Sphincter-sparing surgery for complex anal fistulas: radiofrequency thermocoagulation of the tract is of no help
Abstract
Aim
To compare the rate of failure of radiofrequency thermocoagulation for anal fistula with that of rectal advancement flap in a case-matched study.
Method
Patients who underwent radiofrequency treatment were compared with age- and sex-matched patients with Crohn's disease (CD) who underwent a rectal flap procedure. Fistula features, general characteristics and the main clinical events were recorded in a prospective database. Failure was defined by at least one of following: abscess, purulent discharge, visible external opening or further drainage procedure.
Results
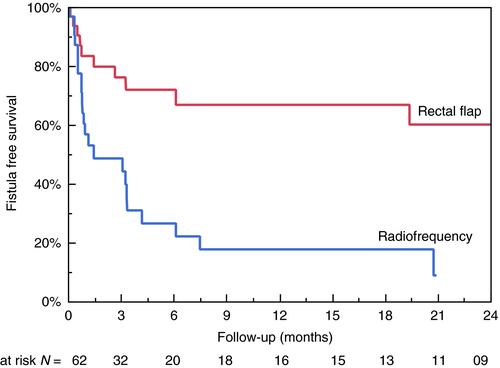
A total of 62 patients [median age 45 (range 36.8–57.5) years; 22 women, 40 men; 22 with CD] were analysed. The failure rate of radiofrequency treatment was higher than that of rectal flap treatment (74.2% vs 32.2%; P = 0.004). The cumulative probabilities of failure of the radiofrequency treatment were 53.8% (38.8–68.3), 71.8% (55.3–84.0) and 87.4% (70.6–95.3) at 3, 6 and 12 months, respectively. Three patients in the radiofrequency group required drainage for an abscess and one had severe thermal ulceration. The Cox proportional hazards regression model (surgical procedure, obesity, CD) showed rectal flap treatment [3.48 (1.60–8.07); P = 0.001] and CD [2.60 (1.16–6.41); P = 0.02] to be the main independent predictors of healing.
Conclusion
Radiofrequency thermocoagulation is a less satisfactory sphincter-sparing treatment for the management of anal fistula than a rectal flap procedure.
What does this paper add to the literature?
In patients with high and/or complex anorectal fistulas, surgeons frequently avoid dividing the sphincter during a fistulotomy. Among the sphincter-sparing procedures, thermocoagulation of the fistula tract seems to be less effective than rectal advancement flap.
Introduction
The therapeutic management of anal fistulas is complex for several reasons, depending, in particular, on the anatomical presentation of the fistula and the presence of Crohn's disease (CD). This is especially true for high and/or complex cases because consecutive surgeries may alter both the sphincter and continence. Strategies with a sufficient risk–benefit ratio for the treatment of anal fistulas are widely debated. The expected benefit is the durable healing of suppuration with a low risk of recurrence. Ideally, the technique is also simple, inexpensive and reproducible, while avoiding the risk of disorders of faecal continence related to sphincter lesions or significant deformation of the anal canal 1, 2. New strategies enter evaluation as soon as there is evidence that they avoid the need for sphincter division (sphincter-sparing surgery). Rectal advancement flap methods are the classic strategies. Other approaches attempt to achieve coagulation or closure of the fistulous tract through heat destruction, occlusion or ligation 3. However, these new methods are mainly case series without any comparative evaluation 4.
Our aim was to compare a new minimally invasive procedure of thermocoagulation of the fistula tract (radiofrequency) with rectal advancement flap surgery in a case–control evaluation. Factors associated with treatment failure were analysed.
Method
Study population
All prospective medical data were recorded between January 2006 and January 2018 in our proctology unit database. The following data were recorded: gender, age, obesity, smoking habit, CD, past medical and surgical history, including sphincter-sparing surgery (fibrin glue, collagen plug, ligation of the intersphincteric fistula tract) and fistula drainage. The characteristics of the fistula were assessed on the day of the surgical procedure: simple/complex fistula, infra- or supralevator fistula, horseshoe fistula or anovaginal fistula. Data for patients with carcinoma fistulas and those with anovaginal or rectovaginal fistulas were not used. Patients who underwent radiofrequency treatment were case-matched with those who underwent a rectal flap procedure according to age, gender and the occurrence of CD.
Study design
This was a case–control retrospective investigation after extraction of selected items from a prospective maintained database.
Rectal-flap surgical technique
Patients were admitted on the day of the intervention and received preoperative prophylaxis (1000 mg metronidazole). With the patient in the Lloyd Davis position, the external opening was enlarged and the fistulous tract excised as far as possible without reaching the external sphincter. The internal opening of the fistula was exposed and the tissue and overlying anodermis excised. Two to three stitches, facing and occluding the internal opening, provided plication of the muscle. Then, the submucosal area was dissected to create a flap with a large buttonhole shape, without acute edges. The plicated muscle was covered with the thus produced mucosal flap. All stitching was performed with resorbable sutures. Sealing of the closure was verified at the end of the procedure. A local anaesthetic block with 150 mg ropivacaine hydrochloride completed the procedure. Occlusion of the tract was verified at the end of the procedure by gentle saline injection through the external orifice. Patients were discharged on the day of the procedure. The rectal flap advancements were performed by the principal surgeon. There was no prior bowel preparation, but analgesics and stool softeners were used during the postoperative period (3 weeks).
Radiofrequency surgical technique
All patients were admitted on the day of the intervention and received preoperative prophylaxis (1000 mg metronidazole). With the patient in the Lloyd Davis position, the surgeon performed a clinical examination that confirmed that drainage was effective and selected the method that would most easily close the internal orifice. If the opening was small, the technique involved a simple mucosal resorbable suture (figure of eight). In patients with a large internal opening, rectal flap advancement was preferred over radiofrequency treatment. Tissues around the fistula were protected from thermal destruction by injection with fresh saline solution around the fistula. The radiofrequency energy was applied along the fistula tract while removing an endovascular flexible probe (radially emitting) from the internal to the external orifice. This strategy is derived from endovascular procedures for varices 4. Energy was delivered every 5 mm with an endovenous radiofrequency source (EVRF®; F Care Systems, Antwerpen, Belgium). Each impact was up to 0.8 s and equivalent to 25 W. The total dose delivered along the length of the fistula tract was calculated. Occlusion of the tract was verified at the end of the procedure using a smooth probe applied through the external orifice. A local anaesthetic block with 150 mg ropivacaine hydrochloride completed the procedure. Patients were discharged on the day of the procedure.
Definitions and follow-up
Obesity was defined by a body mass index ≥ 30 kg/m2.
Complex fistulas were defined as deep trans-sphincteric fistulas, supralevator fistulas, fistulas with an abscess or extension with of the primary tract, low anovaginal fistulas or horseshoe fistulas.
Failure of the procedure was defined as the occurrence of at least one of the following: abscess, purulent discharge, visible external opening or a further drainage procedure. Failure could be observed in the early follow-up, but a minimum follow-up of 12 weeks was requested to distinguish failure and late healing. A medical assessment with clinical examination was conducted at each visit.
Follow-up was defined as the time between the day of the surgical procedure (rectal flap or radiofrequency) and the first assessment of failure or the last visit for patients for whom the procedure was successful.
Statistical analysis
Quantitative variables are presented as medians and percentiles (interquartile range 25% and 75%). Categorical variables are presented as numbers and percentages of the cohort. The data for the radiofrequency group were compared with those for the rectal flap group. The main outcome was failure of the surgical procedure, confirmed by the persistence of the fistula tract. The cumulative probabilities of surgical failure were estimated from the day of the evaluated procedure (at referral) to the occurrence of failure using the Kaplan–Meier method with 95% confidence intervals (CIs). Factors associated with failure of the cohort were identified by univariate analysis using the log-rank test. The results are shown as hazard ratios (HRs) with 95% CIs. Independent predictors of each outcome were identified by multivariate analysis. All significant variables with P < 0.1 in the log-rank test were retained and integrated into a Cox proportional hazards regression model for surgical failure. The results are shown as HRs with 95% CIs. Statistical analyses were performed using jmp pro 13.2 software (SAS Campus Drive Cary, North Carolina, USA).
Ethical considerations
The purpose of the database was to facilitate enrolment in prospective trials and retrospective assessments of therapeutic strategies in several fields of colorectal pathogenesis. This database was approved by the Commission Nationale Informatique et Liberté (CNIL, no. 1412467). Authorization for use of radiofrequency was obtained from the Agence Nationale de Sécurité du Médicament et des Dispositifs Médicaux (ANSM, no. DMDPT-BLOC/MM/2016-A01107-44).
Results
Study population
Among 633 patients with anal fistulas identified from the prospective database, 87 underwent at least one rectal anal advancement flap procedure and 31 underwent a radiofrequency thermocoagulation procedure. Among the 87 patients who underwent the rectal flap procedure, 31 were case-matched according to the presence of CD, gender and age. The characteristics of the population are summarized in Table 1. The fistula tracts were complex in all except three cases. Three patients had simple direct trans-sphincteric tracts that could be treated by fistulotomy. All these three had an anteriorly placed fistula which increased the risk of faecal incontinence. Two patients were already incontinent before the procedure. Anterior tracts were reported in ten cases (five in each group). All patients had prior drainage with inserted setons. The median duration of the fistula before referral was approximately 2 years and one-third of the population had experienced a previous sphincter-sparing procedure before referral. CD was reported for 22 patients (35.5%), but all were in remission at the time of surgery: they all received anti-tumour necrosis factor alpha (anti-TNFα).
| Variables | Population (n = 62), no. (%) or median [IQR 25–75] | Rectal flap (n = 31), no. (%) or median [IQR 25–75] | Radiofrequency thermocoagulation (n = 31), no. (%) or median [IQR 25–75] | P-value |
|---|---|---|---|---|
| Female/male | 22/40 (35.5/64.5) | 11/20 (35.5/64.5) | 11/20 (35.5/64.5) | |
| Age at surgery (years) | 45 [36.8–57.5] | 44 [35.1–57.5] | 45 [37.3–57.7] | |
| Obese | 6 (9.7) | 1 (3.1) | 5 (16.1) | 0.09 |
| Crohn's disease | 22 (35.5) | 11 (35.5) | 11 (35.5) | |
| Smoking | 18 (29.0) | 10 (32.3) | 8 (25.8) | 0.52 |
| Fistula follow-up before the procedure (months) | 22 [11–50] | 25 [10–39] | 21 [12–64] | 0.9033 |
| No. of fistula drainages before the procedure | 3 [1–4] | 3 [1–4] | 3 [1–4] | 0.25 |
| Sphincter-sparing surgery before rectal flap/radiofrequency | 21 (33.9) | 12 (38.7) | 9 (29.0) | 0.42 |
| Characteristics of the fistula at time of surgery | ||||
| Simple/complex | 3/59 (4.8/95.2) | 0/31 (0/100) | 3/31 (9.7/90.3) | 0.07 |
| Anovulvar fistula | 10 (16.9) | 5 (16.1) | 5 (16.1) | 1.0 |
| Length of the fistula (mm) | – | – | 30 [20–38] | – |
| Closure of the internal orifice | – | – | 28 (90.3) | – |
| Delivered energy (J) | – | – | 1225 [981–1781] | – |
| Delivered energy in J/length of the fistula | – | – | 53 [41–61] | – |
| Duration of the surgery (min) | 30 [29–36] | 35 [30–45] | 30 [25–30] | 0.0031 |
| Healing rate and follow-up | ||||
| Failure of the rectal flap/radiofrequency | 33 (53.3) | 10 (32.2) | 23 (74.2) | 0.004 |
| Duration of the follow-up (months) | 5 [3–27] | 23 [5–45] | 4 [2–5] | 0.0023 |
Procedure
The median duration of the procedure was 30 min: it was significantly longer for rectal flap than for radiofrequency treatment (Table 1). Closure of the internal part of the tract was effective in all rectal flap and 28/31 radiofrequency procedures. The length of the tract was precisely measured during the radiofrequency but not the rectal flap procedure. There were no intra-operative complications. Significant secondary effects were reported in three patients (two abscesses and haemorrhoidal prolapse) after rectal flap and five patients (three abscesses, one haematoma and one thermic ulceration with rectovaginal fistula) after radiofrequency treatment.
Follow-up evaluation
The median follow-up after referral was 5 (3–27) months. The median follow-up was significantly longer for the rectal flap group [23 (5–45) months] than the radiofrequency group [4 (2–5) months] due to the recent development of the radiofrequency procedure (Table 1). After a median follow-up of 5 months, the global failure rate was 10/31 (32.2%) in the rectal flap group and 23/32 (74.2%) in the radiofrequency group (P = 0.04). The cumulative probability of surgical failure is shown in Fig. 1. The cumulative probabilities of failure rate of rectal flap advancement were 18% (9.0–32.8), 22.9% (12.3–38.6), 28.8% (16.2–45.8) and 35.7% (20.5–54.5) at 3, 6, 12, and 24 months, respectively. The cumulative probabilities of failure rate of the radiofrequency procedure were 53.8% (38.8–68.3), 71.8% (55.3–84.0) and 87.4% (70.6–95.3) at 3, 6 and 12 months, respectively. The differences were highly significant (P = 0.0004). Failure occurred very early in the radiofrequency group as 15/31 (48%) had a recurrence within the first month of follow-up and 20/31 (65%) within the first 2 months of follow-up. Univariate analysis using the log-rank test to identify factors associated with failure of the global cohort showed three main factors to be associated with a higher failure rate: the radiofrequency procedure [3.59 (1.73–8.02); P = 0.0004], obesity [3.18 (1.17–7.40); P = 0.026] and the absence of CD [2.68 (1.25–6.40); P = 0.01]. The fistulas of obese subjects did not heal, regardless of the type of surgical procedure. The fistula tracts of patients with CD healed in 14 of 22 (63.6%) cases. None of the following factors were associated with less favourable healing rates: age, gender, tobacco consumption, past surgical history and type and complexity of the fistula. The Cox proportional hazards regression model (three independent variables included in the model: surgical procedure, obesity, CD) showed rectal flap [3.48 (1.60–8.07); P = 0.001] and CD [2.60 (1.16–6.41); P = 0.02] to be the main independent predictors of healing.
Discussion
We quantified the failure rate and assessed predictive factors for the use of sphincter-sparing surgery for anal fistulas. Sphincter-sparing surgical options are usually offered in patients with high fistula tracts because fistulotomy can lead to faecal incontinence. In this tertiary centre, different strategies have been developed over time and the main goals are that treatment should be minimally invasive and sphincter division should be to avoided. Rectal flap has remained a common strategy over time as other recent techniques have failed to provide satisfactory results in our hands. Due to the retrospective nature of the study and the historical evolution of minimally invasive techniques, treatment selection was mainly based on the opportunity (or not) of offering a new strategy. This is the first evaluation to compare radiofrequency thermocoagulation with a classic strategy (rectal flap advancement).
The main strengths of this study were the sample size, systematic clinical evaluation by experts in the field of proctology and technical homogeneity of the surgery. The data were recorded in a prospective database using recommended classifications. In CD patients, disease characteristics and both therapeutic and surgical strategies were recorded. Finally, the study was a case-matched comparative evaluation with rectal flap advancement in a single tertiary referral centre.
This study also had several limitations. The study design was a retrospective analysis of a prospective database. In addition, this study was performed in a tertiary referral centre, which may have resulted in selection bias in the recruitment of patients. Magnetic resonance imaging (MRI) was not performed for all consecutive patients, and thus these data could not be assessed. Indeed, assessment under general anaesthesia may be as useful as MRI, but neither ultrasound scan nor MRI is currently recommended before rectal flap advancement surgery. The median follow-up was short because the tested procedure is new, but this did not have an impact because recurrence occurred shortly after the surgery. We also suggest that the short follow-up did not allow us to assess late healing after 6 months. Finally, faecal incontinence was not assessed.
Radiofrequency thermocoagulation appears to be a promising minimally invasive surgical method, with a high-level of satisfaction at the end of the procedure. The fistula tract is coagulated and occluded by the probe, as shown by the absence of catheterization in nine of ten patients. This technique is easy to learn, simple to perform and rapid to carry out. It offers a comparable approach to the use of other strategies for tract coagulation, such as laser coagulation. However, disappointment within the first month of follow-up was associated with a very high recurrence rate in our study. These results are markedly poorer than those obtained with laser thermocoagulation. Coagulation methods offer symptomatic benefit in two-thirds of cases 5. Postoperative complications are ultimately quite rare, but there may be lasting pain, bleeding complications and oedematous reactions. There are scientific limitations to the previously performed studies, as they were uncontrolled, with a short follow-up and insufficient evaluation of failure. The definition of primary failure or success has often been imprecise, and relapse occurs early. Moreover, the long healing time after such an occlusion strategy is still a potential problem. Long-term evaluation is more appropriate for assessing these new methods 6. Long-term evaluations have shown that primary success varied between 55% and 65%, that several techniques were combined during the same procedure (closure of the internal orifice, lowering the flap, rerouting), and that they were repeated to obtain a more favourable healing rate 7. Another study also mentioned the need for prior drainage to obtain a better result with thermocoagulation methods 8. In our hands, radiofrequency thermocoagulation had a lower healing rate than that reported for loose setons. A retrospective Egyptian study examined factors associated with recurrence after the placement of a drain (removed secondarily after 3 months without further surgical procedures) for the treatment of high and/or complex anal fistulas 9. This study is informative because it provides an appreciation of the level of therapeutic response that would be spontaneously observed without surgery to achieve fistula tract closure. Surprisingly, recurrence was very low after simple removal of the drain: recurrent suppuration was observed in 10% of cases after a median follow-up of 16 months. In this retrospective cohort series, the therapeutic success rate was superior to that of the best methods of occlusion or coagulation of the tract. This puts into question the true minimally invasive effect of thermocoagulation. We observed at least one thermic ulceration after treatment of the fistula tract. It is conceivable that these new techniques are not as ‘minimally invasive’ as reported, leading to unclosed fibrotic tracts.
The failure rate for rectal flap advancement reported in our cohort is comparable to that of some studies in the literature 10. In a recent meta-analysis, the pooled failure rate for rectal flap advancement was 21%, with better results for full-thickness (7.4%) than partial-thickness flaps (19%) 11. In our study, the surgeons performed a partial-thickness flap and the failure rate was higher (34.1%) than that reported by the meta-analysis. However, the anal fistulas in our study were mainly complex and/or horseshoe fistulas. These factors have been reported to be predictive of failure 9.
Anal fistulas related to CD are classically the most challenging to treat because the tracts are complex and perianal lesions affect both the local and luminal prognosis. Paradoxically, our study suggests a better healing profile for patients with CD than for those without. Indeed, a previous study testing the long-term benefit of laser thermocoagulation also showed that it tended to be greater for patients with CD 7. Randomized control trials have been carried out on the combined use of biologicals and surgical closure, but success rates have been difficult to assess because it has been difficult to determine the contribution of each procedure 12, 13. In a recent study surgical closure of the tract was shown to improve healing rates better than treatment with biologicals or thiopurines 14. However, half of the patients with perianal fistulizing CD relapsed within 5 years of discontinuation of anti-TNFα 15. Thus, it is conceivable that anti-TNFα could also offer a benefit to patients with complex fistulas of cryptoglandular origin; the impact on the inflammatory process of the tract may enhance the benefit of sphincter-sparing surgery.
Conclusion
Coagulation of the fistula tract has the conceptual goal of fistula healing without dividing the anal sphincter. However, this minimally invasive technique requires careful prospective evaluation whereas optimistic assessments have been based on retrospective studies in which several combined and/or repeated techniques were used. Promising methods should associate the good healing rate reported in retrospective trials with a low frequency of side effects. Radiofrequency thermocoagulation does not fulfil these criteria and the technique needs improvement (lower intensity, larger diffusion). The place of biologicals in such treatment strategies is still under evaluation. Randomized controlled trials will be necessary to identify the most effective sphincter-sparing techniques.
Conflict of interest
None of authors have a conflict of interest.
Author contributions
Conception and design of the study: LS, CB, AMLH. Acquisition of the data: AMLH, GB. Analysis and interpretation of the data: CB, AMLH, LS. Drafting of the article: AMLH, LS, CB, GB. All authors reviewed the paper and approved the final submitted version.
Funding
There is no funding.