Alveolar ridge preservation and its impact on marginal bone level changes around dental implants: A retrospective, cohort comparative study
Chiara Cinquini and Rossana Izzetti contributed equally to this study.
Abstract
Objectives
This retrospective study compared the outcomes of implants placed in alveolar ridge preservation (ARP) treated sites with those in spontaneously healed (SH) sites.
Materials and Methods
The study included patients presenting with one implant placed in an ARP-treated socket and one in an SH site. The primary outcome was the comparison of Marginal Bone Level Changes (MBLC). Statistical analysis was performed to identify factors influencing MBLC, including age, gender, smoking, parafunctional habits, and prosthetic emergence angle.
Results
Of these, 28 patients (23 females, 82.1%) were included in this analysis. Sockets in the SH group were classified as type I, whereas type II sockets were more common in the ARP group. The SH group exhibited significantly higher MBLC than the ARP group (p = 0.032), with values, respectively, of 1.00 [0.25; 1.62] and 0.40 [0.00; 1.00] mm. Among all evaluated parameters, the performance of ARP was the only factor significantly affecting MBLC (β = −0.72, SE: 0.32, p = 0.026). Age, gender, smoking, parafunctional habits, and prosthetic emergence angle did not significantly affect MBLC.
Conclusions
The study shows the potential role of ARP in maintaining stable marginal bone levels around implants. In our sample, ARP significantly reduced MBLC compared with spontaneous healing, highlighting its possible impact in clinical practice for better peri-implant bone stability.
Summary box
What is known
Alveolar ridge preservation (ARP) aims to reduce post-extractive bone volume shrinkage to facilitate implant placement and, subsequently, implant-prosthetic rehabilitation. Among the factors potentially affecting peri-implant tissue stability, the emergence profile of prosthetic restoration has been reported with conflicting results in the literature.
What this study adds
According to our results, ARP was superior to spontaneous healing in preserving peri-implant tissues and preventing marginal bone loss. The prosthetic emergence profile does not significantly affect marginal bone level changes over time.
1 INTRODUCTION
The morphology of the alveolar ridge following tooth extraction is an extremely relevant critical factor for implant placement. Bone remodeling is well known to reduce the alveolar ridge's volume overall. This process can be further influenced by the thickness of the buccal bone, the integrity or defect of the buccal bone wall, and the condition of the soft tissues.1
The characteristics of extraction sockets have been extensively investigated in the scientific literature. Previous attempts have been made to classify the alveolar socket based on bone height and width, as well as soft tissue quality, quantity, and phenotype. Thus, fresh extraction sockets can be categorized as adequate, compromised, or deficient.2
According to Juodzbalys and colleagues,2 an alveolar socket is considered adequate (type I) if it has a bone height greater than 10 mm, a buccal bone thickness greater than 2 mm without periodontal or traumatic socket bone lesions, and gingival tissue that is pink, firm, and at least 2 mm thick. Compromised (type II) and deficient (type III) sockets are characterized by reduced height, decreased buccal bone thickness, and inflamed and thin gingival tissue with deficiencies or variations. An ideal buccal bone thickness of at least 2 mm is recommended to reduce the risk of mid-facial mucosal recession and further loss of the buccal bone wall.3, 4
Site morphology can be improved in compromised or deficient extraction sockets by grafting the residual sockets, a procedure known as alveolar ridge preservation (ARP). This procedure involves the application of grafting materials of various origins, such as human, animal, or synthetic (allograft, xenograft, or alloplastic), which may be combined with barrier membranes.5 ARP aims to preserve the alveolar ridge volume and prevent the need for additional procedures at the time of implant placement. However, the grafting material is partially replaced by newly formed bone, leading to slightly reduced mineralization of the grafted socket compared with spontaneously healed alveolar sockets.6, 7
The success of the ARP procedure is closely related to the type of extraction socket being grafted. A previous study has indicated a lower occurrence of biological complications such as peri-implantitis in type I and II grafted sockets compared with type III.8 Nonetheless, the survival rate and marginal bone level changes of implants placed in grafted sites are similar to those of implants placed in pristine bone, and the overall clinical performance is comparable.9, 10
Various factors can potentially affect tissue stability around implant-supported rehabilitations, including smoking and parafunctional habits.11, 12 It has been suggested that the emergence profile of the prosthetic restoration may influence marginal bone loss13, 14 and the risk of developing peri-implantitis,15 although the literature reports conflicting results.
The present study assessed implant success in grafted versus non-grafted alveolar sockets within a cohort of patients selected from a previously described study population.8
The primary aim of this study was to compare marginal bone level changes around implants inserted in sites treated with ARP versus implants inserted in pristine bone.
Secondary outcomes were the rate of complications, the need for additional bone grafting procedures at the time of implant placement and the evaluation of variables that could affect clinical outcomes such as the prosthetic restoration's emergence profile, parafunctional habits and smoking habits.
2 MATERIALS AND METHODS
2.1 Study protocol and approval
A retrospective, cohort comparative study was conducted on patients previously treated at the University Hospital of Pisa by the same expert oral surgeon (AB) with more than 30 years of experience. To be eligible, patients should have had one implant placed in an ARP-treated site and an implant placed in a spontaneously healed (SH) site, matching for positioning in the dental arch. Dental records were examined, and eligible patients were recalled for follow-up between January 2021 and April 2022. All patients received detailed information regarding the study protocol and were asked to sign a written consent form to participate in the study.
To be included, patients had to fulfill the following eligibility criteria:
- Patients ≥18 years.
- Ability to understand and sign a written consent form.
- Compliance with study follow-up.
- Patients treated with medications affecting bone metabolism.
- Patients during pregnancy or breastfeeding.
- Patients with uncontrolled medical conditions.
- Patients with incomplete medical records.
- Patients not capable of giving their consent to participate in the study.
The study was conducted following the Good Clinical Practice Guidelines (GCPs) and according to the statements of the Declaration of Helsinki as amended in 2013,11 and was reported according to the STROBE (Strengthening the reporting of observational studies in epidemiology) guidelines.12
The Institutional Review Board approved conducting this retrospective analysis (North-West Tuscany Ethics Committee, approval number: 57489/2019).
2.2 Surgical procedures
Tooth extractions were performed with a minimally traumatic surgical technique with the use of thin elevators and forceps to preserve the buccal bone plate. In multi-rooted teeth, root separation was performed with high-speed handpieces and surgical burs, and the roots were extracted separately. The alveolar sockets were left to either spontaneous healing (SH) or grafted according to ARP procedures.
ARP involved alveolar sockets filling with collagenated cortico-cancellous porcine bone (Osteobiol®, MP3®, Tecnoss Dental, Giaveno (TO), Italy) up to the bony walls. A collagen membrane of porcine origin (Osteobiol®, Evolution®, Tecnoss Dental, Giaveno (TO), Italy) was placed to avoid biomaterial displacement and stabilized with sutures (Figure 1).
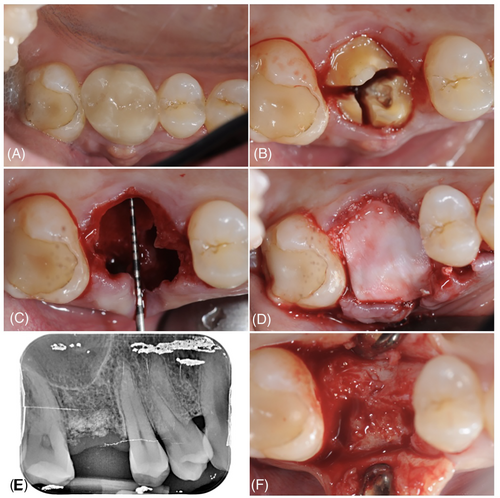
Implants were inserted in the grafted sockets 4/5 months after grafting.
2.3 Retrospective data collection
Two investigators (CC and RI) screened the medical records of patients treated with at least two dental implants (one in an ARP-treated site and one placed in spontaneously healed ridge), and eligible patients fulfilling the inclusion/exclusion criteria were included.
Demographic data, including age, gender, presence of systemic diseases and continuative pharmacological therapy, were collected from the patient's medical records.
Smoking habits were registered dichotomously as absent/present. The presence of tooth wear (including restorations) exposed dentinal tissue, hypertrophic masticatory muscles, and tooth fractures were considered signs of the presence of parafunctional habits.13 Finally, the number of oral hygiene recalls per year was registered.
Tooth extraction characteristics and performance of ARP procedure (simple/complex extraction, type of extraction socket according to Juodzbalys and colleagues)2 were retrieved from patients' medical records. Tooth position (incisor, canine, premolar or molar), the reason for extraction (decay, fracture, or endodontic/periodontal/orthodontic/prosthetic reasons) and biomaterials used for ARP were also recorded.
Data on the implant-prosthetic rehabilitations included timing of implant placement, implant characteristics (bone or tissue-level, length and diameter, surface, abutment connection), surgical intervention features (insertion torque values, implant stability, need for additional bone regeneration procedures at the time of implant placement, complications), prosthetic restoration type (cemented or screw-retained), and time of function at follow-up.
2.4 Follow-up recall
The follow-up evaluation included clinical and radiographic assessment and was carried out by a single calibrated examiner (intra-examiner reliability >0.8) not involved in patients' treatment.
The survival and success rates of implant-prosthetic rehabilitations14 were assessed as complications, soft tissue recession or metal exposure, implant health status (healthy or presence of mucositis or periimplantitis), periodontal parameters, and radiographic marginal bone level (MBL).
Periodontal parameters were registered with a standardized periodontal probe (UNC). Periodontal probing was performed with gentle pressure until resistance reached the pocket's end.15 Probing depth (PD) and bleeding on probing (BoP) were evaluated at six sites per implant. The presence of peri-implant suppuration and clinical signs of inflammation were evaluated as dichotomic parameters (presence/absence). Periodontal Screening Recording (PSR) was performed with the PSR probe on natural teeth as described by Jeffcoat and colleagues,16 with values ranging from 0 (PD <3.5 mm and absence of BOP) to 4 (PD >5.5 mm).
Follow-up periapical radiographs were performed with the parallel cone technique, a Rinn sensor holder and a phosphor image sensor (VistaScan system, Dürr Dental, Bietigheim-Bissingen, Germany).
MBL was measured at distal and mesial sites with the digital software DBSwin (Air Techniques Inc, Melville (NY)) as the distance between the fixture-abutment interface and the implant's most apical point. Radiographic Marginal Bone Level Change (MBLC) was measured by comparing baseline intraoral radiographs taken following prosthetic loading with follow-up radiographs.
The emergence angle was calculated on mesial and distal aspects of the implant-prosthetic restoration according to the method described by Katafuchi and colleagues17 as the angle between the long axis of the implant and a line tangent to the prosthetic restoration.
Survival and success rates were evaluated according to the criteria proposed by Albrektsson and colleagues14 Implant health status was evaluated according to the criteria proposed in 2017 by Berglundh and colleagues18 as absence of erythema, BoP, swelling and suppuration. In the presence of BoP and/or clinical signs of inflammation, the site was considered affected by peri-implant mucositis. Peri-implantitis was diagnosed in cases of radiographic bone loss associated with inflammation or infection.
2.5 Statistical analysis
The performance of both procedures (SH and ARP) for each patient created nested paired data due to the within-subject correlation. The power calculation was based on a two-sided paired t-test, which tested the null hypothesis that there would be no difference (on average) in within-subject mean marginal bone level changes (from T0 to T3) between the two procedures (SH vs. ARP). Twenty-eight patients were required to detect an effect size of 0.85 with 80% power at a 5% significance level, where the effect size was defined as the expected mean difference between the two procedures of average within-subject changes of mean marginal bone level divided by the standard deviation of itself. The analysis was conducted on two levels: patients and implants. Descriptive statistics were produced following the variable's distribution. Continuous variables were summarized by median [first; third] quartiles and categorical by absolute frequencies and percentages (%). The differences in mean MBL at implant placement, restoration, and follow-up were assessed using the Wilcoxon rank sum test for the primary outcome variable. The Wilcoxon rank sum and McNemar tests assess differences in ridge preservation procedure versus ridge preservation in implant level characteristics. The linear mixed model evaluated the relationship between ridge preservation and the change in marginal bone level over time, controlling for patient characteristics. The p-values were calculated using Satterthwai. The model's performance was assessed using the Akaike Information Criterion (AIC), the Bayesian Information Criterion (BIC) and the Pseudo-R2. All statistical tests were two-sided, with a significance level set at p ≤ 0.05. Analyses were performed using the R software environment for statistical computing and graphics (version 4.2; http://www.r-project.org/).
3 RESULTS
Forty patients were initially screened to be included in this study; of these, 28 patients (23 females, 82.1%) had one implant placed in an ARP-treated site and an implant placed in a spontaneously healed (SH) site and were thus included in this analysis.
Mean follow-up at the time of recall was 100 [87.5; 134] months for the ARP group and 84.5 [45.2; 114] months for the SH group, with no statistically significant differences (p = 0.074).
Medical history revealed the presence of systemic diseases and pharmacological treatment in 50% of patients. 17.9% of the patients were smokers (Table 1) and 15 patients had parafunctional habits (53.6%). Most patients (71.4%) attended to two or more oral hygiene recalls per year.
| Patients' characteristics | N = 28 |
|---|---|
| Age, years | 56.0 [54.0; 61.0] |
| Gender | |
| F | 23 (82.1%) |
| M | 5 (17.9%) |
| Smoking habit | |
| No | 23 (82.1%) |
| Yes | 5 (17.9%) |
| Parafunctional habits | |
| No | 13 (46.4%) |
| Yes | 15 (53.6%) |
| Metabolic-endocrine diseases (osteoporosis, diabetes) | |
| No | 14 (63.6%) |
| Yes | 8 (36.4%) |
| Psychiatric (anxiety disorder) | |
| No | 14 (87.5%) |
| Yes | 2 (12.5%) |
| Neoplastic | |
| No | 14 (93.3%) |
| Yes | 1 (6.67%) |
| Other (hypercholesterolemia, gastroesophageal reflux, gastritis, psoriasis, dematomyositis) | |
| No | 14 (66.7%) |
| Yes | 7 (33.3%) |
A total of 56 extractions were performed. Molars and premolars accounted for the majority of elements extracted. The presence of carious lesions was the most common reason for tooth extraction. Overall, no differences between the SH and ARP groups were noted regarding the type of tooth extracted, reason for extraction or surgical complexity.
Regarding extraction socket classification, a statistically significant difference was observed between the ARP and SH groups (p = 0.040). Most cases in the SH group belonged to type I, whereas in the ARP group, type II was more common. Type III alveolar sockets were encountered in two cases, one per each group (Table 2).
| Tooth extractions characteristics | SH (n = 28) | ARP (n = 28) | p-Value |
|---|---|---|---|
| Tooth type | |||
| CI (cuspid, incisor) | 1 (3.57%) | 3 (10.7%) | 0.611 |
| MP (molar, premolar) | 27 (96.4%) | 25 (89.3%) | |
| Reason for tooth extraction | |||
| Caries | 17 (54.9%) | 14 (45.1%) | 0.624 |
| Endodontic lesion | 4 (14.3%) | 6 (21.4%) | |
| Fracture | 7 (25.0%) | 8 (28.6%) | |
| Tooth extraction | |||
| Complex | 6 (21.4%) | 5 (17.9%) | 1.000 |
| Simple | 22 (78.6%) | 23 (82.1%) | |
| Type of extraction socket | |||
| I | 16 (57.1%) | 7 (25.0%) | 0.040 |
| II | 11 (39.3%) | 20 (71.4%) | |
| III | 1 (3.57%) | 1 (3.57%) | |
- Note: p-Value derived from the McNemar test. Bold values: statistically significant differences between groups.
- Abbreviations: ARP, alveolar ridge preservation; SH, spontaneously healed.
In the ARP group, collagenated cortico-cancellous porcine bone was used as grafting material, with a mean quantity of 0.73 cc (SD = 0.25 cc) per site.
In sites treated with ARP, implant placement was performed 5.00 [4.50; 6.00] months after tooth extraction; in SH sites, implants were placed after a mean of 26.00 [9.00; 54.00] months.
Regarding baseline characteristics of implant placement (Table 3), no differences were noted among study groups except for the insertion torque parameter, which registered significantly higher values in the SH group compared with the ARP group (p = 0.020).
| Implant level characteristics at baseline | SH (n = 28) | ARP (n = 28) | p-Value |
|---|---|---|---|
| Months from prosthetic restoration to the last follow-up | 84.5 [45.2; 114] | 100 [87.5; 134] | 0.074 |
| Implant placement (maxilla, mandible) | |||
| Maxilla | 14 (50.0%) | 19 (67.9%) | 0.277 |
| Mandible | 14 (50.0%) | 9 (32.1%) | |
| Implant placement (anterior, posterior) | |||
| Anterior | 2 (7.14%) | 3 (10.7%) | 1.000 |
| Posterior | 26 (92.9%) | 25 (89.3%) | |
| Implant type (bone level, tissue level) | |||
| Bone level | 22 (78.6%) | 27 (96.4%) | 0.101 |
| Tissue level | 6 (21.4%) | 1 (3.57%) | |
| Insertion torque | |||
| >35 | 24 (85.7%) | 15 (53.6%) | 0.020 |
| ≤35 | 4 (14.3%) | 13 (46.4%) | |
| Primary stability | |||
| Spinning | 1 (3.57%) | 0 (0.00%) | 1.000 |
| Stable | 27 (96.4%) | 28 (100%) | |
| Additional bone augmentation required (no, yes) | |||
| No | 22 (78.6%) | 23 (82.1%) | 1.000 |
| Yes | 6 (21.4%) | 5 (17.9%) | |
| Complications during or after surgery: No | 28 (100%) | 28 (100%) | |
| Soft tissue augmentation required | |||
| No | 27 (96.4%) | 24 (85.7%) | 0.352 |
| Yes | 1 (3.57%) | 4 (14.3%) | |
| Type of restoration | |||
| Cemented | 21 (75.0%) | 25 (89.3%) | 0.295 |
| Screwed | 7 (25.0%) | 3 (10.7%) | |
| Diameter, mm | 4.00 [4.00; 4.00] | 4.00 [4.00; 4.00] | 0.729 |
| Length, mm | 11.0 [10.0; 11.5] | 11.5 [10.8; 11.5] | 0.087 |
- Note: p-Value derived from the Wilcoxon rank sum test for continuous variables and the McNemar test for categorical ones. Bold values: statistically significant differences between groups.
- Abbreviations: ARP, alveolar ridge preservation; SH, spontaneously healed.
No statistically significant difference was observed in the need for additional bone augmentation at the time of implant placement, which was performed in six cases of the SH group (21.4%) and five of the ARP group (17.9%) (p = 1.000).
Clinical and radiographic implant-level characteristics at follow-up revealed a statistically significant difference for soft tissue recession (p = 0.023) and MBLC (p = 0.032) between the SH and ARP groups. Soft tissue recession occurrence was significantly higher in the SH group (35.7%) compared with the ARP group (7.14%) (Table 4); moreover, the SH group showed significantly higher levels of MBLC than the ARP group, with values, respectively, of 1.00 [0.25; 1.62] and 0.40 [0.00; 1.00] mm (Mean MBLC SH group: 1.506 ± 1.591 mm; Mean MBLC ARP group: 0.758 ± 0.768 mm).
| Implant level characteristics at follow-up | SH (n = 28) | ARP (n = 28) | p-Value |
|---|---|---|---|
| PSR | |||
| 0, 1, 2 | 15 (53.6%) | 16 (57.1%) | 1.000 |
| 3, 4 | 13 (46.4%) | 12 (42.9%) | |
| Soft tissue recession | |||
| No | 18 (64.3%) | 26 (92.9%) | 0.023 |
| Yes | 10 (35.7%) | 2 (7.14%) | |
| Metal exposure | |||
| No | 21 (75.0%) | 26 (92.9%) | 0.143 |
| Yes | 7 (25.0%) | 2 (7.14%) | |
| Implant health status | |||
| Healthy | 21 (75.0%) | 23 (82.1%) | 0.792 |
| Mucositis | 5 (17.9%) | 4 (14.3%) | |
| Perimplantitis | 2 (7.14%) | 1 (3.57%) | |
| Suppuration | |||
| No | 26 (92.9%) | 26 (92.9%) | 1.000 |
| Yes | 2 (7.14%) | 2 (7.14%) | |
| Visual inflammation signs | |||
| No | 21 (75.0%) | 23 (82.1%) | 0.745 |
| Yes | 7 (25.0%) | 5 (17.9%) | |
| Emergence angle mesial (mean) | 27.9 [22.9; 33.8] | 28.1 [20.7; 34.9] | 0.768 |
| Emergence angle distal (mean) | 32.8 [23.5; 42.1] | 28.0 [21.1; 32.6] | 0.321 |
| Emergence angle mesio – distal (mean) | 29.3 [24.6; 37.5] | 29.0 [21.7; 33.6] | 0.419 |
- Note: p-Value derived from the Wilcoxon rank sum test for continuous variables and the McNemar test for categorical ones. Bold values: statistically significant differences between groups.
- Abbreviations: ARP, alveolar ridge preservation; SH, spontaneously healed.
No statistically significant differences between SH and ARP groups were observed in implant health status.
The graphic representation of MBL and MBLC in the two groups is detailed in Figure 2.
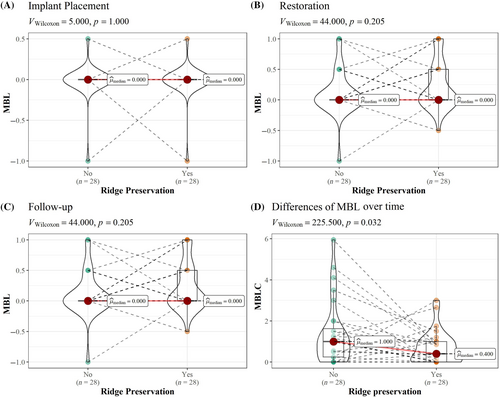
According to the Multivariate multilevel mixed-effects model, the only parameter significantly affecting MBLC was the performance of ARP. No statistically significant influence of age, gender, smoking, parafunctional habits, or prosthetic emergence angle was observed on the marginal bone level changes over time (Tables 5 and 6).
| Dependent variable: MBLC | β | SE | t Value | p-Value |
|---|---|---|---|---|
| Fixed effects | ||||
| Ridge preservation (Ref. Yes) | −0.72 | 0.32 | 2.23 | 0.026 |
| Age | 0.02 | 0.02 | 0.76 | 0.390 |
| Gender (Ref. M) | −0.78 | 0.48 | 1.61 | 0.102 |
| Smoking habits (Ref. Yes) | 0.03 | 0.43 | 0.02 | 0.946 |
| Parafunctional habits (Ref. Yes) | 0.65 | 0.38 | 1.92 | 0.084 |
| Emergence angles mean | 0.01 | 0.02 | 0.40 | 0.690 |
| Random effects | ||||
| Group | Parameter | SD | N | ICC |
| id | Intercept | 0.15 | 28 | 0.02 |
| Model fit | ||||
| AIC = 199.89 | ||||
| BIC = 217.96 | ||||
| Pseudo-R2 (fixed effects) = 0.19 | ||||
| Pseudo-R2 (total) = 0.20 | ||||
- Note: Bold values: statistically significant differences between groups.
- Abbreviations: AIC, Akaike information criterion, Est., estimate; SE, standard error.
| Predictors | DF | SS | MD | DDF | F statistic | Pr(>F) |
|---|---|---|---|---|---|---|
| Ridge preservation (Ref. Yes) | 1 | 7.40 | 7.40 | 27.10 | 5.17 | 0.031 |
| Age | 1 | 0.91 | 0.91 | 22.41 | 0.63 | 0.434 |
| Gender (Ref. M) | 1 | 3.63 | 3.63 | 22.38 | 2.54 | 0.125 |
| Smoking habits | 1 | 0.01 | 0.01 | 22.65 | 0.01 | 0.931 |
| Parafunctional habits (Ref. Yes) | 1 | 4.46 | 4.46 | 22.90 | 3.12 | 0.091 |
| Emergence angles mean | 1 | 0.23 | 0.23 | 47.01 | 0.16 | 0.692 |
- Abbreviations: DDF, denominator degrees of freedom; DF, degrees of freedom; MS, mean square; SS, sum of squares.
4 DISCUSSION
The present study highlights the potential advantages of the ARP in maintaining peri-implant tissue health and in improving marginal bone stability. In this study, ARP was primarily performed in type II alveolar sockets, whereas type I sockets were mostly left to heal spontaneously. This observation suggests that type II extraction sockets are more likely to benefit from ARP to counteract bone volume shrinkage. Implants placed in ARP-treated sites exhibited reduced buccal soft tissue recession and fewer changes in marginal bone level when compared with implants placed in pristine bone. ARP was identified as the only significant factor influencing MBLC over time, with age, gender, smoking, parafunctional habits, and prosthetic emergence angle showing no significant impact on MBLC. This underscores the possible role of ARP in maintaining a stable marginal bone level around implants, which is associated with long-term implant success.
The study also found similar stability and health status of peri-implant tissues in both grafted and non-grafted groups, consistently with other scientific reports.19, 20
A previous study by Barone and colleagues21 indicated favorable outcomes in implant survival and marginal bone stability following ARP. Buonocunto and colleagues8 showed no significant differences in the rates of mucositis and peri-implantitis around implants inserted in grafted sites compared with those in pristine bone, in accordance with the literature.19, 22
Factors potentially affecting ARP outcomes include gingival phenotype, keratinized tissue presence, mesial and distal papillae appearance, buccal bone thickness, extraction socket classification, and integrity of the buccal bone plate. These should be evaluated to ensure aesthetic and functional outcomes.23 Although various ARP protocols exist, positive treatment outcomes have been reported overall, even in cases with severe alveolar destruction.24
According to the literature, the timing of implant placement does not significantly affect implant-related outcomes; indeed, changes in average marginal bone level following immediate implant placement with bone augmentation are similar to those seen with implants placed 3 months after ARP in post-extraction sockets with buccal bony defects of 5 mm or more in the aesthetic zone.19
The need for ARP should be based on considerations of aesthetics, functionality, and associated risks, which should be assessed through a comprehensive clinical and radiographic evaluation of the extraction socket. ARP is recommended for maintaining alveolar ridge integrity, especially in cases where dental implants are planned and for supporting soft tissue around fixed dental prostheses.25
Some concerns22 have been raised regarding the lack of standardization in ARP techniques and biomaterials, as no single method can fully prevent alveolar bone resorption. Variations in study methodologies, anatomical locations, observation methods and follow-up periods complicate comparisons between specific biomaterials and methods described in several clinical trials. Nevertheless, with ARP procedures, the literature consistently reports reduced vertical and horizontal alveolar bone resorption and better preservation of keratinized tissue.
As highlighted by our results, the prosthetic emergence profile does not significantly affect MBLC. This issue has been debated extensively, with conflicting results in the literature. An emergence angle greater than 30° has been considered a significant risk factor for marginal bone loss26 and peri-implantitis development.17 However, other studies underlined that, with an adequate emergence profile in the anterior area, peri-implant soft tissue health is not influenced by the emergence angle.27 Indeed, it should be noted that radiographic assessment of the emergence profile is performed on bidimensional images at the mesial and distal angles of the prosthetic rehabilitation, which may not fully capture the potential influence of the buccal emergence angle. Nonetheless, the present study aligns with existing evidence, supporting the concept that the prosthetic emergence profile does not impact MBLC.
However, the present study has several limitations. First, while allowing for adequate follow-up, the retrospective design relied on the availability and accuracy of medical records. Second, the extraction socket types were heterogeneous, and the teeth involved predominantly molars and premolars. Finally, the timing of study follow-up varied among groups. Indeed, addressing the limitations above through future prospective clinical studies will be crucial for strengthening the clinical recommendations for ARP procedures.
5 CONCLUSION
In our sample, ARP demonstrated superiority in preserving peri-implant tissues and preventing marginal bone loss when compared with SH. These findings suggest the possibility to integrate ARP techniques in routine dental practice, particularly in cases where implant placement is anticipated following extraction. However, further research with a larger sample size, a randomized design and longer follow-up periods is warranted to corroborate these findings and refine clinical protocols for optimal patient care.
AUTHOR CONTRIBUTIONS
All authors have made substantial contributions to the conception and design of the study. AB was involved in patients' treatments. CC and RI have been involved in data collection and patient examination. AP performed the statistical analysis. RI, CC and MN have been involved in data interpretation and manuscript drafting. GI has been involved in data interpretation and critically revised the manuscript. All authors have given final approval for the version to be published and agreed to be accountable for all aspects of the work.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
Supporting data is not available due to the nature of the research and participants' privacy.