scores pre- and post TEM. However, when broken down according to the status of the rectal defect, a significant difference was only demonstrable in Group A, where closing the rectal defect was associated with worsening function (p = 0.02). This is a surprising finding as complete healing would rationally be associated with a more stable functional outcome as compared to those with a complicated recovery (Groups B and C). This finding certainly warrants further investigation.
Debates around management of the rectal defect during TEM are intensifying with the passage of time. The previously held notion of an intraperitoneal defect being associated with increased morbidity and mortality is slowly being discounted [6] and more and more surgeons are honing their endoscopic skills, performing TEM for lesions previously discarded due to risk of peritoneal breach.
Many studies have directly compared the outcomes from leaving the defect open and suture closure and found variable results. The first randomised controlled trial (RCT) on the subject followed patients up for a month [7]. Postoperative bleeding was the only complication encountered and both techniques were judged to be safe and no better than the other. This was validated in a large multicentre comparative study where intra-operative complications occurred in 8% and postoperative morbidity in 19%. Rectal defects were left open in 47% without increasing complications or compromising continence [8]. However, a more recent study has postulated that open management of the rectal defect after TEM may be associated with more postoperative complications (19% vs. 8.4%) but it does pose a viable approach in patients where the defect does not compromise the peritoneal cavity [9]. Another subject of concern has been association of management of TEM defect with increased postoperative pain. This gained popularity after a study in 2011 concluded that postoperative pain after sutured closure of the rectal defect in TEM was associated with a high readmission rate and also high incidence of wound dehiscence [10]. However, a more recent multicentre RCT has nullified these results, exhibiting no difference in postoperative pain between sutured or open defect management. Findings from this trial reassure us that when the mesorectum is intact, open management of a rectal defect does not compromise postoperative recovery [11]. Another study found increased risk of bleeding with open rectal defects but no significant difference overall between the two techniques [12]. Our results also demonstrated no difference between the two groups in terms of infection, bleeding, postoperative pain, urinary retention, urinary tract infection, reinterventions, length of stay and bleeding.
No study in the past has commented on long-term endoscopic surveillance and long-term complications. Approximately 16% of our patients developed sinuses/strictures on surveillance. Significantly more strictures were seen in the closed group. This was independent of the size of the resected lesion. Our findings are in line with a study that investigated development of strictures after TEM. They found that the risk was highest with circumferential lesions (75%) and that the overall incidence in those more than 5 cm was only 3%. No stenoses were witnessed in lesions measuring less than 5 cm [13]. Mucosal ischaemia and lack of mucosal apposition could both account for stricture formation. There is some evidence that circumferential mucosal deficit is an independent risk factor [14, 15]. However, we found more strictures in the closed group than open and therefore it is not apparent if these two factors are indeed the most likely culprits. It is safe to say that development of stenosis after TEM is a multifactorial process. Thankfully, most patients do not develop symptoms and those who do are easily amenable to local therapies.
Faecal incontinence is not uncommon after TEM, with a reported incidence of up to 30% [16] and prevalence of around 2%–12% [17]. It is reasonable to assume that insertion and repositioning of the rectoscope during the procedure may damage the internal anal sphincter (IAS), while larger excisions may negatively impact rectal capacity and sensation [18]. There is data from studies reporting anorectal function and manometry in patients with TEMS. Effects demonstrated are a decrease in anal squeeze pressure and rectoanal inhibitory reflex, as well as a persistent reduction in rectal perception and compliance [18]. Defects in IAS have also been found post-procedure in up to 30% of patients, leading to a reduction in anal resting and squeeze pressures [19]. It has also been deduced that resecting more than 50% of rectal circumference is also adversely associated with rectoanal inhibition reflex and sphincter reflex contractions [19]. We saw a significant difference in continence scores in our patient cohort before and after the procedure and while we did not perform a multivariate analysis to assess the risk factors for this, many studies have already alluded to that and identified old age, full thickness excisions and malignant lesions to be independent risk factors [16, 20].
Another important driver promoting closure of the rectal defect is to develop the technical skills which would be needed if a breach to the peritoneal cavity was to happen, particularly in anteriorly placed neoplasms. These breaches are not uncommon (approximately 6%) [21, 22] and must be sutured. If routinely closing the defects is employed, surgeons performing the procedures must have the required skillset to do so when it is needed, particularly in situations when suturing is quite challenging. It has been feared that suturing a rectal defect leads to an increase in operating times and lengthens the procedure. However, Lee et al. [12] found no significant difference in the operating time (82 vs. 85 min) between suture closure and open rectal defects. Median time taken for suturing a rectal defect is 12 min (range 5–30 min) in our own experience. The flip side to this is recognition of defects that will not be amenable to closure, or will have a high risk of dehiscence if closed. These have been reported to occur in up to 30% of procedures [8]. Such defects can be safely managed as open wounds and closure is best avoided in such circumstances.
Our study is limited by its retrospective nature, although data were retrieved from a prospectively maintained database. This is a single, albeit regional, centre experience and therefore, is subject to inherent selection biases and the usual disadvantages that a retrospective analysis brings, despite the careful and rigorous follow-up performed herein.
In conclusion, management of the rectal defect after TEM remains a matter of debate and largely at the discretion of the operating surgeon, and long-term outcomes and delayed complications should be expected and actively followed up. Patients should be adequately and appropriately counselled for the deterioration in bowel function and continence.
CONFLICT OF INTEREST
None to declare.
FUNDING INFORMATION
No funding was sought for this project.
AUTHOR CONTRIBUTION
KA, DS, SG and AK undertook data collection. KA performed analyses, analysed data and wrote the manuscript. SA and SS provided surgical expertise for the project, where TA oversaw the histological aspects of the project.
ETHICS APPROVAL
Local hospital ethics approval was sought for and granted for the purpose of this study.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.