Chlamydia and HPV induce centrosome amplification in the host cell through additive mechanisms
Funding information: California Cancer Research Consortium, Grant/Award Number: 582146; National Institutes of Health, Grant/Award Numbers: R01 AI153410, R21 AI128723, T32 AI141346; National Science Foundation, Grant/Award Number: ID 2018262334
Abstract
Based on epidemiology studies, Chlamydia trachomatis has been proposed as a co-factor for human papillomavirus (HPV) in the development of cervical cancer. These two intracellular pathogens have been independently reported to induce the production of extra centrosomes, or centrosome amplification, which is a hallmark of cancer cells. We developed a cell culture model to systematically measure the individual and combined effects of Chlamydia and HPV on the centrosome in the same host cell. We found that C. trachomatis caused centrosome amplification in a greater proportion of cells than HPV and that the effects of the two pathogens on the centrosome were additive. Furthermore, centrosome amplification induced by Chlamydia, but not by HPV, strongly correlated with multinucleation and required progression through mitosis. Our results suggest that C. trachomatis and HPV induce centrosome amplification through different mechanisms, with the chlamydial effect being largely due to a failure in cytokinesis that also results in multinucleation. Our findings provide support for C. trachomatis as a co-factor for HPV in carcinogenesis and offer mechanistic insights into how two infectious agents may cooperate to promote cancer.
Take Aways
• Chlamydia and HPV induce centrosome amplification in an additive manner.
• Chlamydia-induced centrosome amplification is linked to host cell multinucleation.
• Chlamydia-induced centrosome amplification requires cell cycle progression.
• Chlamydia and HPV cause centrosome amplification through different mechanisms.
• This study supports Chlamydia as a co-factor for HPV in carcinogenesis.
1 INTRODUCTION
Each year, cervical cancer causes 300,000 deaths in the world, making it the fourth most common cancer in women (Arbyn et al., 2018). Human papillomavirus (HPV) is its main etiologic agent, with 90% of cervical carcinomas linked to “high-risk” HPV types, such as HPV16 and 18 (Muñoz et al., 2003). However, not all women infected with HPV develop cervical cancer, which suggests that additional factors are involved in carcinogenesis. A number of co-factors, including smoking, long-term use of oral contraceptives, and Chlamydia trachomatis infection, have been proposed (Fonseca-Moutinho, 2011; International Collaboration of Epidemiological Studies of Cervical Cancer et al., 2007; Silva, Cerqueira, & Medeiros, 2014). The evidence for C. trachomatis as co-factor is based on sero-epidemiology studies showing that women with cervical cancer were more likely to have had a prior Chlamydia infection (Smith et al., 2002; Zhu, Shen, Luo, Zhang, & Zhu, 2016).
HPV contributes to oncogenesis through multiple mechanisms. It causes aberrant proliferation of host cells, which supports viral DNA replication (Münger et al., 2004). It also promotes genomic instability in an infected host cell by inactivating cell cycle checkpoints, dysregulating host DNA repair pathways and inducing centrosome abnormalities (Banerjee, Wang, Broker, & Chow, 2011; Duensing et al., 2000; Spardy et al., 2009; Thomas & Laimins, 1998). As a consequence, HPV-infected cells accumulate cellular mutations while undergoing enhanced proliferation, which together lead to malignant transformation.
The centrosome, an organelle with a key role in microtubule organisation, is dysregulated in many cancer cells (Chan, 2011; Salisbury, Whitehead, Lingle, & Barrett, 1999). Normal diploid cells have a single centrosome, which duplicates in parallel to DNA in S-phase of the cell cycle. Cancer cells often contain extra, or supernumerary, centrosomes, which is a phenomenon called centrosome amplification (Lingle, Lutz, Ingle, Maihle, & Salisbury, 1998; Pihan et al., 1998). Such supernumerary centrosomes contribute to carcinogenesis by leading to chromosome mis-segregation, genomic instability and enhanced cell invasiveness (Ganem, Godinho, & Pellman, 2009; Godinho et al., 2014). Centrosome amplification is caused by at least three distinct mechanisms, which include cell–cell fusion, cytokinesis defects and dysregulation of the centrosome duplication machinery (Godinho & Pellman, 2014).
High-risk HPV induces centrosome amplification through its oncoproteins E6 and E7. Co-expression of E6 and E7 is sufficient to increase centrosome number in normal human keratinocytes, which leads to multipolar spindles and ultimately to genomic instability (Duensing et al., 2000). Additionally, mice expressing E6 and E7 have cervical and skin lesions containing cells with multiple centrosomes (Schaeffer et al., 2004). E7 expression has been proposed to promote centrosome amplification by altering the centrosome duplication machinery, whereas the mechanism for E6-induced centrosome amplification is less understood (Duensing et al., 2006; Duensing & Münger, 2002).
C. trachomatis also induces centrosome amplification (Grieshaber, Grieshaber, Miller, & Hackstadt, 2006; Johnson, Tan, & Sütterlin, 2009). Tissue culture cells infected with this obligate intracellular bacterium formed extra centrosomes in interphase and multipolar spindles in mitosis (Grieshaber et al., 2006). Intriguingly, these phenotypes persisted after the cells were cured of the infection. C. trachomatis has been proposed to induce centrosome abnormalities by dysregulating the centrosome duplication machinery and by causing cytokinesis defects in host cells (Alzhanov, Weeks, Burnett, & Rockey, 2009; Johnson et al., 2009). An important caveat is that prior mechanistic investigations were mostly done in C. trachomatis-infected HeLa cells, which contain HPV-18 DNA (Schwarz et al., 1985). Thus, these studies measured the combined effects of Chlamydia and HPV on the centrosome, but not the individual contribution of C. trachomatis.
In the present study, we investigated the respective roles of HPV and Chlamydia in causing centrosome abnormalities. To accomplish this goal, we developed a cell culture system that allowed us to determine the individual and combined effects of these two sexually transmitted pathogens on the centrosome in the same host cell. Our results provide biologic plausibility for the role of Chlamydia as a co-factor for HPV in the development of cervical cancer.
2 EXPERIMENTAL PROCEDURES
2.1 Antibodies used in this study
Primary antibodies: anti-centrin (Millipore, 04–1,624), anti-γ-tubulin (Abcam, ab11321), anti-α-tubulin (Sigma, T5168), anti-Cep164 (Santa Cruz, sc-240,226). Secondary antibodies for immunofluorescence microscopy: Donkey anti-Rabbit IgG Alexa Fluor 488 (Invitrogen, A21206), Donkey anti-Mouse IgG Alexa Fluor 555 (Invitrogen, A31570), Goat anti-Rat IgG Alexa Fluor 564 (Invitrogen, A11081), Donkey anti-Goat IgG Alexa Fluor 488 (Invitrogen, A21202).
2.2 Cell culture and Chlamydia infection
The parental hTERT-RPE-1 cell line was obtained from ATCC and cultured at 37°C and 5.0% CO2 in DMEM (Gibco, 11995–065) supplemented with 10% FBS (Atlanta Biologicals, S11550). A549 cells stably expressing HPV16 E6/E7 were a generous gift from Dr. Ashok Aiyar (LSU New Orleans) and were grown in DMEM supplemented with 10% FBS.
Chlamydia infection was done by infecting near-confluent cell monolayers with C. trachomatis serovar L2 (ATCC) at an MOI of 3 in SPG (200 mM sucrose, 20 mM sodium phosphate and 5 mM glutamate; pH 7.2) followed by centrifugation at 700 × g for 1 hr at room temperature. As control, cells were mock-infected with SPG alone. After centrifugation, the inoculum was removed and replaced with DMEM containing 10% FBS. The same infection conditions were used for RPE-1 and A549 cells.
2.3 Generation of RPE-1 cell lines expressing HPV16 E6/E7 oncoproteins
The pLXSN-HPV16 E6/E7 retroviral vector was obtained from Addgene (Plasmid #52394). From this vector, the pLXSN-Empty control vector was generated using Gibson assembly with forward primer 5′-TCCTCTAGAGTCCTGTAATCCTACCATGGCTGATCCTGCAG-3′ and reverse primer 5′-GATTACAGGACTCTAGAGGATC-3′. The pLXSN retroviral vectors and helper plasmid were co-transfected in 293 T cells with calcium phosphate (293 T cells and helper plasmid were generous gifts from Dr. Aimee Edinger, UC Irvine). Viral particles were collected 48 hr after transfection and used to infect RPE-1 cell monolayers with 10ug/mL polybrene (Sigma). Colonies were pooled after 10 days of selection with 600ug/mL G418 (Fisher, BP-918). HPV16 E6/E7 expressions were confirmed via RT-PCR. Forward primer 5′-GCAAGCAACAGTTACTGCG-3′ and reverse primer 5′- GGTTTCTCTACGTGTTCTTG-3′ were used to detect HPV16 E6 expression, and primer pair 5′-CAGCTCAGAGGAGGAGGATG-3′ and 5′-GCCCATTAACAGGTCTTCCA-3′ were used to detect HPV16 E7 expression.
2.4 Immunofluorescence microscopy
Cells, grown and infected on glass coverslips, were fixed in 100% ice-cold methanol for 10 min. Cells were permeabilized and incubated in a blocking buffer (2% FBS, 0.1% Triton) for 30 min at room temperature. C. trachomatis and host cell DNA were stained with NucBlue (Invitrogen, P36985). Centrosomes were detected with antibodies to centrin to observe centrioles, Cep164 to mark mother centrioles and γ-tubulin to observe pericentriolar material. Mitotic spindles and microtubule regrowth were visualised with anti-α-tubulin antibody. Coverslips were mounted with ProLong Glass Antifade containing NucBlue (Invitrogen, P36985). Immunofluorescence microscopy images were acquired on a Zeiss Axiovert 200 M microscope.
2.5 Microtubule regrowth assay
Cells grown on coverslips in growth medium supplemented with 25 mM HEPES were first incubated on ice for 40 min to depolymerize microtubules and then shifted to room temperature for 4 min to allow microtubule regrowth. Cells were rinsed for 40 s with microtubule buffer (60 mM PIPES, 25 mM HEPES, 10 mM EGTA, 2 mM MgCl2, 0.25 nM Nocodazole, 0.25 nM Paclitaxel, pH 6.9) and fixed with ice-cold methanol for 7 min prior to immunofluorescence microscopy analysis with antibodies to α-tubulin and γ-tubulin.
2.6 Pharmacological inhibition of cell cycle progression and centrosome duplication
Mock or Chlamydia-infected RPE-1 cells were arrested in S-phase by incubating them with 2 mM thymidine (ACROS Organics, 226,740,050) in standard growth medium for 24 hr, starting at 12 hpi. Cells were arrested in G2 by first incubating them with 2 mM thymidine for 18 hr, followed by release from the thymidine block for 6 hr and incubation with 10 μM RO-3306 (TOCRIS, cat # 4181) in standard medium for 12 hr. Both the S-phase and the G2 arrest experiments were analysed at 36 hpi using immunofluorescence microscopy.
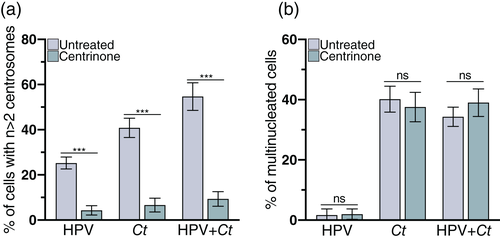
To inhibit centrosome duplication, Chlamydia, HPV and HPV + Chlamydia cells were incubated with 125 nM of the Plk4 inhibitor centrinone (MedChemExpress HY-18682) in standard growth medium starting at 1 hpi. The experiment was evaluated by immunofluorescence microscopy at 36 hpi.
2.7 EdU labeling
Cells undergoing S-phase were identified using the Click-iT EdU Cell Proliferation kit (Invitrogen, C10337). Control or HPV cells were grown on coverslips and infected with Chlamydia at an MOI of 3. At 36 hpi, cells were incubated with 10 μM EdU for 30 min and fixed with 4% PFA. EdU labelled cells were detected following the manufacturer's protocol.
2.8 Statistical analyses
For each experiment, three independent biological replicates were performed, and the results are presented as mean ± SD. Data were analysed by unpaired, two-tailed t-tests with Welch's correction on Graph Pad PRISM software version 8.
3 RESULTS
3.1 An experimental system for studying the effects of Chlamydia and HPV on the centrosome
We developed a cell culture model that allowed us to separate the effects of HPV and Chlamydia trachomatis (referred to as Chlamydia hereafter) on the centrosome in the same human cell (Figure 1a). We used retinal pigment epithelial cells (RPE-1) as the host cell because these diploid epithelial cells are neither cancerous nor transformed by HPV, unlike HeLa or A2EN cells that are commonly utilised for Chlamydia infection (Buckner et al., 2016). To mimic the effects of HPV on the centrosome, we generated an RPE-1 cell line that stably expresses the viral oncoproteins HPV16 E6 and E7 (referred to as “HPV cells”) (Figure S1). Prior studies showed that ectopic co-expression of the HPV oncoproteins E6 and E7 was sufficient to induce centrosome amplification (Duensing et al., 2000; Duensing & Münger, 2002). Ectopic E6/E7 expression is proposed to mimic the effect of HPV on the centrosome, with the advantage that this approach does not require a stratified epithelium typically used in an HPV infection model (Bienkowska-Haba et al., 2018). However, because we are not performing actual HPV infections, we cannot exclude the possibility that other HPV factors may contribute to the phenotypes measured in this study. RPE-1 cells transduced with an empty vector lacking these viral oncogenes served as a negative control (“control cells”).
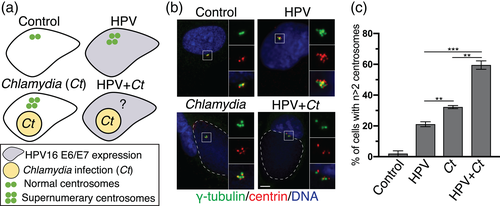
We infected either control cells with C. trachomatis to produce “Chlamydia cells”, or HPV cells to generate “HPV + Chlamydia cells”. For these infections, we used C. trachomatis serovar L2 because this strain has been used as an experimental model to study C. trachomatis-induced centrosome amplification (Grieshaber et al., 2006; Johnson et al., 2009). This strain is representative of other C. trachomatis strains, such as the genital serovars D and G, that produce comparable levels of centrosome amplification (Grieshaber et al., 2006).
We then compared the percentage of control, HPV, Chlamydia and HPV + Chlamydia cells with amplified centrosomes. We detected centrosomes by immunofluorescence microscopy with antibodies to the centrosomal marker proteins γ-tubulin and centrin2, which stain the pericentriolar material (PCM) and centrioles, respectively. Centrosome amplification was defined as cells harbouring more than two centrosomes (n > 2 γ-tubulin dots) (Figure 1b).
3.2 Chlamydia and HPV dysregulated centrosome number in an additive manner
This systematic approach revealed different effects of these two pathogens on the centrosome. Control cells had only few supernumerary centrosomes (Prevalence of 1.9%). Chlamydia cells showed a higher prevalence of amplified centrosomes than HPV cells (Prevalence of 32.2% vs. 21.1%) (Figure 1c), but the highest percentage of extra centrosomes (59.5%) was seen in HPV + Chlamydia cells. These data demonstrated that Chlamydia had a greater effect on the centrosome than HPV, and that together, they caused more centrosome amplification than either infectious agent alone (Figure 1c). Thus, HPV and Chlamydia cause centrosome amplification in a host cell through additive mechanisms.
We also examined the effects of HPV and Chlamydia on the centrosome of A549 cells, which are HPV-negative lung carcinoma cells. Similar to our results with RPE-1 cells, there was a greater prevalence of centrosome amplification in Chlamydia cells when compared with HPV cells. However, because E6/E7 expression did not cause a statistically significant increase in the percentage of A549 cells with amplified centrosomes, we were unable to test if the effects of HPV and Chlamydia on centrosome amplification are additive (Figure S2). We conclude from these experiments that, unlike for HPV, the prominent effects of Chlamydia in dysregulating centrosome number is independent of the cell type used as the host cell.
3.3 Chlamydia- and HPV-induced centrosome amplification did not disrupt the function of the centrosome in organising microtubules
We next tested if Chlamydia and HPV altered the function of the centrosome, which organises microtubules by controlling their nucleation and anchoring. HPV, Chlamydia and HPV + Chlamydia cells all formed a radial array of interphase microtubules, which was indistinguishable from that of control cells (Figure 2a). There was also no difference in the growth kinetics of microtubules as measured in regrowth assays (Figure 2b).
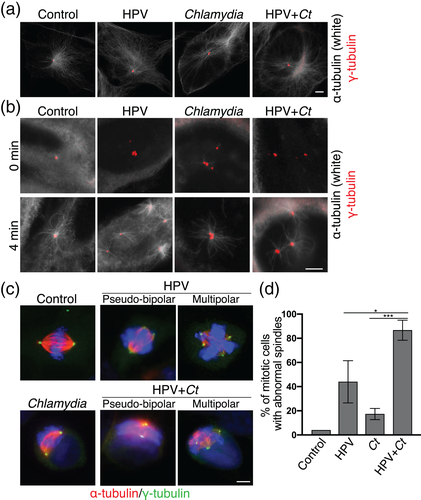
We further analysed spindle formation to assess centrosome function in mitosis (Figure 2c). HPV and HPV + Chlamydia cells showed a higher prevalence of abnormal spindles, including multipolar and pseudo-bipolar spindles, than control or Chlamydia cells (Figure 2c,d). This finding suggests that the abnormal interphase centrosomes in HPV and HPV + Chlamydia cells may promote the formation of abnormal mitotic spindles. In contrast, while a high percentage of Chlamydia cells had supernumerary centrosomes in interphase (Figure 1c), only few of these cells actually progressed into mitosis and formed abnormal spindles. We conclude that all cells with abnormal centrosomes were able to form mitotic spindles and that cell cycle progression to reach mitosis may be disrupted in Chlamydia cells with supernumerary centrosomes.
3.4 Chlamydia cells with amplified centrosomes are multinucleated and defective in cell cycle progression
We observed that Chlamydia was more likely to cause host cell multinucleation than HPV. Exactly 32.9% of Chlamydia cells and 32.1% of HPV + Chlamydia cells were multinucleated, compared with only 3.9% of HPV cells and 1.0% of control cells (Figure 3a). In Chlamydia cells, multinucleation and centrosome amplification were often present in the same cell. Consistent with this observation, we determined a ϕ coefficient of 0.94 between the two phenotypes, which indicates a strong correlation (Figure 3b). In contrast, HPV cells had a low ϕ coefficient of 0.23. HPV + Chlamydia cells displayed an intermediate correlation (ϕ coefficient = 0.49), consistent with a mixed effect (Figure 3b).
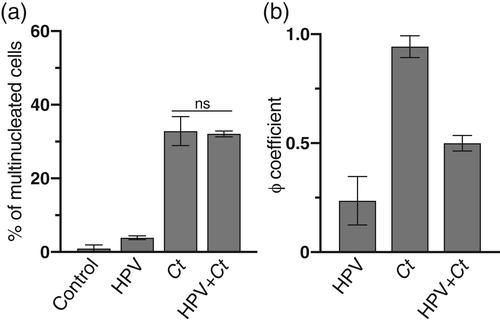
As multinucleation can cause cells to arrest in the G1 phase of the cell cycle (Ganem et al., 2009; Hart, Adams, & Draviam, 2021), we compared cell cycle progression in mono- and multinucleated Chlamydia and HPV + Chlamydia cells. Mononucleated Chlamydia and HPV + Chlamydia cells, as well as multi-nucleated HPV + Chlamydia, incorporated EdU, a marker for S-phase entry, to similar extents (Figure S3). In contrast, the percentage of EdU-positive multinucleated Chlamydia cells was reduced (Figure S3), suggesting that these cells become arrested in a pre-S-phase stage of the cell cycle, likely in G1.
3.5 Chlamydia-induced centrosome amplification and multinucleation result from a cytokinesis defect
The strong correlation between centrosome amplification and multinucleation in Chlamydia cells is indicative of a cytokinesis defect in the host cell, a reported consequence of Chlamydia infection (Alzhanov et al., 2009; Sun, Sin, Poirier, & Harrison, 2016). To test this hypothesis, we counted the number of Cep164-positive foci in HPV, Chlamydia and HPV + Chlamydia cells, focusing on cells with supernumerary centrosomes (Figure S4). In a normal mitotic cell, the two mature Cep164-positive centrioles are passed on to the two daughter cell after cytokinesis (Schmidt et al., 2012). The presence of two mature centrioles in the same cell is, therefore, a strong indicator of a cytokinesis defect. Greater than 60% of Chlamydia cells had two Cep164-positive foci, whereas HPV cells contained predominantly a single Cep164 focus. HPV + Chlamydia cells showed an intermediate phenotype (Figure S4).
As a complementary approach, we prevented Chlamydia, HPV and HPV + Chlamydia cells from reaching cytokinesis by blocking cell cycle progression either in S-phase or G2 and then measuring the prevalence of amplified centrosomes and multinucleation in each cell population. We induced a cell cycle arrest in S-phase by treating cells with thymidine. We also arrested cells in G2 by first synchronising cells in S-phase, with thymidine treatment and washout, and then incubating them with the G2 inhibitor RO-3306 (Ma & Poon, 2017). Each of these cell cycle manipulations decreased the prevalence of multinucleation as well as centrosome amplification in Chlamydia cells, but not in HPV cells (Figure 4a,b). Once again, HPV + Chlamydia cells showed an intermediate phenotype. Thus, multinucleation and centrosome amplification are closely linked in Chlamydia cells, with both phenotypes depending on progression through the cell cycle. Together, these results indicate that centrosome amplification in Chlamydia, but not in HPV cells, may be the consequence of a cytokinesis defect. They also provide further support that these pathogens contribute to centrosome abnormalities through different mechanisms in the same host cell.
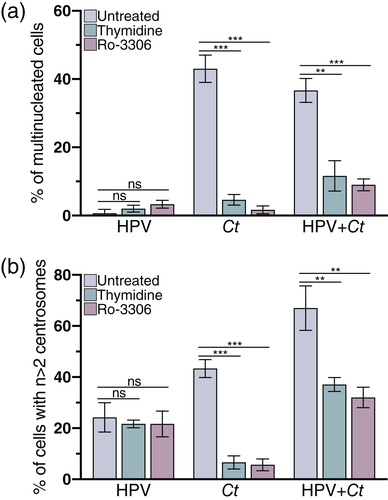
Our experimental set-up allowed us to examine an alternative model in which centrosome amplification in Chlamydia cells was proposed to cause multinucleation (Brown et al., 2014). To test this order of events, we prevented centrosome duplication through the use of the Plk4 inhibitor centrinone, which has been shown to block new centriole assembly in RPE-1 cells (Wong et al., 2015). Centrinone treatment significantly reduced centrosome amplification in HPV, Chlamydia and HPV + Chlamydia cells (Figure 5a), which is consistent with published results on Plk4 inhibition (Johnson et al., 2009; Korzeniewski, Treat, & Duensing, 2011). However, centrinone treatment did not prevent multinucleation in Chlamydia cells (Figure 5b), suggesting that centrosome amplification is not necessary for Chlamydia-induced multinucleation.
4 DISCUSSION
To investigate how C. trachomatis could contribute to HPV-mediated carcinogenesis, we measured the respective effects of these intracellular pathogens on the centrosome in the same host cell. We found that Chlamydia induced more cells to have amplified centrosomes than HPV and that these pathogens together caused an even higher percentage of cells with supernumerary centrosomes. These additive effects, together with our mechanistic analyses, suggest that Chlamydia and HPV induce centrosome amplification through different mechanisms. This study thus provides evidence that C. trachomatis, as a co-factor for HPV, may contribute to the development of cervical cancer by enhancing centrosome defects.
Chlamydia has been reported to cause centrosome amplification (Grieshaber et al., 2006; Johnson et al., 2009). These prior cell culture studies have predominantly used transformed cell lines that have an HPV background, such as HeLa cells (Grieshaber et al., 2006; Johnson et al., 2009; Knowlton, Fowler, Patel, Wallet, & Grieshaber, 2013). Although Chlamydia was found to also induce centrosome amplification in HPV-negative cell lines, such as NIH3T3 or HFF, these studies did not separate or compare the effects on the centrosome caused by either Chlamydia, HPV or both pathogens together (Grieshaber et al., 2006; Johnson et al., 2009; Knowlton et al., 2013). Furthermore, comparing centrosome amplification between different Chlamydia-infected HPV-negative and positive cell lines can be difficult. We avoided these issues by developing a cell culture model that uses the same cellular background to measure the respective effects of Chlamydia and HPV on the centrosome.
HPV has been shown to induce centrosome amplification through its oncoproteins E6 and E7. E7 is proposed to be the primary driver of centrosome amplification in an HPV infection. This conclusion is based on data showing that E7 dysregulates the centrosome duplication machinery in a Cdk2-dependent manner (Duensing et al., 2006) and that transient E7 expression is sufficient to cause centrosome amplification (Duensing, Duensing, Crum, & Münger, 2001; Duensing & Münger, 2002). In contrast, E6 has been proposed to play a lesser role in centrosome amplification by disabling the p53-dependent checkpoint (Duensing et al., 2001; Duensing & Münger, 2002). The loss of this checkpoint could lead to a cytokinesis defect (Bunz et al., 1998; Duensing et al., 2001), in which the nucleus and the two centrosomes duplicate normally, but the cell fails to divide, resulting in a multinucleated cell with extra centrosomes (Cosenza & Krämer, 2016).
This present study compared the mechanisms through which Chlamydia and HPV produce supernumerary centrosomes. We propose that Chlamydia-induced centrosome amplification is the result of a cytokinesis defect. This idea is supported by the observation that centrosome amplification in Chlamydia cells strongly correlated with host cell multinucleation and required progression through mitosis. Additionally, most Chlamydia cells with supernumerary centrosomes had two Cep164-positive foci. In contrast, centrosome amplification in HPV cells did not correlate with multinucleation and was independent of cell cycle progression. Furthermore, most HPV cells with amplified centrosomes only contained one mature Cep164-positive mother centriole.
Together, these data suggest that HPV and Chlamydia induce centrosome defects through different mechanisms in the same host cell. While HPV primarily dysregulates the centrosome duplication machinery through E7 (Duensing et al., 2001; Duensing & Münger, 2002), Chlamydia appears to cause centrosome dysregulation by disrupting cytokinesis. Consistent with this model, blocking cell cycle progression in HPV + Chlamydia cells partially reduced the prevalence of amplified centrosomes because it eliminated the contribution of Chlamydia, but not HPV, to this phenotype. Overall, our results suggest that these two pathogens activate two distinct pathways to induce centrosome dysregulation, although the respective contribution of each pathway to centrosome amplification appears to be cell type specific (Figure S2).
Chlamydia is proposed to block cytokinesis through multiple mechanisms, including the physical presence of the inclusion and expression of the chlamydial proteins, CT223 (IPAM) or the protease CPAF (Greene et al., 2003, Alzhanov et al., 2009, Sun et al., 2011, Brown et al., 2014). The latter two studies both described evidence for a link between multinucleation and centrosome amplification, but Brown and colleagues suggested that multinucleation is the consequence of CPAF-induced centrosome amplification in Chlamydia-infected cells (Brown et al., 2014). Our data, however, suggest that the cytokinesis defect is upstream of the other two phenotypes because centrinone treatment blocked centrosome amplification in Chlamydia cells but did not prevent multinucleation. Currently, it is not clear if centrosome amplification and multinucleation are functionally linked or if they are two independent consequences of the cytokinesis defect.
The presence of Chlamydia and HPV in the same cells produced a high prevalence of abnormal spindles but did not affect the function of the centrosome in organising microtubules in interphase or mitosis. As supernumerary centrosomes can lead to spindle defects, we propose that Chlamydia and HPV together produce abnormal spindles by altering centrosome number rather than function. These abnormal spindles may lead to chromosome mis-segregation and aneuploidy (Zhou et al., 1998), thereby providing a mechanism by which Chlamydia may contribute to HPV-induced carcinogenesis.
Our study provides evidence for Chlamydia-induced cell cycle dysregulation in the host cell. We observed that fewer multinucleated Chlamydia cells progressed through the cell cycle than either mononucleated Chlamydia or multinucleated HPV + Chlamydia cells (Figure S3). Thus, in addition to the known effect on cytokinesis, which leads to centrosome amplification and multinucleation, Chlamydia appears to disrupt progression through interphase. This Chlamydia-induced cell cycle arrest is likely in G1 and may be the consequence of either centrosome amplification or multinucleation. Centrosome amplification and multinucleation have been reported to lead to a G1 arrest through p53-dependent or p53-independent mechanisms, respectively (Hart et al., 2021; Mikule et al., 2007). However, as Chlamydia infection is known to induce p53 degradation, the presence of multiple nuclei in infected cells is more likely to induce this G1 arrest in a p53-independent manner (González et al., 2014:2; Hart et al., 2021; Siegl, Prusty, Karunakaran, Wischhusen, & Rudel, 2014). In HPV + Chlamydia cells, the presence of E6 and E7 may release the G1 arrest, possibly by degrading retinoblastoma protein (pRB) (Boyer, Wazer, & Band, 1996; Giacinti & Giordano, 2006), resulting in cell cycle progression and the formation of aberrant mitotic spindles.
We hypothesize that these combined effects on the centrosome occur through co-infection, with HPV infection preceding the Chlamydia infection. Both sexually transmitted agents are highly prevalent, making co-infection likely. These pathogens each infect the stratified epithelia of the cervix, but they do so at different locations, with HPV infecting basal cells (Spurgeon & Lambert, 2017), while Chlamydia infects the superficial cell layer (Murall et al., 2019). It is known, however, that HPV-infected basal cells divide, differentiate and migrate to the epithelial surface (Pinidis et al., 2016), thus providing a population of HPV-infected cells that can be infected acutely by Chlamydia. Our HPV/Chlamydia cell culture model mimics this sequence of events by taking cells expressing HPV E6 and E7 and then infecting them with C. trachomatis.
Our data are consistent with a “hit-and-run” model, in which C. trachomatis infects a cervical cell that has an on-going HPV infection and contributes to HPV-induced carcinogenesis by augmenting centrosomal defects in these cells. Chlamydia typically causes a lytic infection, but we propose that some co-infected cells survive the Chlamydia infection and have enhanced centrosomal defects that promote their progression into cancer cells. This model is supported by data showing that cervical cancer cells do not have evidence of active Chlamydia infection (Wallin et al., 2002). In addition, cervical cancer has been associated with serological evidence of past, rather than current, Chlamydia infection (Wallin et al., 2002). There is also evidence that cells can be cleared of a C. trachomatis infection with antibiotics while retaining amplified centrosome number (Grieshaber et al., 2006) or can survive through a non-lytic process called extrusion (Hybiske & Stephens, 2007).
Our findings provide biologic plausibility for C. trachomatis as a co-factor for HPV in carcinogenesis and have implications for the management of HPV and C. trachomatis infections. Based on this study, HPV-infected women who have had a prior C. trachomatis infection may be at a higher risk for the development of cervical cancer. Our findings suggest that current screening for cervical cancer, which is based on Pap smear identification of premalignant cells and HPV test, may not be adequate (Fontham et al., 2020). Enhanced screening for past C. trachomatis infection could be performed with an antibody blood test, but not with the standard C. trachomatis test, which is a nucleic acid amplification test (NAAT) that only detects an active or resolving infection (Meyer, 2016). If Chlamydia does contribute to cervical cancer, there will also be a greater need to identify and treat active infections and to develop a vaccine.
ACKNOWLEDGMENTS
We would like to thank Dr. Karl Munger for his input and guidance on generating our HPV16 E6 and E7-expressing RPE-1 cell line, and Dr. Aimee Edinger and Brendan Finicle for their assistance with lentiviral transductions. We also thank Dr. Ashok Aiyar for generously providing us with the A549 cell lines. This research was supported by the California Cancer Research Consortium (CCRC grant # 582146 to Christine Sütterlin) and the National Institutes of Health (R21 AI128723 and R01 AI153410 to Ming Tan and Christine Sütterlin). Kevin Wang was supported by a National Institutes of Health T32 training grant (AI141346). Karissa J. Muñoz was supported by a National Science Foundation graduate research fellowship (ID 2018262334).
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon request.




