‘Let's talk about sex’: a patient-led survey on sexual function after colorectal and pelvic floor surgery
Funding information
This study received no external funding. All authors involved volunteered their own time.
Abstract
Aim
Discussions regarding sex after colorectal and pelvic floor surgery are often overlooked by clinicians. This is the first patient designed and delivered study to explore sexual function and practices after colorectal surgery. The aim was to explore the questions about sex that matter to patients and their partners following colorectal or pelvic floor surgery through a patient and public involvement survey. The results of this work will underpin the creation of a sex patient reported outcome measure.
Methods
An anonymous online survey tool (Survey Monkey™) was disseminated via social media (Twitter, Facebook). Thematic analysis was applied to 130 free text comments posted by participants to identify key themes.
Results
Some 632 individuals completed the survey. Most respondents were women (80% n = 507), 49.5% (n = 312) were married and 14% (n = 87) identified as LGBT+ (lesbian, gay, bisexual and transgender +). Indications for surgery varied: 34% were treated for ulcerative colitis (n = 214); 31% Crohn's (n = 196); 17% (n = 109) cancer; and 17% (n = 110) for perianal fistula. For patients who had a stoma formed (85%, n = 540), over half (51%, n = 324) lived with their stoma for 1–5 years. Respondents reported substantial alterations to their preferences for sexual positions, sexual activity and body confidence following surgery. Most respondents indicated that they were not offered advice about sex by a healthcare professional.
Conclusions
The survey showed a substantial impact on the mechanics of sex following colorectal surgery. Few patients were offered preoperative information regarding sex, which has implications for informed consent. This study demonstrates a clear unmet need, voiced by patients, that open dialogue is necessary preoperatively to discuss sexual (dys)function.
What does this paper add to the literature?
This is the first paper to be conceptualized and delivered by patients, with foundational patient and public involvement (PPI). It discusses in detail the impact of colorectal and pelvic floor surgery on sex from a patient's perspective and highlights the need for an open dialogue about sexual activity between clinicians and patients.
INTRODUCTION
Intimacy, sexual function and relationships are widely considered to be important aspects of our psychological, physical and emotional welfare as humans. However, diseases which affect the colon, rectum or other pelvic organs may cause disruption to any (potentially) sexually active individual [1-3], as may the treatment of such conditions or diseases, including chemotherapy, radiotherapy or surgery [4-6]. Sexual activity after surgery may sometimes improve, due to elevations in self-esteem, reduction in pain or the restoration of continence [7, 8]. However, for some the inability to resume sex, or embark on a life where sexual activity is no longer an option or has to be significantly altered, can be life-changing [9].
Discussions with healthcare professionals around resuming sexual activity may vary in quality and quantity, and patients often find it difficult to initiate such conversations [10, 11]. Taboo, embarrassment, cultural context, physical setting and individuals' personalities can all create barriers to open dialogue [5, 12]. The language used is crucial and requires ‘emotional intelligence’ from healthcare workers to pick up on cues made by patients to navigate and normalize such conversations [13]. This leads to the risk that sex postoperatively may not be discussed or may only be discussed briefly and/or superficially, despite evidence that sex after surgery should be talked about during the counselling and consent process [14]. The authors also feel from their own and extensive anecdotal experiences that this remains lacking.
Our aim was to open a conversation amongst patients and discover whether sex is an important topic. We aimed to explore the impact that colorectal and pelvic floor surgery has on the sex lives of patients and investigate whether adequate information, advice and support regarding sex are provided by surgical teams. This survey was designed to be the patient and public involvement (PPI) phase of a project to develop a patient reported outcome measure, highlighting important areas of discussion, difficulty and dilemma surrounding sex after surgery. The project was conceptualized, led and delivered by patient-researchers with support from clinician mentors.
METHODS
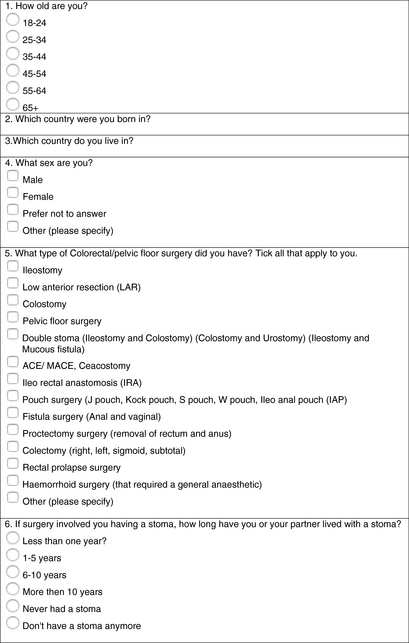
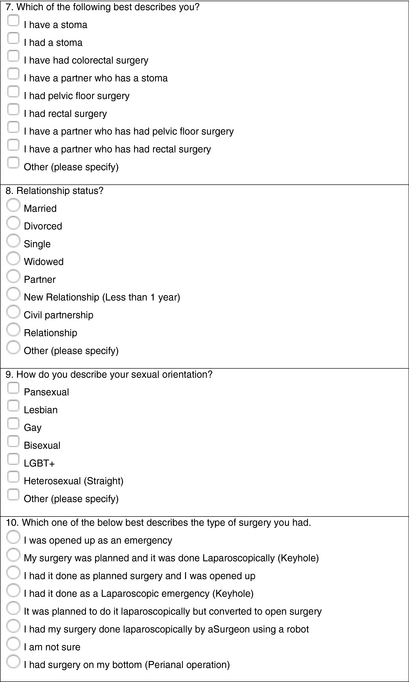
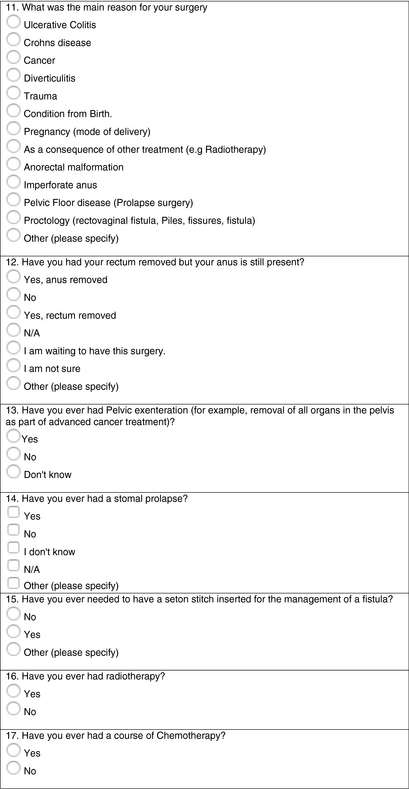
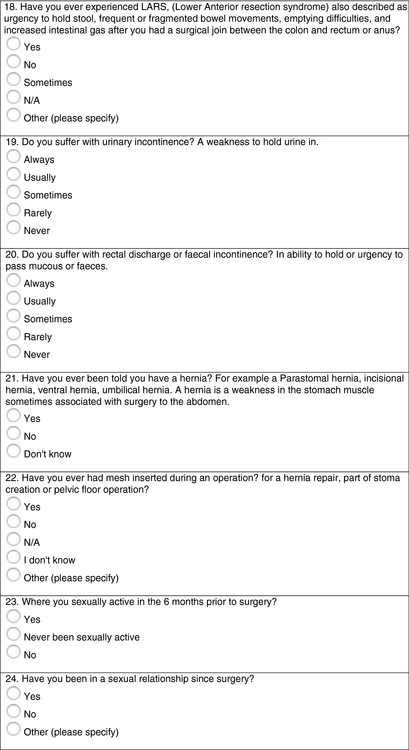
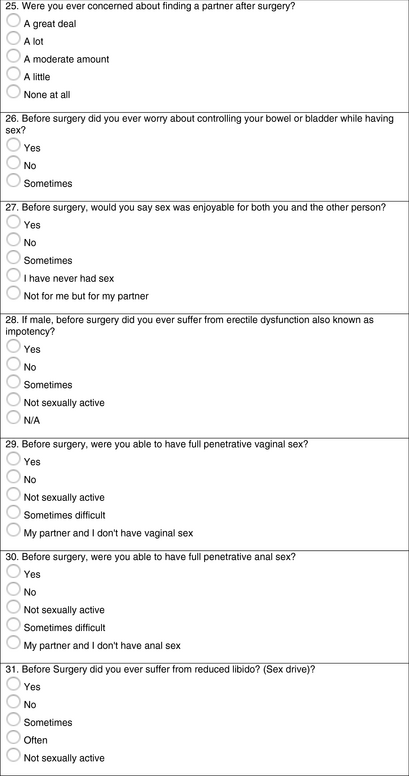
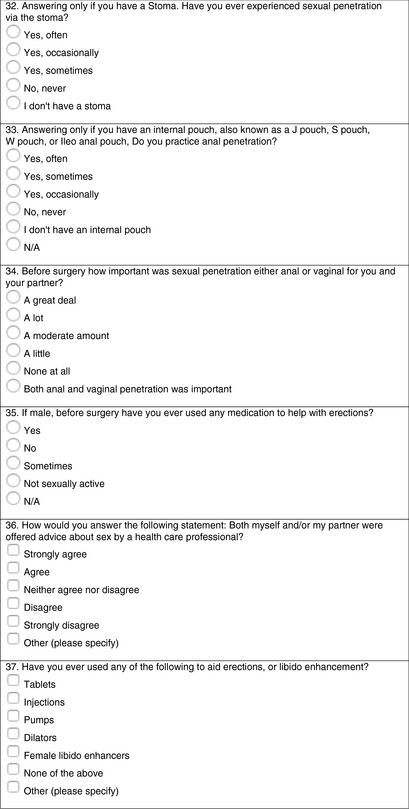
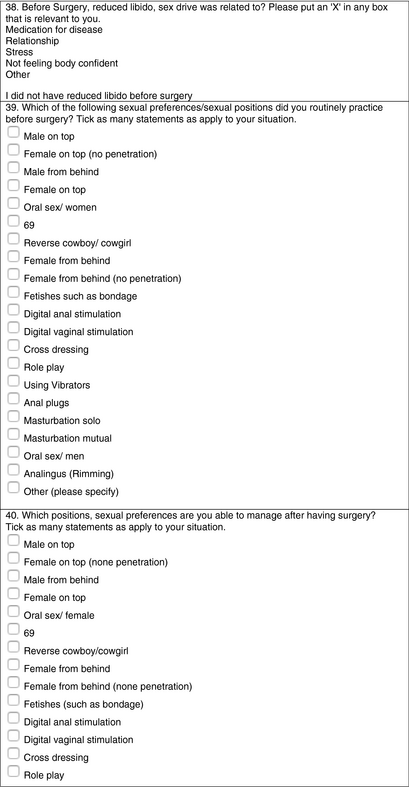
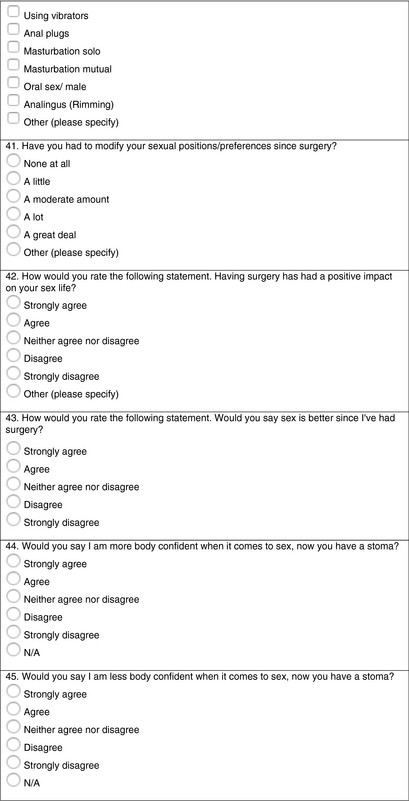
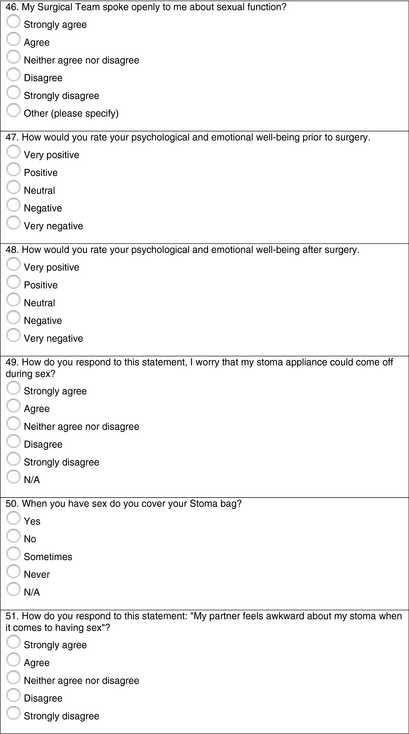
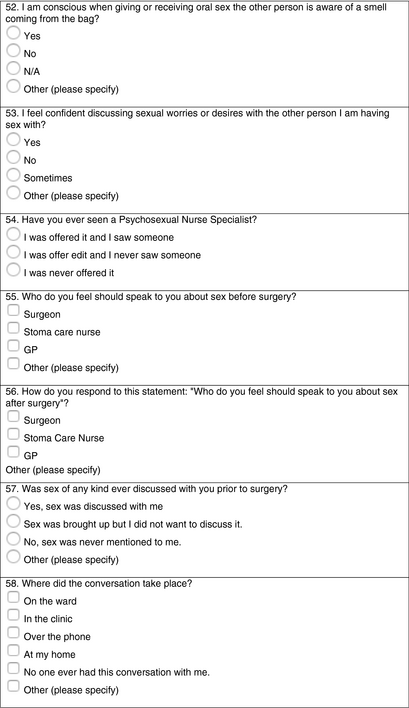
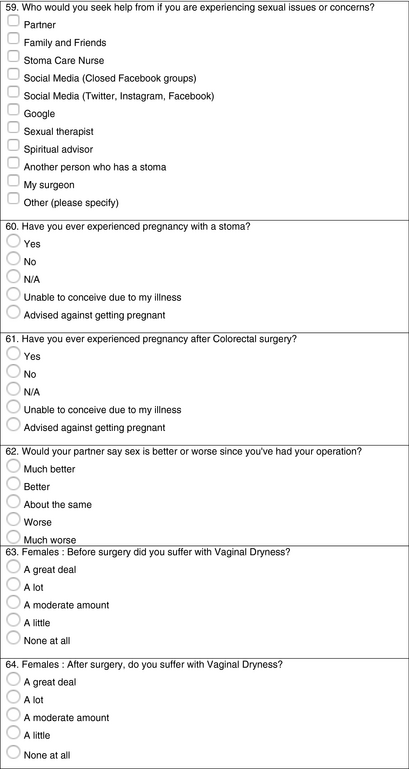
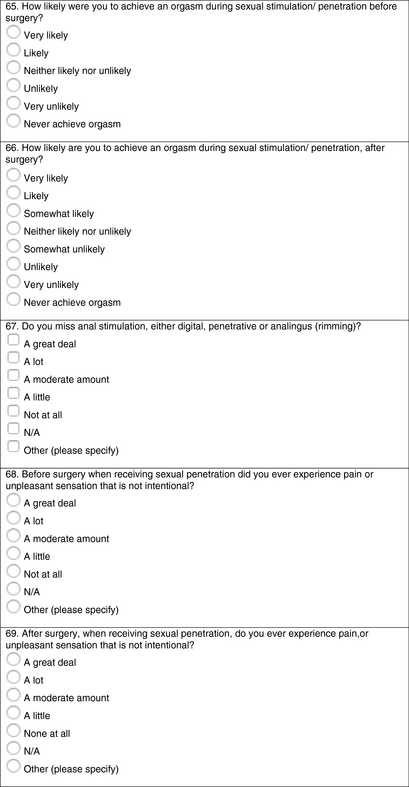
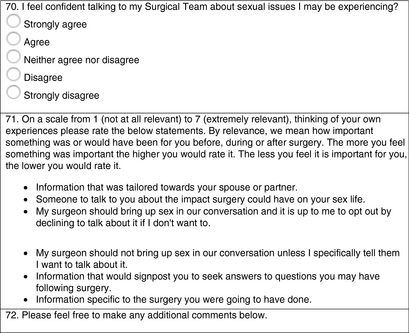
Our primary objective was to perform a patient delivered survey. Using the web based CHERRIES checklist [15], we explored and highlighted the questions which matter most to patients and their partners in relation to sex following colorectal and/or pelvic floor surgery (see Appendix 3).
Ethical approval
No ethical approval could be sought for this PPI exercise since the survey was not carried out from within an institution or organization that has access to a research ethics committee. This is an important point for future consideration for truly patient led and delivered research. The survey represented the gathering of patient views voluntarily by other patients. In the survey introduction, all patients were informed that anonymized answers may be included in peer reviewed publications and consent was implied when participants completed the questionnaire.
ND, SS and BD paid particular attention to the sensitive nature of the survey at the very start (see Appendix 1) making clear that it was strictly for 18 year olds and older due to its explicit nature and content. Extra support and signposting were offered for those who may have been affected by the survey.
Development of the survey
The development and testing process of this survey was performed via an exploratory conversation with a selection of patients that was facilitated by ND on 1 December 2019 via Facebook Messenger. ND invited 20 people across four different patient association groups on Facebook to volunteer their own personal feedback and suggestions to questions about sex after surgery. ND selected invited participants based on their personalities, openness to sensitive topics such as sex after surgery, their network of patient reach and their reputation within the community. Each selected participant was verified by ND based on their history of dialogue and advocacy within the patient community. ND later invited SS and BD, both with experience of PPI, and together they used the primary feedback from the pilot study focus group to develop a 72-question survey which was disseminated on social media.
SM, JP and CB, and later PT, JC and RF, were subsequently invited to be mentors and provide guidance through the process of this PPI work. The mentors offered advice and input only, with all decision making and analysis performed by the patients themselves.
Survey publicity and participant recruitment
A Twitter account (@colorectalsex) was set up by ND with careful attention to the logo, a clear concise bio and regular teaser/taster tweets to build a network of followers from both the patient and the surgical community. Within a few days, over 400 people became followers. The Twitter account formed the platform from which the final survey was launched. As well as using the @colorectalsex Twitter account, all authors tweeted and retweeted a link to the survey from their own accounts. Patient associations and groups such as Purple Wings, Making Ostomies Cool, Ostomy Lifestyle Athletes, Ileostomy and Internal Pouch Association (Birmingham) and Stoma in a Tea Cup all shared a link to the survey on their groups.
Data collection and analysis
Participants completed the survey via an anonymous link. The survey was closed after 3 days. The results were shared with the entire research team via analysis links within the Survey Monkey platform. Free text comments were reviewed by two of the authors (ND and BD) and thematically coded using narrative analysis [16].
RESULTS
Demographics
Some 632 individuals completed the survey. Demographic, disease and surgical data are shown in Table 1. In the 540 (85%) patients for whom a stoma was formed, over half of these patients (51%, n = 324) lived with their stoma for 1–5 years.
| Age | % (n) | Gender | % (n) |
|---|---|---|---|
| 18–24 | 6.5% (41) | Male | 19.3% (122) |
| 25–34 | 27.1% (171) | Female | 80.2% (507) |
| 35–44 | 31.3% (198) | Other | 0.5% (3) |
| 45–54 | 22.5% (142) | ||
| 55–64 | 10.2% (65) | ||
| 65+ | 2.4% (15) | ||
| Type of surgery | Reason for surgery | ||
| Ileostomy | 71.7% (451) | Ulcerative colitis | 34% (214) |
| Proctectomy | 39.8% (250) | Crohn's disease | 31.2% (196) |
| Colostomy | 20.5% (129) | Cancer | 17.3% (109) |
| Colectomy (right, left, sigmoid, subtotal) | 20% (126) | Diverticulitis | 1.9% (12) |
| Fistula surgery (anal and vaginal) | 16.7% (105) | Proctology (rectovaginal fistula, piles, fissures, fistula) | 1.9% (12) |
| Ileoanal or Kock pouch | 12.4% (78) | Condition from birth | 1.8% (11) |
| Pelvic floor surgery | 23.8% (33) | Trauma | 1.4% (9) |
| Double stoma (ileostomy and colostomy) (colostomy and urostomy) (ileostomy and mucous fistula) | 4.3% (27) | As a consequence of other treatment (e.g., radiotherapy) | 1.1% (7) |
| Lower anterior resection | 4.1% (26) | Pelvic floor disease (prolapse surgery) | 0.8% (5) |
| Ileorectal anastomosis | 2.9% (18) | Pregnancy (mode of delivery) | 0.6% (4) |
| Haemorrhoid surgery | 2.5% (16) | Anorectal malformation | 0.5% (3) |
| ACE/MACE, caecostomy | 0.2% (1) | Imperforate anus | 0.2% (1) |
| Other (please specify) | 11.5% (72) | Other (please specify) | 7.3% (46) |
Note
- Some individuals indicated more than one surgery type and these were recorded as they reported them; e.g., proctectomy and colostomy.
- Abbreviation: ACE/MACE, antegrade colonic enema/Malone antegrade colonic enema.
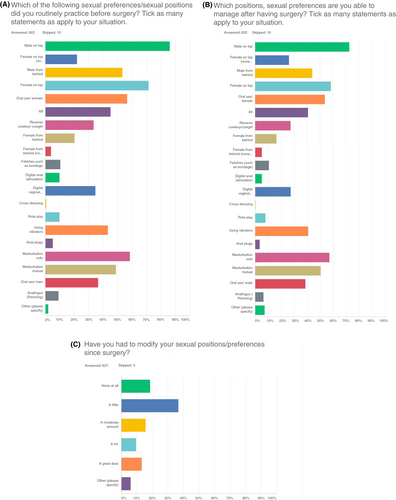
Impact of surgery on body image, sexual practices and pleasure, and on psychological and emotional wellbeing
Fifty-four per cent of respondents described that they lacked body confidence to a moderate or strong degree following ostomy surgery. Surgery tended not to have a positive impact on respondents' sex lives, with 46% of respondents disagreeing or strongly disagreeing that having surgery had a positive impact, and 29% indicating no significant difference. The frequency of different sexual positions amongst the respondents before and after surgery is shown in Figure 1. More than a third (37%) of respondents reported modifying their sexual positions at least a moderate amount following surgery.
However, whilst some respondents described a negative impact of surgery on their enjoyment of sex, others described how sex improved following surgery or how they still enjoyed a fulfilled sex life with some adjustment.
When asked about their psychological and emotional wellbeing before surgery, 30% declared it as positive, rising to 35% after surgery. Almost no one (1.42%, n = 9) met a psychosexual nurse specialist around the time of their surgery.
Comments from respondents from the free text space in this section of the survey, discussing the impact of surgery on body image, sex and wellbeing, are found in Table 2.
| ‘I have been married 32 years and had my operation almost 10 years ago. We have always had a very loving and caring relationship with my husband…. After surgery we had fun talking and exploring sex. I think it helped me to know I’m loved and therefore we were in it together’ |
| ‘Things have improved a lot in the 7 years since my surgery, for both my partner and I…. I'm no longer so focused on penetration and there is a lot more enjoyment and a lot less anxiety about sex…. This more relaxed attitude has also helped alleviate some of the physical problems, which makes sex nowadays a lot more positive and confidence boosting’ |
| ‘My hubby's always made me feel beautiful and sexy with a stoma or a J-pouch or with my scars and that's what makes our sex life work and gives me confidence’ |
| ‘Having a bag has made me more confident about my body image but fistulas/setons have made it harder. Setons are hard to explain to new partners, whereas bags are quite simple and people have heard about them…. I have a fistula that runs very close to my vagina internally and when I have a collection it makes penetrative sex too painful. My upcoming proctectomy will remove this problem but it's a big worry as to how sex will be after that’ |
| ‘I was due to have pelvic clearance and was only told about the impact on my sex life and vagina the week of the surgery. It has impacted my life incredibly. … I am not confident and have found it difficult with new sexual partners…. Life is extremely difficult since the cancer’ |
Information from and discussion with clinicians regarding sex after surgery
The overwhelming majority of respondents (79%) disagreed or strongly disagreed with the statement that they had been offered advice about sex by a healthcare professional (Figure 2a). Most either disagreed or strongly disagreed that their surgical team had spoken openly to them about sexual function. When asked who they felt they should speak to before and after surgery about sex, most (72% and 83% respectively) said it should be with a stoma nurse (Figure 2b,c). However, 78% reported that sex was never mentioned prior to surgery. As well as stoma care nurses (SCNs), 302 respondents (48%) felt that their surgeon should include sex in discussions concerning the impact of surgery. These two professional groups were also the people patients felt should speak to them about sex after surgery (83% SCN and 48% surgeon).
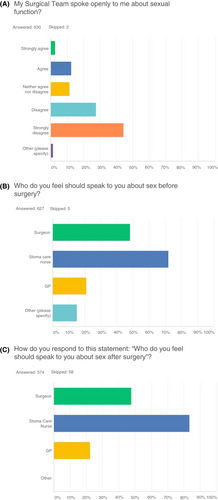
Comments from respondents from the free text space in this section of the survey are found in Table 3. Many comments from respondents highlighted the difficulties of accessing information about the impact of surgery on their sex life. Respondents described being unaware preoperatively of the impact surgery might have and how the issues around sex were not discussed unless they were raised by patients themselves. Several comments described having to find alternative sources of information, for example through social media groups. Additional free text comments from respondants can be found in (see Appendix 2).
| ‘… there were many complications when the stoma was reversed resulting in six surgeries. …erectile dysfunction and lately I have been experiencing retrograde ejaculation. … I just wish someone had warned me of the potential sexual implications just to be more ready’ |
| ‘I'm so glad someone is researching this. … I'm furious that clinicians have never raised the subject with me and I thought it was my fault sex hurt so much’ |
| ‘I had my surgery at 18 (5 years ago) and sex/body image was NEVER discussed with me. It would have been awkward I'm sure but it is so important’ |
DISCUSSION
Following colorectal and pelvic floor surgery, sexual function remains an infrequently discussed quality of life measure for patients. After surgery, more than half of patients surveyed described having significant issues with body confidence, over a third reported changing their sexual practices at least moderately and almost half described enjoying sex less than before surgery. Given this burden, it is perhaps even more concerning that, of the patients surveyed, only one in five patients felt they had the opportunity to discuss sex after surgery with a healthcare professional.
The impact of surgery on sex carries implications for consent and preoperative expectations and is important for patient decision making, as highlighted in the General Medical Council Decision Making and Consent guidelines [17]. This guidance highlights that it is the doctors' duty to find out what matters to individual patients and explain the potential consequences of all treatment options.
Given the prevalence of sexual dysfunction following colorectal and pelvic floor surgery, and the impact that patients have reported this has on their emotional wellbeing, this conversation is imperative both before and after surgery in order for patients to make appropriate personal choices regarding their care and to manage postoperative expectations. Our study has highlighted that many patients would have benefited from a considered discussion with a member of the surgical team about this, with some patients even feeling that this was consciously omitted due to perceived ‘awkward[ness]’ or even feeling that ‘no-one seemed interested’.
For more than one in three patients undergoing colorectal surgery, compromises were made regarding sex, such as a change in favoured positions, due to pain, altered anatomy or function including perceived smell or hygiene (e.g., ‘penetrative sex too painful’, ‘unable to achieve an erection’). For a small number of patients, surgery has ultimately become a barrier to intercourse or sexual intimacy. For example, particularly as one LGBTQ+ (lesbian, gay, bisexual, transgender and queer+) patient described: ‘because I am gay it [sex] was completely overlooked…. I can't have anal penetration anymore’, and as another noted ‘as a gay man I do worry about having a proctectomy…. I feel there is little/no information or support for gay people.’ Arguably, lack of a sensitive discussion about what a patient may experience sexually post-surgery, led by a surgeon or SCN, may compromise the whole notion of whether consent was ever appropriately sought or given.
The authors believe this issue to be at the heart of why we embarked on this study. Do we as patients need to get better at asking the questions? Or do clinicians need to offer an opt-out approach to topics around sex after surgery so that each person gets the same level of information unless they decide not to continue the conversation? Qualitative work to understand how a wide cross-section of patients want to discuss sex, including how to initiate, signpost and explore the sex conversation, where it should be held, by whom, when and, importantly, when not, is a crucial next step.
Respondents were more likely to report that conversations around sex should be instituted by stoma nurses rather than by surgeons (83% vs. 48%). This is perhaps due to the predominant gender disparity of survey respondents and stoma nurses (both mostly women), or due to the nature of the relaxed relationship which develops over time between patients and their stoma nurse. Further investigation of this question is important and might include a more representative sample of patients undertaking the survey (including more men and older women), a detailed qualitative investigation of patients' views on who they would prefer to have these conversations with and why, and an assessment of SCNs' and surgeons' communication skills around sex.
To our knowledge this PPI work is the first in this field to be entirely devised and delivered by patients. The language, tone and publicity surrounding the survey were all inevitably patient centred; therefore ethical approval via orthodox means was not necessary or applicable as this study was led primarily by non-institution affiliated patients, and PPI work does not require ethical approval.
The limitations of this work include the nature of the survey and the recruitment method. The survey was developed by a small team using the advice gained from pilot work with a small group of patients. None of the authors has specific qualitative research expertise. Recruitment was biased in a number of ways: first, social media platforms were used to recruit patients which may influence the age and social status of respondents [18]; second, the authors and their contacts are more heavily involved in ostomate advocacy regarding their own underlying health conditions, which may have led to a high proportion of respondents having stomas; third, the majority of respondents were young women, and the relevance of our findings to older women and to men is unclear. Further work should be performed to ensure a cross-section of gender, age, ethnicity and sexuality to ensure the generalizability of findings.
Some patients noted via free text that some of the question wording was confusing, particularly where patients had had multiple operations and were not sure if the question related to their first operation, most recent operation, or was a more general overview of their postoperative experiences. The inclusion criteria were also broad with the intention of being an inclusive study for all colorectal and pelvic floor patients; however (for example), most published data on sexual dysfunction exists for cancer patients [19-21]. Further focused work on patients with benign disease may demonstrate differences in the form of dysfunction identified by patients [22-24].
We have shown that there is a mismatch between what patients say they want and what some healthcare professionals provide. Important decisions regarding surgery are being taken without discussion of sex, which is both crucial to quality of life for many patients and likely to be severely affected by some colorectal and pelvic floor operations. We suggest that early use of sexual dysfunction screening tools (such as the National Institutes of Health Patient-Reported Outcomes Measurement Information System or the International Index of Erectile Function) [25] may encourage early discussion and encourage patients to seek help if delayed onset sexual problems arise [26]. A limitation of the existing screening tools for the authors, however, is around the wording used, whether they are designed to be filled in by patients alone or with a researcher, and how they were developed (particularly emphasizing the role, if any, of patients).
The development of a sex-based patient reported outcome measure is vital for patients and clinicians, with implications for patient consent and treatment choices, clinician training and information delivery, as a tool for measuring patient satisfaction in interventional studies and for the management of sexual dysfunction postoperatively. This PPI study has initiated the conversation about sex for patients and clinicians, in an attempt to address a taboo subject. We hope that this discussion around sex will encourage healthcare workers to first discuss sex with their patients more freely and frequently and second to consider the language they use when discussing sex after surgery. By normalizing talking about sex, the quality of life for patients after surgery will be improved.
ACKNOWLEDGEMENTS
ND, SS and BD conceptualized and created the study design. ND convened and administered a pilot study focus group. In addition, SM, JP, CB, JC, PT, RF all contributed to the survey design as mentors. It was very important to us that the survey remained patient led from its inception. Data were collected via Survey Monkey and internet links to the results were sent to all authors. ND, SS, BD, CB, RF and PT assisted with drafting the manuscript and approved the final version for submission. The Authors wish to express their sincere gratitude to the Association of Coloproctology Great Britain & Ireland (ACPGBI) for supporting members of the Patient Liason Group (PLG) and funding to enable Open Access.
CONFLICT OF INTEREST
All authors declared no conflicts of interest.
AUTHOR CONTRIBUTIONS
The authors would like to express their gratitude to our other mentors: Professor Susan Moug (SM), James Park (JP) and Julie Cornish (JC). The authors would also like to thank all the patients and healthcare professionals who provided input to the survey: SCN Mark Johnson, Professor Nils Habbe and Gianluca Pellino, as well as all the patient charities who shared our survey on their social media pages also the Association of Coloproctology of Great Britain and Northern Ireland (ACPGBI) and the Bowel Disease Research Foundation (BDRF) who also shared our survey. All three patients have extensive experience within the ostomy community and have been involved in a number of colorectal research studies as PPI members.
APPENDIX 1
Let's talk about sex baby
SEX AFTER COLORECTAL AND PELVIC FLOOR SURGERY(SACS)
You are being invited to take part in a proposed study. We are looking for patients who have had bowel or pelvic floor surgery to participate. Before you decide whether or not to participate, it is important for you to understand why this study is being done and what it will involve.
Please take time to read the following information carefully and decide whether or not you wish to take part.
Discussions about bowel, bladder or pelvic floor habits and/or symptoms can cause embarrassment and shame to the person, if you add in the impact these issues can have on your sex life. That shame or embarrassment may not only affect you but the people closest to you also.
Whenever someone undergoes colorectal or pelvic floor surgery, their sex life may resume but could also change. We do not fully understand the reason for this, but they may experience symptoms that are both physical and psychological in nature.
The main aim of this study is to guide a future piece of research using patient input from the start. We want to find out what these issues are that matter to people and their partners who undergo colorectal/pelvic floor surgery with a particular focus on sex and the impact surgery may or may not have.
Using these results we will undertake further work to define the key outcomes, which matter to patients following surgery, and to develop a validated PROM (patient reported outcome measure) specifically around sex, that can be used as part of a patient pathway for bowel/pelvic floor surgery. This will help surgeons and patients understand the impact on a patient's sex life.
We are very aware that completing this survey will involve recalling memories that may evoke lots of emotions; equally we hope that involving the person closest to you will also allow for an opportunity to have an open discussion about the topic.
If for whatever reason you feel you would like to speak to someone or seek further advice please do not hesitate to contact the support organizations below.
Colostomy UK: http://www.colostomyuk.org/
PRDA: http://www.prda.org
Ileostomy Association: https://iasupport.org/
Bowel & Bladder UK: https://www.bbuk.org.uk/
Bowel Cancer UK: https://www.bowelcanceruk.org.uk/
The survey is intended for those 18 years and older due to the explicit content.
The answers you give will be anonymous. We will not be asking you for any identifying information that will link your answers to you, such as name or email.
If, however, you feel we have not asked any questions that really matter to you, please feel free to add this into our free comment textbox. Please note, this will also be anonymous.
Thank you.
Nicola Dames (Patient and Lead Researcher)
Sarah Squire (ACPGBI_PLG Member) Association of Coloproctology GB and Ireland
Anthony Devlin (Lay Representative)
Special thanks to the colorectal and pelvic floor surgeons as well as stoma care nurses for their guidance and support.
APPENDIX 2
|
Sex after surgery and a bag has never been raised and I wish it had. 12 April 2020 3:09 PM |
|
Post-surgery my nerves were damaged so too painful to have sex. 16 March 2020 3:18 PM |
|
My surgery was 30 years ago, when people had not really heard of Crohn’s disease. Very little information was given to me about anything and there was no one to talk to; you simply learned what to do when it happened. I am glad things are very different now. ☺ 16 March 2020 2:52 PM |
|
This is a great conversation to have. I had a stoma for 6 months 4 years ago. Unfortunately there were many complications when the stoma was reversed resulting in six surgeries that had a significant impact on my recovery. I experienced hernias, erectile dysfunction and lately I have been experiencing retrograde ejaculation. This all seems to be linked to the number of procedures I had and potentially the medication. As a gay man, I had never considered having children but I have now been offered the option to freeze my sperm since this new condition will only get worse. I just wish someone had warned me of the potential sexual implications just to be more ready. 16 March 2020 1:43 AM |
|
I feel very sad that no one has offered me any support regarding my life now I have a stoma. Mine was after having sepsis after three perforations. I'm still trying to cope with the trauma which I'm also not getting any help with. Unless I am suicidal or going to harm anyone, there is not enough funding to help me. My poor partner too, who is now my carer, is also grieving for the life we once had. His depression has led him to drinking. I hate my life now. 16 March 2020 1:24 AM |
|
Not only do I feel there was limited info given about impact of surgery on fertility (I had IVF [in vitro fertilization] after surgery), I also feel no discussion of sexual issues has ever been broached and I now feel it would be very difficult to raise it with surgeons or a stoma care nurse. It took me many years to understand that the dull pulling, aching and numb feelings I get from penetrative sex are related to my adhesions which have tethered my ovaries and tubes also causing infertility and a small bowel obstruction. I found myself just wanting the banging to stop before my partner could climax and then trying to avoid sex altogether, associating it with pain. I don't know if there is anything that can be done to help or any point in talking about it. It's a mechanical problem which can't be fixed with drugs or feeling body confident or relaxing. I'm scared sex will only be more painful after a proctectomy. 16 March 2020 12:24 AM |
|
I'm so glad someone is researching this. I only learned a few months ago that pelvic pain is common in people who've had colorectal surgery—and I've had lots of surgery, starting before I was sexually active. I'm furious that clinicians have never raised the subject with me and I thought it was my fault sex hurt so much. 16 March 2020 12:04 AM |
|
I had no help from anyone post-surgery. I found the Ileostomy Association in 2007 (8 years post-surgery). I should have been given their information by my stoma nurse. I felt alone before the Ileostomy Association. 15 March 2020 8:34 PM |
|
My surgery—subtotal colectomy with ileorectal anastomoses—was 12 years ago. It was done with keyhole, five entry points, including cutting open a previous c-section scar. I'm not sure if my answers are relevant to recent times. 15 March 2020 8:16 PM |
|
I've had to prompt discussions about sex with surgeons particularly after J-pouch excision as it wasn't clear when it was safe to resume sex afterwards. I was using a Facebook closed group to find out what others did. It would've helped to talk about it pre-excision surgery and also afterwards as part of planned discussion, things to expect. I was able to ask two surgeons afterwards at about 6 and 12 weeks post-excision op about sex. It is very much guided by if you're healed up, comfortable and ready, but it helps to talk about. My partner didn't want to cause me any harm by engaging in sex too soon and it would have helped him to have had some information on this. 15 March 2020 7:59 PM |
|
I had my surgery as a relatively young woman 34 years old. At no time was sex discussed although I had many fears about body appearance and my perceived failure as a woman to the point I declined surgery till I almost died. I was married to my first husband—only sexual partner for 30 years until his death. I subsequently remarried but have never been able to have penetrative sex with my second husband—early menopause due to surgery, scar tissue and no oral sex due to my perceived issues regarding my bag. We still have a very loving relationship but hugely regret I cannot participate in the above. 15 March 2020 7:55 PM |
|
I wish I would have had more sex info. I was told after the small percentage of changes that sexual function could have. I was in that small percent and I felt it was played off and I was not given anyone to speak to. 15 March 2020 7:37 PM |
|
Some of the questions or statements felt awkward due to the wording leading me to be very unsure if it was a statement or a question which changes how I would have answered things. I also feel that you are missing a huge section of research here and that is dealing with trauma that has been caused from having a stoma or having surgery getting a stoma and how friends and family have treated me since learning that I have a stoma. 15 March 2020 5:42 PM |
|
I had colectomy, proctectomy, hysterectomy as separate surgeries. Multiple surgeries in between colectomy and proctectomy related to disease, but sexual function and health have always been affected and never addressed unless I brought it up. Increased blood flow to the areas increased tension and pain to adhesions and it can easily take a mental toll on oneself and their partner thinking they're doing something wrong causing pain. 15 March 2020 5:40 PM |
|
Am very disappointed that radiation treatments completely ruined my previously great sex life. Was told to accept as my new normal. 15 March 2020 3:43 PM |
|
Unable to achieve an erection and unable to ejaculate, But I don't worry about it; at 75 it is great to still be alive. 15 March 2020 3:29 PM |
|
My relationship with my male partner never recovered sexually. Could not cope with the bag. 15 March 2020 9:17 AM |
|
I experienced excessive scar tissue that filled the vaginal cavity due to perforation being cut internally. I used dialysis for over a year before I could have sex at all, and over 2 years before it was no longer painful. I still experience pain with use of rigid toys and during exams due to said scar tissue. I'm told this will never go away. 15 March 2020 5:21 AM |
|
My problems are due to scarring due to cancer being low and outside of bowel… began from a micropore that headed straight outside. So sexual penetration is/was very painful. 15 March 2020 4:04 AM |
|
It's hard to remember everything that the doctor/surgeons said to me when I first had surgery as I was so ill; they should take into consideration that if someone is so ill there should be someone with them when getting told about the surgery or what will happen after surgery. 15 March 2020 3:36 AM |
|
I had my surgery young and had only had one sexual partner for a short period before my surgery. Most answers are based on my post-op experiences with long term relationships. Have been an ostomate for over 30 years. 15 March 2020 2:24 AM |
|
I had multiple laparoscopic surgeries for ostomies before being cut open for a colectomy; the sex I had with an ostomy but before being cut open did not cause any pain whatsoever. 15 March 2020 2:21 AM |
|
I want to clarify that the reason my sex life is better post-surgery is because I am no longer in pain, and I also don't have to worry about incontinence anymore. I am more able to relax now. 15 March 2020 1:52 AM |
|
Things have improved a lot in the 7 years since my surgery, for both my partner and I. Physically there are still problems but I accept them now and work with them. I'm no longer so focused on penetration and there is a lot more enjoyment and a lot less anxiety about sex. My partner's libido has recovered after childbirth and we both enjoy sex a lot more than we used to. This more relaxed attitude has also helped alleviate some of the physical problems, which makes sex nowadays a lot more positive and confidence boosting. 15 March 2020 1:48 AM |
|
No one ever told me about how the tightness of my pelvic floor would change. I found out by searching the internet about it. It's been 4 years since my total colectomy and at times I still struggle with penetration because my muscles are so tight. It's better than it used to be but is still something I wish I had a professional to talk about it with. There is sometimes pain with different positions now that my uterus has shifted and the scar tissue inside can cause pain as well. Having someone to talk about those things and what other experiences to expect post-op (3–6 months out, 1–2 years out etc.) would be very helpful to patients. 15 March 2020 1:27 AM |
|
I am still unsure about the impact surgery has had on my sex life. Having had Crohn's since the age of 10 and then having had two sets of surgery, I am unsure how sex should feel and I just know it has been different following both surgeries. My sex drive has definitely increased since having my rectum removed. I also think I have a loss of sensation upon vaginal penetration since my rectum has been removed. A GP told me fairly recently upon a cervical examination that he could see the vaginal wall had collapsed. This is something I have been concerned about and it has been playing on my mind. 15 March 2020 1:23 AM |
|
I have been unable to have penetrative sex since my surgery. I have seen a gynaecologist with very little impact except to begin to treat my menopausal vaginal atrophy etc. The best things I've done is to find a pelvic physio who recognized that I've been sewn up too tightly so that my pelvic floor is constantly engaged, meaning there is no internal space for sex. 15 March 2020 12:03 AM |
|
Sex is non-existent in my life—had five IBD surgeries now. 14 March 2020 10:50 PM |
|
I had my surgery as a young teenager so my only experience of open intercourse itself has been after surgery. 14 March 2020 10:46 PM |
|
It would have been nice to have been told how having open surgery and an ileostomy could affect the sensation you can get in your vagina during sex and that it could affect your bladder in some way. I also didn't know that it could cause scar tissue in the abdomen meaning sex could be painful when the body tenses up during sex. I no longer have much sensation in my vagina during penetrative sex and can't feel my partner so I don't know if I'm doing things right and he can no longer satisfy me in that way so we have to find other ways. 14 March 2020 10:29 PM |
|
My sex life and libido are currently non-existent—not sure if it's physical or psychological or both—but it's very frustrating and no one cares. Thank you for the study. 14 March 2020 10:23 PM |
|
Thanks for all you and the team do. x 14 March 2020 10:09 PM |
|
Thank you—there should be more conversations happening around sex and an ostomy, although it's not something that happens a lot! 14 March 2020 10:01 PM |
|
Thank you for doing this very important and necessary research. 14 March 2020 10:01 PM |
|
My sex life is over and my hubby is frustrated, as am I. I haven't had any help or advice from any of the stoma team or consultant regarding my operation. Just don't know what to do. 14 March 2020 8:57 PM |
|
My ob/gyn referred me to a specialized physical therapist who had moderate success helping me. Otherwise my situation would not have improved. 14 March 2020 8:50 PM |
|
The whole area of sex and conception is totally ignored. I ended up losing my fertility and I am still struggling to get adequate explanation of my early menopause which I am convinced is directly linked to my stoma surgery and subsequent removal of rectal stump. There seems to be no join up or explanation of the risks. I had surgery as a 19-year-old healthy fertile person. I could have had eggs harvested and frozen. As it is I have adopted a wonderful little girl and I wouldn't change that for the world but it feels like there is a need for much better understanding and information about how this surgery can impact on your sex life and ability to have children. 14 March 2020 8:44 PM |
|
I am happy with the stoma, and it was necessary. My husband won't have sex with me—even with my vanilla blush intimacy underwear that hides the bag. I wish someone had spoken to us before surgery about this. I’m very lonely and feel ugly now, but not because of the stoma itself—but because of my husband’s response. He says it doesn't bother him but he refuses sex. 14 March 2020 8:01 PM |
|
I had my surgery in 1994, lived with an ileostomy for 25 years. Had the rectum and colon removal about 4 years ago. There is not enough discussion. 14 March 2020 7:48 PM |
|
I was due to have pelvic clearance and was only told about the impact on my sex life and vagina the week of the surgery. It has impacted my life incredibly. My husband left me due to this. I have therapy. I am not confident and have found it difficult with new sexual partners. I have had shortening of the vagina and it is difficult and often painful to accommodate a penis. I also am in surgical menopause so have dry vagina. Life is extremely difficult since the cancer. 14 March 2020 7:44 PM |
|
I was aware that I would be having a full anal/colorectal resection but was totally unaware that my surgery would include a posterior vaginal resection until my doctor informed me after the surgery. At that time I was told I may never be able to have a normal sex life again. 14 March 2020 7:31 PM |
|
I have been married 32 years and had my operation almost 10 years ago. We have always had a very loving and caring relationship with my husband. Talking about our feelings and thoughts has been very much part of our relationship. After surgery we had fun talking and exploring sex. I also had a hysterectomy so that had an impact too which only added to exploring new and fun ways to express our love. I think it helped me to know I’m loved and therefore we were in it together. Looking forward to the next 32 years! Woohoo! Interesting survey, let’s get talking! 14 March 2020 6:31 PM |
|
It may have been the most traumatic experience of my life receiving an emergency ileostomy, but I am thankful for it. My mental health has definitely suffered tremendously. 14 March 2020 5:31 PM |
|
After surgery no more erection. 14 March 2020 4:52 PM |
|
This is a topic that is so important to me and I am so grateful to you. I had my colectomy before I’d ever had sex (age 15) and had my proctocolectomy 9 years into marriage. I am a vocal advocate of finding satisfying ways to have sex no matter the situation and I so hope that more patients will have access to safely exploring and feeling supported as they find what works for them. Thank you for this! 14 March 2020 4:29 PM |
|
Thank you for doing this survey. I had my surgery at 18 (5 years ago) and sex/body image was NEVER discussed with me. It would have been awkward I'm sure but it is so important. I am with the same partner that I was with before my surgery, which meant that we could deal with this together and I was supported, but I could have easily not had that. I have heard awful stories from other women who have been in very scary situations post-surgery, and it should be a priority of the team to make sure people are confident after surgery—that they know their worth and don't let people make them feel shit! Thanks again! Loved seeing this! 14 March 2020 3:13 PM |
|
I felt it wasn't geared for people with a urostomy—we are just as important, even more so as we aren't as many. 14 March 2020 2:16 PM |
|
For you to understand my answers better: I had my first stoma surgery as a child and then lived without a stoma and then got another one as an adult. So I have experienced sex with and without a stoma and it is very important for me to have open discussions about the topic. 14 March 2020 2:06 PM |
|
I’ve been married to the same man 31 years, before and after my surgery, and we work together to have a satisfying sexual relationship. My hubby's always made me feel beautiful and sexy with a stoma or a J-pouch or with my scars and that's what makes our sex life work and gives me confidence. 14 March 2020 1:35 PM |
|
I am unable to have sex due to massive scar tissue in my vagina. We have to rely on oral sex to satisfy my husband but I feel very guilty I can't have sex. 14 March 2020 1:20 PM |
|
The impact on the patient's sex life is far greater than simply being told ‘the right person won't mind if you have an ostomy’. The issue is that there are so many people who will reject you for it even if you're body confident. I think the detrimental psychological effect on a person’s sex life and self-esteem is a more significant issue than the physical ability to have sex. 14 March 2020 12:58 PM |
|
I left a horrible coercive control violent relationship and found a new lovely partner and had a few months of joy and then bam this. Now I am a disgusting repulsive stinking creature with a massive pouch vaginal fistula and scars and a huge hernia and just gross. Have to fast to be able to leave the house to work. Will die alone—probably in shit. 14 March 2020 12:37 PM |
|
Some of the answers did not have an ‘Other’ option. I've had numerous surgeries and been in two significant relationships since my first and subsequent surgeries so something’s related to my first relations and some to my second so I didn't feel I answered the questions fully. 14 March 2020 12:21 PM |
|
Having a bag has made me more confident about my body image but fistulas/setons have made it harder. Setons are hard to explain to new partners, whereas bags are quite simple and people have heard about them. Because of setons I have to make sure I'm clean/remove sanitary pads before sex which kills spontaneity. I have a fistula that runs very close to my vagina internally and when I have a collection it makes penetrative sex too painful. My upcoming proctectomy will remove this problem but it's a big worry as to how sex will be after that. Male surgeons talk about sex in relation to fertility when my fertility is so much less important to me than the ability to have pleasurable sex! 14 March 2020 12:19 PM |
|
No one mentioned sex and when I asked my stoma nurse after my surgery, she looked at me strange, like I was mad for even wanting to be intimate with my husband. 14 March 2020 12:05 PM |
|
I feel that because I am gay it was completely overlooked. And that apparently I can’t have anal penetration anymore but I feel embarrassed to bring the topic up again as it is not in line with my surgeon’s culture so I think it would offend and be really awkward but I’m not sure I can take another few years. I just want to connect with my partner again! 14 March 2020 11:29 AM |
|
The wording of the previous question (scale 1–7) wasn't very clear. I'm not sure I fully understand whether you asking me whether I thought I should or should not have the information based on the wording of the first question. I have assumed ‘what information would you want’ was asked. 14 March 2020 11:04 AM |
|
Didn't have sex much before and will probably never have it again. 14 March 2020 10:26 AM |
|
I had stoma surgery aged 16 so I had no sexual experience beforehand. I do think my sensitivity and ability to feel all sensations during sex is less than it would have otherwise been (I've understood that through conversation with friends and partners). 14 March 2020 10:24 AM |
|
We do have to use lube these days, and slightly alter position. I still enjoy sex and climax. My main issue is being too tired to actually get in the mood sometimes, so frequency is linked to that as opposed to anything else. 14 March 2020 9:05 AM |
|
My vagina has ‘fallen back’ since my surgery, sex is far more painful and I have occasional urinary incontinence. Not a lot of fun. 13 March 2020 7:34 PM |
|
I think it is important that I had extreme difficulties after surgery with sex and it took a long while to get to where I am now with it. 13 March 2020 6:06 PM |
|
I’m a male and I miss being anal penetrated fully and that makes sex and orgasm very difficult. Wish I could get that back. 13 March 2020 5:54 PM |
|
I have a new partner since my surgery so some questions will be irrelevant I'm afraid. 13 March 2020 5:15 PM |
|
Proctectomy left me with erectile dysfunction; surgeon just said take a pill. Sadly they don't work for me at present. 13 March 2020 4:31 PM |
|
Neither my general practitioner nor my urological oncology team have provided me with any support or even had the slightest comments as to my reporting my inability to be penetrated sexually without it being agonizing. I have begged multiple gynaecologists, urological oncologist as well as my general practitioner to please refer me to a pelvic floor specialist since no one else is even willing to respond to my sexual complaints. A year and a half later I have still not gotten a referral to a pelvic floor specialist. Not only is sexual penetration agonizing but I have constant pelvic pain and swelling in my legs and feet from the radical lymphadenectomy as well as varicose veins which have caused tarsal tunnel syndrome. Recently even defaecation has become a brutally painful difficult process. I feel there is no support for this for me and frequently fall deeply into despair. 13 March 2020 4:26 PM |
|
Having a stoma took away the spontaneity of sex as I would always want to make sure my bag was empty. I was very conscious of the bag hanging and getting in the way. I eventually got a Level 3 support belt so I could take the bag out of the way, and it was almost like sex prior to surgery again. 13 March 2020 1:45 PM |
|
My vagina was shortened in length due to the cystectomy. Nothing was explained as to how that would impact me, our relationship or what recovery to expect. My uterus was also removed during surgery but this wasn't confirmed prior to surgery taking place. More support afterwards would have been beneficial. 13 March 2020 11:48 AM |
|
My sex life took a nose dive after surgery (as well as removing the tumour, they had to give me a total hysterectomy as the tumour had invaded and attached itself to my Fallopian tube/womb. So as well as surgical/treatment discomfort, I had menopause issues to deal with too. I'm no longer with my partner and choose to remain single. 13 March 2020 11:40 AM |
|
I feel some questions weren't relevant or didn't give a relevant answer, for example questions about how my partner felt before my surgery were not answered honestly as we didn't know each other before my surgery. 13 March 2020 9:44 AM |
|
The stoma makes me feel unattractive, hinders sex. But also the removed surgery has made it somewhat impossible to actually have sex even when trying to. 13 March 2020 8:37 AM |
|
I struggle with erectile dysfunction sometimes and ejaculation is not as pleasurable and is sometimes dry. 13 March 2020 7:29 AM |
|
I find I have people to speak to who tried to come up with solutions; in the end it would include more surgery and no idea of a success rate. 13 March 2020 4:09 AM |
|
I was 22 having ileostomy and transvaginal mesh surgery. I had been with my partner for 4 years at that point. We fought my cancer together. Nothing about sex was mentioned to me. But not only that. I didn’t know a stoma could prolapse, or invert, or get a fistula. No one explained green or slimy output. No one told me anything really. Just what foods I shouldn't eat. I still don’t get support now. My stoma nurse team never have time for me. My surgeon is a waste of space. She wouldn’t listen when I told her not to do the mesh but she did it anyway and now I have complications. I also have pudendal nerve damage so sex is pretty much impossible. And my hand is very damaged from chemotherapy without steroids due to bone rotting complications (AVN) so I can’t even masturbate. My hands are too slow and painful and vibrations are too fast and painful. But no medical professional will help me. I just get asked if I'd like to try antidepressants. And no. No I wouldn’t. 13 March 2020 3:39 AM |
|
Discussion before surgery about what to expect should detail what help is available, i.e. talk to surgeon, nurse etc., and also the availability of physio. This may aid patients to get help sooner rather than suffer in silence. 13 March 2020 2:07 AM |
|
Married 35 years at time of male colostomy fixation. Our sex life has always been good. After surgery, largely due to very good communication between us, resumption of normal sex happened as fast as the surgical wounds healed to allow it. Now married 40 years, sex is satisfying to both partners, and engaged in a minimum of once a week on a schedule, as well as frequent spontaneous sessions as well. We've both always enjoyed it! 13 March 2020 2:01 AM |
|
I wish something like this existed before, to raise awareness to provide insight to help people lost and suffering from the impact. I hope more is done to raise awareness of the pros and cons of surgery and the possibility of issues and direction to services that can help when and if it occurs for people. 13 March 2020 12:44 AM |
|
Q10 wasn't sure if it's referring to most recent surgery as I've had multiple surgeries. Q20 suffered considerably after subtotal. Q62 couldn't answer as partner post-subtotal was a new partner and have not had sex with him post-proctectomy. Q64 have had the total opposite of dryness post-proctectomy. Considerable constant discharge which is awful. I've mentioned this to my GP who didn't really say much about it but going to mention it to my surgeon at my next appointment. Q66 could achieve orgasm post-subtotal but have not had sex post-proctectomy Great survey! Having bowel disease and being an ostomate can be very lonely and isolating; the subject of sex can make it even more so. It's a hugely important subject and think it's something that's, unfortunately, pretty much left to patients to explore themselves with very little guidance of where to go for help if needed, which would be made harder for anyone who isn't confident or open talking about it anyway without the complication of colorectal surgery. It may also be hard from the other side for surgeons/nurses to talk about with patients as they may not be able to gauge how the patient will react if the subject is brought up. I often think my surgeon hasn't brought it up because my Mam is always with me! My surgeon and stoma nurses are amazing and have a great relationship with them. I'm an open and confident person and I've learnt since my first surgery that things like this don't faze them so I wouldn't hesitate to approach them if I was having any issues sexually as I have total faith and trust in them. However, I totally understand that it would be difficult for some people. I actually told my stoma nurses (not in a huge amount of detail) that I'd met someone and had sex post-subtotal as they have played a huge part in my journey and they still do. I feel like I can talk to them about anything, about all my milestones whether big or small. I'm sure that hearing about actual experiences from patients can only help them support other patients. I hope my responses weren't too confusing as my sexual experiences and attitude towards sex differ massively between post- subtotal and post-proctectomy. I've tried to expand as best I can in the notes and hope I haven't been too long winded! I managed to get to the end this time without flicking between apps! Haha 13 March 2020 12:42 AM |
|
Since surgery I've had four partners who all had no issues with my ileostomy. I have lost confidence sexually and worry about leakage and it getting in the way and I don't enjoy sex in the same way I used to. No matter what I've tried I can't shake that worry. 13 March 2020 12:20 AM |
|
I didn't know that colorectal surgery could change the tilt of your sexual organs, and make sex more difficult from certain angles. It would've been nice to know that that was a danger. 13 March 2020 12:07 AM |
|
Sex was never mentioned to me during any of the nine surgeries I've had. This made me feel silly to ask about it. I wanted to ask how soon could I have sex and masturbate but didn’t know who to ask. I hate the sound of my bag rustling during sex or masturbation but no one talks about it so it feels like I'm the only one. My husband says that he doesn’t care about my bag and when I try to cover it up he thinks I must not be enjoying myself. I don’t like going on top now as I hate seeing my bag flap about. I wish more people spoke about it. After my J-pouch removal and removing my anus my vulva was numb and I was terrified it would never return but I had no idea who to ask about it. The feeling returned after a few weeks. When you're really poorly talking about masturbation or sex can seem a bit frivolous like you should be worrying about getting well not orgasms! I'm so happy you're doing this, thank you. x 12 March 2020 11:56 PM |
|
I had treatment before my tumour removal surgery so I believe radiation therapy caused my vaginal stenosis and now I fear my sex life is over. 12 March 2020 11:27 PM |
|
As I had emergency surgery it did not cross my mind that things would change. However, having to also have a hysterectomy was a shock. I think my cervix was removed and that I feel affected my ability to feel the deep orgasm I was used to. As it was emergency surgery my sexual feelings did not cross my mind. 12 March 2020 11:27 PM |
|
I really felt lost after surgery. I met my current partner 7 months after surgery so he has never known me any differently but I had concerns that were difficult to talk about at the time; just feeling grateful to be alive made me feel I shouldn't discuss something that didn't feel important in the bigger picture of things. 12 March 2020 11:25 PM |
|
I feel that sex isn't talked about enough when deciding to have a surgery like this. I didn't really have anyone to ask my questions to and kind of felt a little out in left field. 12 March 2020 11:14 PM |
|
I was 14 when I had an ileostomy. I was not sexually active prior to surgery. I subsequently had an ileoanal pouch. I am now married with a 7 year old conceived naturally and delivered by c-section. I am 45 years old. 12 March 2020 11:09 PM |
|
When I did speak to stoma nurse about sex and self-confidence she told me I should feel lucky that I had got through the operation and had a life again. 12 March 2020 10:59 PM |
|
The question about have I experienced pregnancy before and after a stoma, I answered yes to both as I had emergency surgery for a stoma when I was 26 weeks pregnant so I was pregnant when I had the surgery and continued my pregnancy after the surgery. 12 March 2020 10:39 PM |
|
Thank you for this! I want to add that the vaginal dryness I experience is linked to the hormonal change that is rooted in the destruction of my ovaries by radiation. I am in hormonal treatment since 2 years now. But I feel pain during penetration that is not caused by the dryness. My gynaecologist says it has to be psychological because she can't find any problem. It feels like my vagina is right up closed and it would be impossible to penetrate. After climaxing via oral stimulation and by starting slowly in heavy pain it gets better and better until it's completely fine but not completely painless. Funny that all the positions but the missionary position are working. This one is just impossible even later when it feels good. Thank you for working on this! 12 March 2020 10:36 PM |
|
After surgery I had rectal stump blow out and after proctectomy developed a perineal vaginal fistula that needed four surgeries, the latest being a big operation to take muscle from buttock and thigh and put in pelvic dead space. I have had difficulty with pain during sex since. 12 March 2020 10:09 PM |
|
Thank you for this research. This is something I wasn't prepared to struggle with post-surgery once I started feeling better and it's wearing on my mental health and positivity I've achieved thus far post-op. It is comforting to know that people care about something that continues to be so taboo and want to help improve the lives of patients who undergo such a life-altering process. 12 March 2020 10:14 PM |
|
I had an ileostomy and this was ultimately reversed into an IRA [ileorectal anastomosis]. As a gay man I do worry about having a proctectomy, and I feel there is little/no information or support for gay people and others for whom anal penetration is a principal form of sex. 12 March 2020 9:43 PM |
|
Hi. I have a J-pouch and I love that you are researching this but this question is off the mark. Transgender isn't a sexuality. The options should probably be straight, gay, lesbian, bisexual, pansexual, asexual, other (for instance I'm pan and there should be an option for that). Also the questions are unnecessarily gendered so you should say ‘If you have a vagina’ etc. rather than question for women. E.g. I am a trans man and I have a vagina. I found the survey very confusing and heteronormative, especially the questions about sexual positions. The other thing I found confusing was I have had three surgeries but the questionnaire was geared as if they were asking about one. So I answered the questions about having a stoma, despite not having one any more. And e.g. one was laparoscopic, one was open etc. But thank you for taking the time to research this; I think it's very important. 12 March 2020 9:24 PM |
|
After surgery I'm unable to have sex—it's far too painful. 12 March 2020 9:14 PM |
|
I feel there was an overall lack of information and support prior to and following my surgery. 12 March 2020 9:07 PM |
|
My issues have mainly been due to radiation treatment, which was discussed with oncology consultant prior to treatment and followed up after treatment. 12 March 2020 8:59 PM |
|
This is a vital piece of research. However, speaking personally, it is geared at people sexually active before and after surgery. I was 15 when I had my surgery. Was not sexually active beforehand and not one professional gave me any advice or instruction. Now aged 68, my husband and I have had to ‘make do and mend'! 12 March 2020 8:22 PM |
|
Still have issues, tried pelvic floor physio no better. 12 March 2020 8:21 PM |
|
Surgery and our conditions affect us all differently. I personally have struggled with body image and the impact of my illness when trying to maintain a healthy sexual relationship for over a year now, as pre-proctectomy last summer I had a terrible time with truly horrendous complex anal fistulas and recurrent pelvic sepsis that meant fistulas needed dressing every day, and excessively bled and discharged pus. Since then and particularly following stoma surgery, my sex life hasn't quite recovered out of nerves in general (e.g., is this going to be uncomfortable or painful? Am I going to be rigid or awkward because I'm so out of the swing of it and look quite different now?) and being quite concerned about being too worked up about it all to enjoy it and also for my partner to enjoy it. I otherwise have no issues with body image due to my stoma and love that I have finally regained control of my ability to live life and not be a prisoner in my own body like I used to before. Solving my concerns about my body in the bedroom and sex in general would just be the final piece of the puzzle for me. 12 March 2020 8:19 PM |
|
There seems to be an avoidance about talking around issues relating to sex. I have tried to find answers to the problems I now have but no one seems interested in finding out why or finding a solution for me. 12 March 2020 7:57 PM |
APPENDIX 3
| Item category | Checklist item | Explanation |
|---|---|---|
| Design | Describe survey design | Describe target population, sample frame. Is the sample a convenience sample? (In ‘open’ surveys this is most likely.) |
| IRB (Institutional Review Board) approval and informed consent process | IRB approval | Mention whether the study has been approved by an IRB |
| Informed consent | Describe the informed consent process. Where were the participants told the length of time of the survey, which data were stored and where and for how long, who the investigator was, and the purpose of the study? | |
| Data protection | If any personal information was collected or stored, describe what mechanisms were used to protect unauthorized access | |
| Development and pre-testing |
Open Research
DATA AVAILABILITY STATEMENT
Data available on request from the authors.