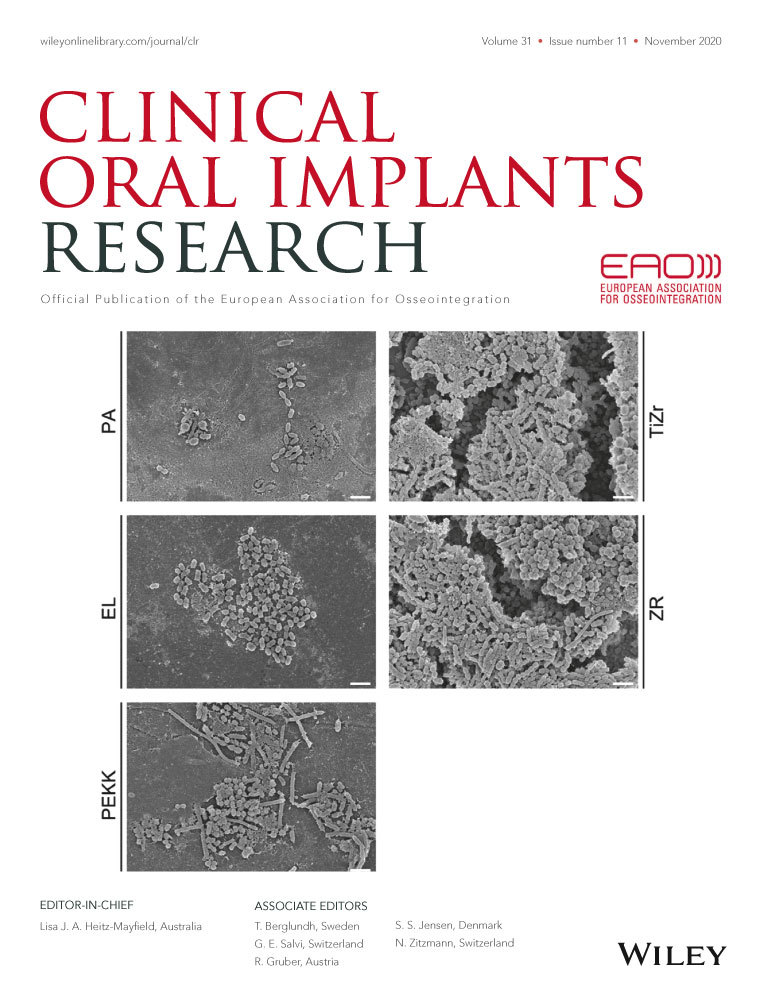
Biofilm formation on metal alloys, zirconia and polyetherketoneketone as implant materials in vivo
Barbara Zeller
Department of Reconstructive Dentistry, University Center for Dental Medicine, University of Basel, Basel, Switzerland
Contribution: Data curation (equal), Investigation (equal)
Search for more papers by this authorSimone Stöckli
Department of Oral Health and Medicine, University Center for Dental Medicine, University of Basel, Basel, Switzerland
Contribution: Data curation (equal), Investigation (equal)
Search for more papers by this authorLucia K. Zaugg
Department of Reconstructive Dentistry, University Center for Dental Medicine, University of Basel, Basel, Switzerland
Contribution: Methodology (equal), Writing - original draft (equal)
Search for more papers by this authorMonika Astasov-Frauenhoffer
Department Research, University Center for Dental Medicine, University of Basel, Basel, Switzerland
Contribution: Investigation (supporting), Methodology (supporting)
Search for more papers by this authorIrmgard Hauser-Gerspach
Department Research, University Center for Dental Medicine, University of Basel, Basel, Switzerland
Search for more papers by this authorTuomas Waltimo
Department of Oral Health and Medicine, University Center for Dental Medicine, University of Basel, Basel, Switzerland
Contribution: Conceptualization (equal), Project administration (equal), Supervision (lead)
Search for more papers by this authorCorresponding Author
Nicola U. Zitzmann
Department of Reconstructive Dentistry, University Center for Dental Medicine, University of Basel, Basel, Switzerland
Correspondence
Nicola U. Zitzmann, Department of Reconstructive Dentistry, University Center for Dental Medicine, University of Basel, Mattentrasse 40, CH-4058 Basel, Switzerland.
Email: [email protected]
Contribution: Conceptualization, Project administration, Resources (equal), Supervision (lead), Writing - review & editing (equal)
Search for more papers by this authorBarbara Zeller
Department of Reconstructive Dentistry, University Center for Dental Medicine, University of Basel, Basel, Switzerland
Contribution: Data curation (equal), Investigation (equal)
Search for more papers by this authorSimone Stöckli
Department of Oral Health and Medicine, University Center for Dental Medicine, University of Basel, Basel, Switzerland
Contribution: Data curation (equal), Investigation (equal)
Search for more papers by this authorLucia K. Zaugg
Department of Reconstructive Dentistry, University Center for Dental Medicine, University of Basel, Basel, Switzerland
Contribution: Methodology (equal), Writing - original draft (equal)
Search for more papers by this authorMonika Astasov-Frauenhoffer
Department Research, University Center for Dental Medicine, University of Basel, Basel, Switzerland
Contribution: Investigation (supporting), Methodology (supporting)
Search for more papers by this authorIrmgard Hauser-Gerspach
Department Research, University Center for Dental Medicine, University of Basel, Basel, Switzerland
Search for more papers by this authorTuomas Waltimo
Department of Oral Health and Medicine, University Center for Dental Medicine, University of Basel, Basel, Switzerland
Contribution: Conceptualization (equal), Project administration (equal), Supervision (lead)
Search for more papers by this authorCorresponding Author
Nicola U. Zitzmann
Department of Reconstructive Dentistry, University Center for Dental Medicine, University of Basel, Basel, Switzerland
Correspondence
Nicola U. Zitzmann, Department of Reconstructive Dentistry, University Center for Dental Medicine, University of Basel, Mattentrasse 40, CH-4058 Basel, Switzerland.
Email: [email protected]
Contribution: Conceptualization, Project administration, Resources (equal), Supervision (lead), Writing - review & editing (equal)
Search for more papers by this authorBarbara Zeller and Simone Stöckli should be considered joint first authorship.
Tuomas Waltimo and Nicola U. Zitzmann should be considered joint senior author.
[Correction added on 06 October 2020 after first online publication: The electron microscopy image for PEKK in Figure 4 has been corrected in this current version.]
Abstract
Objectives
This study investigated biofilm formation on discs of metal alloys, zirconia and polyetherketoneketone in vivo.
Material and Methods
Sixteen healthy volunteers conducted two runs of 24 hr each wearing an intraoral splint with 15 discs representing five different materials (gold-based [EL] and silver-based [PA] noble metal alloys; zirconia [ZR]; polyetherketoneketone [PEKK]; titanium zirconium alloy [TiZr]). Safranin staining assays and colony-forming unit (CFU) counts were conducted. Linear mixed-effects models were used to compare materials, and geometric mean ratios with 95% confidence interval were calculated with the level of significance set at α = 0.05.
Results
Less biofilm mass and lower CFU counts were found on PA and EL, while ZR and PEKK developed similar levels as the reference material TiZr alloy. Compared with PA, biofilm mass was 1.5 times higher for EL (p = .004), 1.7 times higher for PEKK (p < .001), 2.2 times higher for TiZr (p < .001) and 2.4 times higher for ZR (p < .001). The culturing method confirmed these results for EL and PA with lower CFU compared to TiZr. The biomass staining technique and cell culturing correlated for EL and PA.
Conclusion
Silver-based noble alloy and gold-based high noble alloy demonstrated the least biofilm formation indicating a potential clinical use as material for implant components in the transmucosal compartment. Zirconia and Polyetherketoneketone revealed similar results as the reference material titanium zirconium alloy used in commercially available titanium dental implant.
REFERENCES
- Aas, J. A., Paster, B. J., Stokes, L. N., Olsen, I., & Dewhirst, F. E. (2005). Defining the normal bacterial flora of the oral cavity. Journal of Clinical Microbiology, 43, 5721–5732. https://doi.org/10.1128/JCM.43.11.5721-5732.2005
- Abrahamsson, I., Berglundh, T., Glantz, P. O., & Lindhe, J. (1998). The mucosal attachment at different abutments. An experimental study in dogs. Journal of Clinical Periodontology, 25, 721–727. https://doi.org/10.1111/j.1600-051X.1998.tb02513.x
- Abrahamsson, I., & Cardaropoli, G. (2007). Peri-implant hard and soft tissue integration to dental implants made of titanium and gold. Clinical Oral Implants Research, 18, 269–274. https://doi.org/10.1111/j.1600-0501.2006.01326.x
- Ainamo, J., & Bay, I. (1975). Problems and proposals for recording gingivitis and plaque. International Dental Journal, 25, 229–235.
- Berglundh, T., Armitage, G., Araujo, M. G., Avila-Ortiz, G., Blanco, J., Camargo, P. M., … Zitzmann, N. (2018). Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. Journal of Periodontology, 89, 313–318. https://doi.org/10.1002/JPER.17-0739
- Bollen, C. M., Papaioanno, W., Van Eldere, J., Schepers, E., Quirynen, M., & van Steenberghe, D. (1996). The influence of abutment surface roughness on plaque accumulation and peri-implant mucositis. Clinical Oral Implants Research, 7, 201–211. https://doi.org/10.1034/j.1600-0501.1996.070302.x
- Chouirfa, H., Bouloussa, H., Migonney, V., & Falentin-Daudre, C. (2019). Review of titanium surface modification techniques and coatings for antibacterial applications. Acta Biomaterialia, 83, 37–54. https://doi.org/10.1016/j.actbio.2018.10.036
- Council on Dental Materials, Instruments, and Equipment (1984). Classification system for cast alloys. Journal of the American Dental Association, 109, 766.
- de Avila, E. D., Avila-Campos, M. J., Vergani, C. E., Spolidorio, D. M., & Mollo Fde, A. (2016). Structural and quantitative analysis of a mature anaerobic biofilm on different implant abutment surfaces. Journal of Prosthetic Dentistry, 115, 428–436. https://doi.org/10.1016/j.prosdent.2015.09.016
- El Awadly, T. A., Wu, G., Ayad, M., Radi, I. A. W., Wismeijer, D., Abo El Fetouh, H., & Osman, R. B. (2020). A histomorphometric study on treated and untreated ceramic filled peek implants versus titanium implants: Preclinical in vivo study. Clinical Oral Implants Research, 31, 246–254. https://doi.org/10.1111/clr.13562
- Feng, Q. L., Wu, J., Chen, G. Q., Cui, F. Z., Kim, T. N., & Kim, J. O. (2000). A mechanistic study of the antibacterial effect of silver ions on Escherichia coli and Staphylococcus aureus. Journal of Biomedical Materials Research, 52, 662–668. https://doi.org/10.1002/1097-4636(20001215)52:4<662:AID-JBM10>3.0.CO;2-3
- Ferraris, S., & Spriano, S. (2016). Antibacterial titanium surfaces for medical implants. Materials Science and Engineering: C, 61, 965–978. https://doi.org/10.1016/j.msec.2015.12.062
- Flores, C. Y., Diaz, C., Rubert, A., Benitez, G. A., Moreno, M. S., Lorenzo, F., … Vericat, C. (2010). Spontaneous adsorption of silver nanoparticles on Ti/TiO2 surfaces. Antibacterial effect on Pseudomonas aeruginosa. Journal of Colloid and Interface Science, 350, 402–408. https://doi.org/10.1016/j.jcis.2010.06.052
- Grosgogeat, B., Reclaru, L., Lissac, M., & Dalard, F. (1999). Measurement and evaluation of galvanic corrosion between titanium/Ti6a14v implants and dental alloys by electrochemical techniques and auger spectrometry. Biomaterials, 20, 933–941.
- Guan, M., Chen, Y., Wei, Y., Song, H., Gao, C., Cheng, H., … Xiong, W. (2019). Long-lasting bactericidal activity through selective physical puncture and controlled ions release of polydopamine and silver nanoparticles-loaded TiO2 nanorods in vitro and in vivo. International Journal of Nanomedicine, 14, 2903–2914.
- Hahnel, S., Wieser, A., Lang, R., & Rosentritt, M. (2015). Biofilm formation on the surface of modern implant abutment materials. Clinical Oral Implants Research, 26, 1297–1301. https://doi.org/10.1111/clr.12454
- Hanawa, T. (2020). Zirconia versus titanium in dentistry: A review. Dental Materials Journal, 39, 24–36.
- John, G., Becker, J., & Schwarz, F. (2017). Effects of different titanium zirconium implant surfaces on initial supragingival plaque formation. Clinical Oral Implants Research, 28, e84–e90. https://doi.org/10.1111/clr.12878
- Kim, J. S., Kuk, E., Yu, K. N., Kim, J. H., Park, S. J., Lee, H. J., … Cho, M. H. (2007). Antimicrobial effects of silver nanoparticles. Nanomedicine, 3, 95–101. https://doi.org/10.1016/j.nano.2006.12.001
- Knaus, J., Schaffarczyk, D., & Colfen, H. (2020). On the future design of bio-inspired polyetheretherketone dental implants. Macromolecular Bioscience, 20, e1900239.
- Koutouzis, T., Richardson, J., & Lundgren, T. (2011). Comparative soft and hard tissue responses to titanium and polymer healing abutments. Journal of Oral Implantology, 37, 174–182. https://doi.org/10.1563/AAID-JOI-D-09-00102.1
- Lassila, L., Säilynoja, E., Prinssi, R., Vallittu, P. K., & Garoushi, S. (2020). The effect of polishing protocol on surface gloss of different restorative resin composites. Biomaterial Investigations in Dentistry, 7, 1–8. https://doi.org/10.1080/26415275.2019.1708201
- Lopez-Piriz, R., Sola-Linares, E., Granizo, J. J., Diaz-Guemes, I., Enciso, S., Bartolome, J. F., … Moya, J. S. (2012). Radiologic evaluation of bone loss at implants with biocide coated titanium abutments: A study in the dog. PLoS One, 7, e52861. https://doi.org/10.1371/journal.pone.0052861
- Martinez, A., Guitian, F., Lopez-Piriz, R., Bartolome, J. F., Cabal, B., Esteban-Tejeda, L., … Moya, J. S. (2014). Bone loss at implant with titanium abutments coated by soda lime glass containing silver nanoparticles: A histological study in the dog. PLoS One, 9, e86926. https://doi.org/10.1371/journal.pone.0086926
- Meier, R., Hauser-Gerspach, I., Lüthy, H., & Meyer, J. (2008). Adhesion of oral streptococci to all-ceramics dental restorative materials in vitro. Journal of Materials Science. Materials in Medicine, 19, 3249–3253.
- Mishra, S., & Chowdhary, R. (2019). Peek materials as an alternative to titanium in dental implants: A systematic review. Clinical Implant Dentistry and Related Research, 21, 208–222. https://doi.org/10.1111/cid.12706
- Nascimento, C., Pita, M. S., Santos Ede, S., Monesi, N., Pedrazzi, V., Albuquerque Junior, R. F., & Ribeiro, R. F. (2016). Microbiome of titanium and zirconia dental implants abutments. Dental Materials, 32, 93–101. https://doi.org/10.1016/j.dental.2015.10.014
- Nevins, M., Nevins, M. L., Camelo, M., Boyesen, J. L., & Kim, D. M. (2008). Human histologic evidence of a connective tissue attachment to a dental implant. International Journal of Periodontics and Restorative Dentistry, 28, 111–121.
- O'Leary, T. J., Drake, R. B., & Naylor, J. E. (1972). The plaque control record. Journal of Periodontology, 43, 38. https://doi.org/10.1902/jop.1972.43.1.38
- Qin, S., Xu, K., Nie, B., Ji, F., & Zhang, H. (2018). Approaches based on passive and active antibacterial coating on titanium to achieve antibacterial activity. Journal of Biomedical Materials Research Part A, 106, 2531–2539. https://doi.org/10.1002/jbm.a.36413
- Rimondini, L., Cerroni, L., Carrassi, A., & Torricelli, P. (2002). Bacterial colonization of zirconia ceramic surfaces: An in vitro and in vivo study. International Journal of Oral and Maxillofacial Implants, 17, 793–798.
- Roehling, S., Astasov-Frauenhoffer, M., Hauser-Gerspach, I., Braissant, O., Woelfler, H., Waltimo, T., … Gahlert, M. (2017). In vitro biofilm formation on titanium and zirconia implant surfaces. Journal of Periodontology, 88, 298–307. https://doi.org/10.1902/jop.2016.160245
- Schwarz, F., Sculean, A., Romanos, G., Herten, M., Horn, N., Scherbaum, W., & Becker, J. (2005). Influence of different treatment approaches on the removal of early plaque biofilms and the viability of SAOS2 osteoblasts grown on titanium implants. Clinical Oral Investigations, 9, 111–117. https://doi.org/10.1007/s00784-005-0305-8
- Teughels, W., Van Assche, N., Sliepen, I., & Quirynen, M. (2006). Effect of material characteristics and/or surface topography on biofilm development. Clinical Oral Implants Research, 17, 68–81. https://doi.org/10.1111/j.1600-0501.2006.01353.x
- Venugopalan, R., & Lucas, L. C. (1998). Evaluation of restorative and implant alloys galvanically coupled to titanium. Dental Materials, 14, 165–172. https://doi.org/10.1016/S0109-5641(98)00024-4
- Wang, M., Bhardwaj, G., & Webster, T. J. (2017). Antibacterial properties of pekk for orthopedic applications. International Journal of Nanomedicine, 12, 6471–6476.
- Wataha, J. C. (2000). Biocompatibility of dental casting alloys: A review. Journal of Prosthetic Dentistry, 83, 223–234. https://doi.org/10.1016/S0022-3913(00)80016-5
- Yamane, K., Ayukawa, Y., Takeshita, T., Furuhashi, A., Yamashita, Y., & Koyano, K. (2013). Bacterial adhesion affinities of various implant abutment materials. Clinical Oral Implants Research, 24, 1310–1315. https://doi.org/10.1111/j.1600-0501.2012.02574.x
- Yuan, B., Cheng, Q., Zhao, R., Zhu, X., Yang, X., Yang, X., … Zhang, X. (2018). Comparison of osteointegration property between pekk and peek: Effects of surface structure and chemistry. Biomaterials, 170, 116–126. https://doi.org/10.1016/j.biomaterials.2018.04.014
- Zaugg, L. K., Astasov-Frauenhoffer, M., Braissant, O., Hauser-Gerspach, I., Waltimo, T., & Zitzmann, N. U. (2017). Determinants of biofilm formation and cleanability of titanium surfaces. Clinical Oral Implants Research, 28, 469–475. https://doi.org/10.1111/clr.12821
- Zee, K. Y., Samaranayake, L. P., & Attström, R. (1997). Scanning electron microscopy of microbial colonization of ‘rapid’ and ‘slow’ dental-plaque formers in vivo. Archives of Oral Biology, 42, 735–742. https://doi.org/10.1016/S0003-9969(97)00059-9
- Zitzmann, N. U., & Berglundh, T. (2008). Definition and prevalence of peri-implant diseases. Journal of Clinical Periodontology, 35, 286–291. https://doi.org/10.1111/j.1600-051X.2008.01274.x