Repositioning accuracy of implant prosthetic components used for digital and conventional workflow
16306 Poster Display Basic Research
Background
In the literature, misfit of the implant-supported restoration of 100 μm or less is often considered as clinically acceptable. The conventional and digital workflow inevitably involves reconnection of impression components and Ti bases to analogs and implants. Moreover, the position of the components could depend on the torque level. The positional inaccuracies of these components can influence the overall accuracy of the workflow and potentially lead to technical and biologic complications.
Aim/Hypothesis
The aim of this study was to evaluate repositioning errors of implant prosthetic components used in conventional and digital workflows. The null hypothesis was that there are no differences in repositioning accuracy of investigated components and position is not depending on the torque level.
Material and Methods
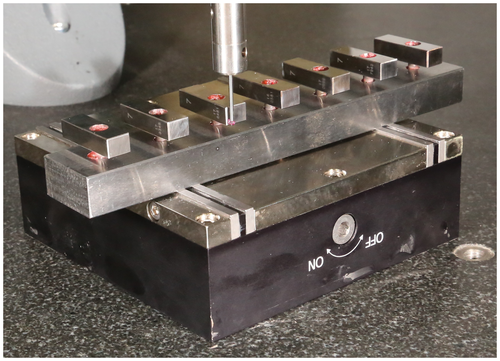
Seven implants (Microcone, Medentika) were fixed in milled steel blank using resin. Implant- and abutment-level impression copings, scan bodies, hex and non-hex Ti bases, and multi-unit caps (seven different components) were evaluated. A standardized test body was glued to each component at exactly the same position. The position of the component-test body complex (CTBC) was consecutively determined seven times after manual disassembly and reassembly using 15 Ncm torque for the impression components and multi-unit caps, while for the Ti bases 15 Ncm and 25 Ncm torque was applied. Predefined spots on the surface of the CTBC were sampled to detect any changes in position using a coordinate measuring machine (Fig. 1). Vertical, horizontal, sagittal and 3D discrepancies after each manual reassembly were monitored. A Mann-Whitney U test was used for pairwise comparison of the mean displacements of components to determine statistical differences (P = 0.05).
Results
Positional displacements were observed in all three axes. The mean (± standard deviation) 3D displacements of the implant-level pick-up copings (36 ± 8 μm) and scan bodies (26 ± 29 μm) were significantly greater than of the abutment-level impression copings (16 ± 8 μm) and scan bodies (12 ± 10 μm). The mean 3D displacement of the Ti base with hex (6 ± 5 μm) was significantly lower than that for the multi-unit cap (11 ± 8 μm). While non-hex Ti base (9 ± 7 μm) group have not significantly differed from the multi-unit cap group (11 ± 8 μm). There was a statistically significant difference in 3D deviations of hex (14 ± 21 μm) and the non-hex (15 ± 10 μm) Ti bases after increasing the torque from 15 Ncm to 25 Ncm.
Conclusion and Clinical Implications
Manual assembly and reassembly results in 3D positional changes of the impression copings, scan bodies and abutments. The components related to conventional and digital workflow could have deviations in the position up to 35 μm. The different torque levels could result in the positional change as well. The clinician should select the workflow with a component having better repositioning accuracy, which can potentially improve the clinical outcomes.