Osseodensification versus lateral window technique for sinus floor elevation with simultaneous implant placement: A randomized clinical trial on patient-reported outcome measures
Abstract
Objectives
To compare patient-reported outcome measures and additional surgical outcomes after sinus floor elevation (SFE) with osseodensification (OD) versus lateral window (LW), both with simultaneous implant placement.
Materials and Methods
Twenty participants requiring single-implant rehabilitation with residual bone height (RBH) ≤4 mm were enrolled. Pain experience, quality of life (QoL) via the Oral Health Impact Profile-14 (OHIP-14), analgesics intake, and other symptoms were self-reported for a week on a daily basis. Surgery duration, complications, and implant stability quotient at baseline (ISQ T0) and after 6 months (ISQ T6) were registered. Participants were followed up for 1 year.
Results
From Day 0 (day of surgery) to Day 3, pain experience was significantly lower (p < 0.05) in the OD group. OHIP-14 score was significantly lower (p < 0.05) in the OD group on all postoperative days, except on Day 5. Average analgesics intake was significantly lower (p < 0.001) in the OD group. Surgery mean duration was significantly higher (p < 0.001) in LW compared to OD (71.1 ± 10.4 vs. 32.9 ± 5.3 min). After osseointegration period, all implants were successfully restored with screw-retained crowns.
Conclusions
Within the limitations of this study, it can be concluded that OD and LW techniques were similarly effective in SFE with simultaneous implant placement when RBH ≤ 4 mm. However, OD significantly outperformed LW in pain experience, impact on self-perceived QoL, surgery duration, postoperative edema, and analgesics intake.
Summary Box
What is known
Lateral window technique is a safe and predictable treatment modality for sinus floor elevation and is still considered the gold standard approach when residual bone height ≤4 mm. However, it has some drawbacks since it is often associated with considerable patient morbidity.
What this study adds
This study demonstrated that osseodensification is as effective as the lateral window technique for sinus floor elevation with simultaneous implant placement when residual bone height ≤4 mm, but with significantly improved patient-reported outcome measures.
1 INTRODUCTION
The edentulous posterior maxilla is often associated with limited bone availability, particularly in terms of residual bone height (RBH) below the maxillary sinus floor. This happens not only due to the resorption of the alveolar ridge following tooth extraction but also due to sinus pneumatization which may occur.1, 2 Furthermore, bone density in this area is usually low which represents an additional challenge for proper implant placement.3 Maxillary sinus floor elevation (SFE) is an effective and safe surgical procedure to vertically increase bone height either through a lateral or crestal approach,4-6 which are both associated with high implant survival rates.6-8 The classical SFE procedure by a lateral window (LW) approach was first presented in the 1970s by Tatum9 and later published and described in more detail by Boyne and James in 1980.10 It is still widely used nowadays and historically considered the gold-standard technique in cases with RBH <5 mm.11-13 However, this surgical approach has some drawbacks since it is often associated with substantial patient morbidity. It requires a wide mucoperiosteal flap with at least one vertical releasing incision for the creation of a bony window in the lateral wall of the maxillary sinus which may result in an increased risk of postoperative pain, facial edema, delay in healing, bleeding, and postoperative infection.14-16 The more conservative transcrestal SFE approach was first proposed in 19769 and later modified by Summers in 199417 through the use of tapered osteotomes to fracture the maxillary sinus floor and elevate the Schneiderian membrane. Traditionally, this technique has been recommended in patients with at least 5 mm of RBH11, 13, 18 and is not indicated in cases with an oblique sinus floor due to the high risk of membrane perforation.18 Moreover, the repeated tapping of the osteotomes with the uncontrolled force for the fracture of the sinus floor may provoke benign paroxysmal positional vertigo (BPPV), which can be incapacitating causing considerable stress to the patient.19, 20 Nevertheless, besides the limited intraoperative visibility, SFE by crestal approach has several advantages compared with the LW approach, namely being less surgically invasive, having less potential for risk of infection,8 and allowing the preservation and full maintenance of the buccal bone (with possible increase in the healing speed).21-23 Thus, several transcrestal alternative techniques have emerged to overcome the disadvantages from the original Summers' method.24, 25 Despite reported successful outcomes, these conventional methods for SFE are not able to enhance bone density, which is often reduced in the posterior maxilla.26
Osseodensification (OD) is a novel surgical technique for implant site preparation that preserves bone by using specially designed burs in counterclockwise (CCW; noncutting motion) with copious irrigation.26 Contrary to conventional drilling techniques, OD promotes bone compaction along the osteotomy walls and into the trabecular spaces, increasing the bone density at the site. A recent multicenter controlled clinical trial showed that OD demonstrated significantly higher implant insertion torque (IT) and primary stability values than standard subtractive drilling, regardless of the jaw and area operated.27 This is in accordance with a recent systematic review in which OD presented consistently higher implant stability quotient (ISQ) at baseline and 4–6 months after implant placement compared with conventional drilling.28 With OD site preparation, the osteotomy is gradually expanded both in lateral and apical direction26, 29-31 so it can be used not only for ridge expansion but also for sinus lift by crestal approach in a safe and predictable way with reduced morbidity.25, 32
Although OD has demonstrated good results in sinus elevation in cases with very reduced RBH,25, 33 the minimum bone height for the safe use of this technique is not yet well established in the literature. Considering the several advantages over the classic LW technique, especially in terms of potentially reducing patient morbidity, it would be interesting to understand to what extent it is possible to use this technique in more extreme cases in which the LW is still considered the gold standard approach.11-13 Thus, the aim of this randomized clinical trial was to compare pain experience after SFE with OD versus LW, both with simultaneous implant placement in similar conditions (RBH ≤4 mm). Secondary outcome measures included other patient-reported outcome measures (PROMs), implant stability, surgery duration, intraoperative and postoperative complications, and analgesics intake.
2 MATERIALS AND METHODS
2.1 Study design
This randomized controlled clinical trial was conducted at the University Clinic of Egas Moniz School of Health and Science (Almada, Portugal), between September 2020 and February 2023. Ethical approval was provided by the Egas Moniz Ethics Committee (no. 859/2020) in accordance with the Helsinki Declaration, as revised in 2013. All participants were fully informed about the study and provided a written informed consent before participation in the trial. The study was registered in the ISRCTN registry (registration number ISRCTN35171361) and is reported according to the Consolidated Standards of Reporting Trials 2010 guideline (CONSORT, www.consort-statement.org). Surgeries were performed between September 2020 and July 2022.
The null hypothesis was established as: in maxillary SFE with simultaneous implant placement when RBH ≤4 mm, OD shows similar pain experience to the LW technique.
2.2 Participants
Panoramic radiographs and cone-beam computed tomography (CBCT) were used for initial participants screening. Participants were recruited according to the following inclusion criteria: (1) age ≥18, systemically healthy; (2) absence of tooth in the posterior maxilla; (3) RBH ≤4 mm; and (4) crestal bone width >6 mm. The exclusion criteria were: (1) RBH >4 mm; (2) smoking more than 10 cigarettes/day; (3) uncontrolled and/or untreated periodontal disease; (4) pregnant or lactating women; (5) history of alcoholism or drug abuse during the past 5 years; (6) hypertension or uncontrolled diabetes; (7) maxillary sinus pathology; (8) temporomandibular joint pathology; (9) patients with malignant tumors; (10) patients taking bisphosphonates or daily steroids; (11) patients with a history of chemotherapy or radiation therapy in the past 5 years. RBH was measured on CBCT in the sagittal section corresponding to the digitally planned implant position. Participants were followed up for 1 year.
2.3 Randomization and blinding
Participants enrolled in the study were randomly allocated in a 1:1 ratio into either the test group (OD) or the control group (LW) with a computer-generated randomization list (https://www.randomizer.org/). Allocation concealment was performed using sealed and opaque numbered envelopes which were opened by the surgeon immediately before the surgery. Participants were blinded to group allocation.
2.4 Surgical procedure
All surgical and prosthetic procedures were performed by one experienced clinician (J.G.). Both SFE techniques (OD and LW) were performed with simultaneous implant placement.
2.4.1 Presurgical phase
All participants underwent prophylactic antibiotics (2 g of amoxicillin 1 h presurgery). Patients rinsed with chlorhexidine digluconate solution (0.2%) for 1 min.
2.4.2 Surgical phase
All surgeries were performed under local anesthesia with articaine hydrochloride 4% with epinephrine (1:100.000).
2.4.3 LW protocol
- Mid-crestal incision and a mesial vertical releasing incision using a #15 blade, followed by an intrasulcular incision around the distal tooth. In the absence of a tooth distally to the edentulous area, a small vertical incision was performed.
- After elevation of a full-thickness mucoperiosteal flap and exposure of the alveolar crestal and the lateral wall of the maxillary sinus, a window was created using a piezoelectric device with a round diamond tip to reach the Schneiderian membrane (Figure 1B). If buccal bone thickness was >1.5 mm, a rotating diamond bur mounted in a handpiece was used for the initial window outline before the final refinement with the piezoelectric tip.
- Schneiderian membrane was then carefully elevated with hand curettes until reaching the medial sinus wall, along with the outlined window which was pushed inwards the sinus cavity. The eventual occurrence of membrane perforations was evaluated during the surgical procedure. Whenever a minor perforation was observed, a resorbable collagen membrane (Bio-Gide®; Geistlich Pharma, AG, Switzerland) was used for its repair. If a large perforation (>10 mm) with massive communication to the sinus cavity occurred, the patient was withdrawn from the study. After adequate membrane elevation, implant site preparation was performed with a traditional undersized drilling protocol (Figure 1C).
- Sinus was then grafted with a synthetic particulate bone substitute composed of calcium phosphosilicate (NovaBone® Morsels) followed by the placement of a conical implant with a platform switched morse-taper connection (IDCAM ST, Implant Diffusion International, Montreuil, France), which was left submerged according to a two-stage protocol (Figure 1D).
- A resorbable collagen membrane (Bio-Gide®; Geistlich Pharma, AG, Switzerland) was then applied to cover the created window, and the flap was repositioned and sutured with nonresorbable monofilament suture (Seralon® 4–0, Serag-Wiessner, Naila, Germany) by primary intention closure (Figure 1E).
- Implants were submerged and no provisional restoration was used during the healing period. Periapical radiographs and CBCT were taken immediately after the surgery and sutures were removed after 7–10 days.
- Patients received then the postoperative instructions and medication.
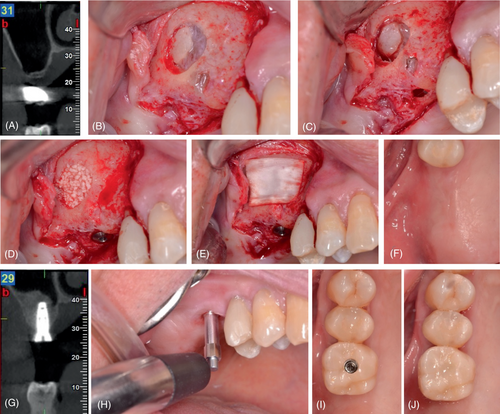
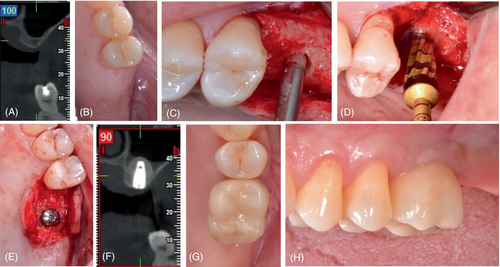
2.4.4 OD protocol
- A limited full-thickness mucoperiosteal flap to expose the alveolar crest was elevated after a mid-crestal and intrasulcular incisions on the adjacent teeth (Figure 2C).
- The implant site was prepared with Densah® Burs (Versah, LLC, Jackson, MI, USA) running in CCW, at 1200 rpm with copious irrigation, according to the manufacturer instruction (described in Densah Sinus Lift Protocol III provided by Versah®). Due to the reduced RBH and according to the protocol, the use of a pilot drill and narrower Densah® burs (2.0 and 2.3) is not recommended. The Densah® bur used to advance past the sinus floor and propel the graft material was chosen based on the implant diameter selected for the site (Figure 2D).
- After gently interrupting the sinus floor, the last densifying bur of the sequence was used in CCW at 100 rpm without irrigation to propel the synthetic bone graft (NovaBone® Dental Putty), advancing no more than 3 mm beyond the initial bone height regardless of the intended elevation (Figure 2C).
- After the placement of a 0.5-cc cartridge, a periapical radiograph was taken intraoperatively to assess the need for additional grafting prior to implant placement.
- Implants were submerged and no provisional restoration was used during the healing period. Periapical radiographs and CBCT were taken immediately after the surgery and sutures were removed after 7–10 days (Figure 2E,F).
- Patients received then the postoperative instructions and medication.
2.5 Postoperative instructions and medication protocol
Participants were instructed to use a cold-pack for the first 24–36 h and a mouth rinse with 0.12% chlorhexidine digluconate solution twice daily for 7 days. Antibiotics were prescribed for all patients (1 g amoxicillin every 12 h for 7 days). A rescue tablet of 600 mg ibuprofen was given to all patients immediately after the surgery. For post-surgical pain control, patients were instructed to take painkillers pro re nata, as deemed necessary (ibuprofen 600 mg every 12 h, supplemented by paracetamol 1000 mg in case of pain peaks). Analgesics use was recorded from the day of the surgery until 7 days after surgery.
2.6 Outcomes
2.6.1 Pain experience and other patient-reported outcome measures
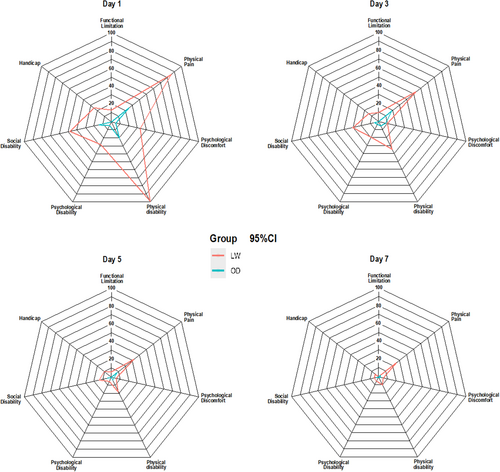
Pain experience after surgery was defined as the primary outcome of this study and daily measured by the participants using a visual analogue scale (VAS) score (0–10, from “No pain” to “Worst pain ever experienced”) in the first postoperative 7 days, with Day 0 being the day of the surgery. Before going to sleep, patients were asked to mark the VAS that best represented the average pain they had experienced during the day. Furthermore, PROMs were additionally appraised by means of postoperative patients' quality of life (QoL). QoL was measured through a modified version of the Oral Health Impact Profile-14 (OHIP-14) questionnaire (see Supplementary Information) which was also daily filled in by the participants in the first 7 days following surgery. The OHIP-14 questionnaire covers 7 domains out of 14 items of oral health impact: functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap. Each item is rated on a 5-point Likert scale coded as follows: 0, never; 1, hardly ever; 2, occasionally; 3, fairly often; and 4, very often. The OHIP-14 total score is then calculated as the sum of the 14 scores (from 0 to 56), with a higher score indicating more negative impact and a lower oral health-related quality of life (OHRQoL). Symptoms such as edema/swelling, hematoma, and epistaxis were also self-reported by patients for 7 days after surgery using a 5-point Likert scale (none, little, moderate, intense, and very intense).
2.6.2 Secondary outcome measures
- ISQ, recorded using resonance frequency analysis (Osstell™; Osstell AB, Gothenburg, Sweden) immediately after implant placement (ISQ T0—primary stability) and following implant exposure after 6 months of healing (ISQ T6—secondary stability), as the average between buccolingual and mesiodistal measures. If ISQ T6 was ≥68, the final impression was made and implants were loaded with screw-retained zirconia crowns. If ISQ T6 value was lower, patients were recalled for a new measurement every 3 weeks until reaching the minimum value established for the final restoration.
- Implant IT measured by surgical drill unit or manual torque wrench.
- Implant osseointegration success rate.
- Patients' registration of analgesics intake during the first week after surgery.
- Duration of surgical procedure, from the initial incision to the completion of the suture.
- Intraoperative complications as Schneiderian membrane perforation or excessive bleeding.
- Postoperative complications as infection, BPPV, early exposure of cover screw or implant failure.
2.7 Sample size
Due to the lack of trials focusing on pain self-report between OD and LW as primary outcome, the relatively limited number of eligible patients within the eligibility criteria and reasonable difference between a minimum invasive approach (OD) and a more invasive one (LW), we considered a Cohen's large effect size (d = 1.4), between LW and OD VAS score distribution. For a power of 80% and a significance level of 5%, the minimum number of participants was determined as 8 participants per group. Assuming a possible 20% dropout during the follow-up period, the final number was established 10 participants per group, in a total of 20 participants.
2.8 Statistical analysis
Data were analyzed by using descriptive and inferential statistical methodologies. For inter-group comparison, the inferential procedure was chosen according to variable typology and data distribution. A nonparametric comparison procedure (Mann–Whitney test) was considered for ordinal variables and for continuous variables since these exhibited no adequacy to normality. Chi-square and Fisher's exact test were used to evaluate association for categorical variables. R ggplot2 package was used for data visualization. Specifically, scatterplots and radar plots were used to visualize data distribution between the groups. A 5% significance level was established for all inferential analyses.
3 RESULTS
3.1 Participants and baseline data
Twenty participants (8 men and 12 women) with a mean age of 47.9 years old (±12.7; range from 24 to 66) were enrolled in the study (Table 1). We did not observe dropouts and all participants completed the follow-up appointments. There were no significant differences (p > 0.05) between the groups according to gender, age, RBH, or missing tooth. Mean RBH was 2.9 ± 0.5 mm (range: 2–3.5 mm) in the OD group and 2.4 ± 0.7 mm (range: 1.5–3.5 mm) in the LW group (p = 0.098). All implants placed in both groups were 10 mm in length.
| OD | LW | p-value | |
|---|---|---|---|
| Age (years), mean (SD) [min–max] | 51.2 (12.6) [23–66] | 44.6 (12.5) [28–66] | 0.197 |
| Gender, n (%) | |||
| Males | 5 (50.0) | 3 (30) | 0.648 |
| Females | 5 (50.0) | 7 (70) | |
| Maxillary tooth location | |||
| 16 | 4 (40) | 3 (30) | 0.478 |
| 26 | 5 (50) | 7 (70) | |
| 17 | 1 (10) | 0 (0) | |
| Residual bone height, mean (mm) | 2.9 (0.5) | 2.4 (0.7) | 0.098 |
- Abbreviations: LW, lateral window; OD, osseodensification.
3.2 Patient-reported outcomes
3.2.1 Pain experience and analgesics intake
Figure 3 shows the evolution of pain experience daily self-reported by patients using a VAS. From Day 0 (the day of the surgery) to Day 3, pain experience was significantly lower (p < 0.05) in the OD (Table 2). Average analgesics intake during the week after surgery was significantly lower (p < 0.001) in OD (two tablets of 600 mg ibuprofen) compared to LW (eight tablets of 600 mg ibuprofen + 1 tablets of 1000 mg paracetamol). Only participants from the LW group (30%; n = 3) took paracetamol in addition to the nonsteroidal anti-inflammatory drugs (NSAIDs).

| Pain (VAS) | LW mean (SD) | OD mean (SD) | p-value |
|---|---|---|---|
| Day 0 | 2.8 (1.0) | 1.1 (1.7) | 0.0126 |
| Day 1 | 2.1 (0.9) | 0.7 (1.6) | 0.0494 |
| Day 2 | 1.9 (0.7) | 0,3 (1.9) | 0.0312 |
| Day 3 | 1.7 (0.0) | 0.0 (1.9) | 0.0082 |
| Day 4 | 1.2 (0.0) | 0.0 (1.6) | 0.0588 |
| Day 5 | 1.0 (0.0) | 0.0 (1.3) | 0.0588 |
| Day 6 | 0.5 (0.0) | 0.0 (1.1) | 0.4497 |
| Day 7 | 0.2 (0.0) | 0.0 (0.4) | 0.4497 |
- Abbreviations: LW, lateral window; OD, osseodensification; SD, standard deviation; VAS, visual analogue scale.
3.2.2 Oral health-related quality of life
The evolution of the overall score and each super-domain of OHIP outcomes between OD and LW groups is shown in Figure 4. According to OHIP-14 total score, the impact in participants' QoL after surgery was significantly lower (p < 0.05) in the OD group on all seven postoperative days, except on Day 5. These results were also observed for OHIP physical and psychological super-domains. Regarding the OHIP social super-domain, the score was only significantly different (p < 0.01) on Day 0 and Day 1 (Table 3). Figure 5 and Table 4 show the differences between the two groups for each OHIP-14 domain (functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap).
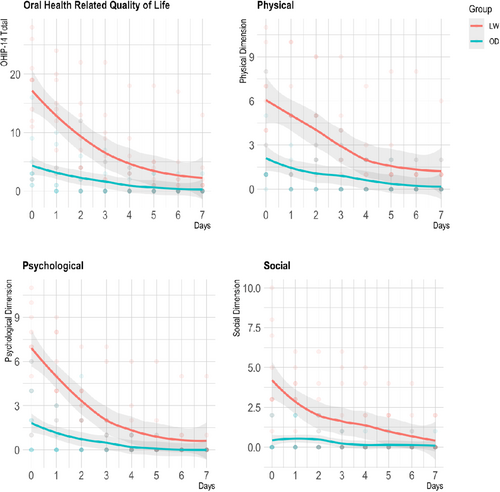
| Day | Group | OHIP-14 total, mean (SD) | p-value | OHIP-14 physical, mean (SD) | p-value | OHIP-14 psychological, mean (SD) | p-value | OHIP-14 social, mean (SD) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| 0 | LW | 17.1 (7.6) | 0.0023 | 6.1 (3.1) | 0.0085 | 6.8 (3) | 0.0018 | 4.2 (3.2) | 0.0011 |
| OD | 4.5 (4.7) | 2.2 (2.5) | 1.9 (2.1) | 0.4 (0.8) | |||||
| 1 | LW | 13.1 (6.9) | 0.0014 | 4.9 (3.5) | 0.0117 | 5.3 (2.4) | 0.0003 | 2.9 (2.0) | 0.0068 |
| OD | 2.7 (3.6) | 1.2 (1.7) | 0.9 (1.3) | 0.6 (1.0) | |||||
| 2 | LW | 9.0 (6.6) | 0.01237 | 4.1 (3.1) | 0.01942 | 3.1 (1.9) | 0.01034 | 1.8 (2.0) | 0.1049 |
| OD | 2.6 (3.9) | 1.2 (1.8) | 0.9 (1.7) | 0.5 (0.8) | |||||
| 3 | LW | 6.9 (6.9) | 0.02379 | 3.0 (2.7) | 0.03503 | 2.1 (2.5) | 0.04167 | 1.8 (2.3) | 0.09126 |
| OD | 1.5 (2.6) | 0.9 (1.5) | 0.4 (0.7) | 0.2 (0.4) | |||||
| 4 | LW | 4.4 (5.6) | 0.02345 | 1.8 (2.1) | 0.00789 | 1.3 (1.9) | 0.04321 | 1.3 (1.9) | 0.06543 |
| OD | 0.9 (1.5) | 0.6 (1.0) | 0.2 (0.4) | 0.1 (0.3) | |||||
| 5 | LW | 3.6 (5.4) | 0.05704 | 1.7 (2.4) | 0.05546 | 0.9 (1.9) | 0.2339 | 1.0 (1.4) | 0.1907 |
| OD | 0.7 (1.3) | 0.4 (0.8) | 0.1 (0.3) | 0.2 (0.4) | |||||
| 6 | LW | 2.8 (5.2) | 0.03309 | 1.4 (2.4) | 0.03605 | 0.7 (1.6) | 0.06789 | 0.7 (1.3) | 0.2339 |
| OD | 0.3 (0.9) | 0.2 (0.6) | 0.0 (0.0) | 0.1 (0.3) | |||||
| 7 | LW | 2.2 (4.0) | 0.03291 | 1.2 (1.8) | 0.03605 | 0.6 (1.6) | 0.1468 | 0.4 (0.8) | 0.4652 |
| OD | 0.3 (0.9) | 0.2 (0.6) | 0.0 (0.0) | 0.1 (0.3) |
- Abbreviations: LW, lateral window; OD, osseodensification; OHIP-14, Oral Health Impact Profile-14.
| T | Group | Functional limitation, mean (SD) | p-value | Physical pain, mean (SD) | p-value | Psychological discomfort, mean (SD) | p-value | Physical disability, mean (SD) | p-value | Psychological disability, mean (SD) | p-value | Social disability, mean (SD) | p-value | Handicap, mean (SD) | p-value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | LW | 1.0 (1.2) | 0.0198 | 4.0 (1.6) | 0.0083 | 2.2 (1.8) | 0.0346 | 4.4 (2.4) | 0.0031 | 1.3 (1.3) | 0.0877 | 2.6 (1.5) | 0.0011 | 1.6 (2.0) | 0.0181 |
| OD | 0.1 (0.3) | 1.6 (1.5) | 0.8 (1.6) | 1.2 (1.1) | 0.4 (0.7) | 0.3 (0.7) | 0.1 (0.3) | ||||||||
| 1 | LW | 0.5 (1.1) | 0.1468 | 3.4 (2.3) | 0.0152 | 1.3 (1.3) | 0.0322 | 3.9 (1.8) | 0.0003 | 1.1 (1.2) | 0.0474 | 1.9 (1.2) | 0.0172 | 1.0 (0.9) | 0.0017 |
| OD | 0.0 (0.0) | 1.0 (1.3) | 0.2 (0.4) | 0.7 (0.9) | 0.2 (0.4) | 0.6 (1.0) | 0.0 (0.0) | ||||||||
| 2 | LW | 0.7 (1.1) | 0.0304 | 2.7 (1.7) | 0.0279 | 0.6 (0.8) | 0.4002 | 2.2 (1.5) | 0.0075 | 1.0 (1.1) | 0.0783 | 1.2 (1.2) | 0.1567 | 0.6 (1.1) | 0.0682 |
| OD | 0.0 (0.0) | 1.0 (1.4) | 0.4 (1.0) | 0.4 (0.7) | 0.3 (0.7) | 0.5 (0.8) | 0.0 (0.0) | ||||||||
| 3 | LW | 0.4 (1.0) | 0.1468 | 2.1 (1.4) | 0.0306 | 0.4 (0.7) | 0.6538 | 1.4 (1.3) | 0.0154 | 0.8 (1.2) | 0.1108 | 1.2 (1.7) | 0.1085 | 0.6 (1.1) | 0.0682 |
| OD | 0.0 (0.0) | 0.7 (1.2) | 0.3 (0.7) | 0.2 (0.4) | 0.1 (0.3) | 0.2 (0.4) | 0.0 (0.0) | ||||||||
| 4 | LW | 0.3 (0.7) | 0.0012 | 1.3 (1.2) | 0.0457 | 0.2 (0.6) | 0.0123 | 1.0 (1.4) | 0.0346 | 0.3 (0.7) | 0.0099 | 0.9 (1.4) | 0.0568 | 0.4 (0.7) | 0.0023 |
| OD | 0.0 (0.0) | 0.4 (0.7) | 0.2 (0.4) | 0.2 (0.4) | 0.0 (0.0) | 0.1 (0.3) | 0.0 (0.0) | ||||||||
| 5 | LW | 0.2 (0.6) | 0.3173 | 1.3 (1.3) | 0.0332 | 0.2 (0.6) | 0.9422 | 0.7 (1.3) | 0.2339 | 0.2 (0.6) | 0.3173 | 0.6 (0.8) | 0.2604 | 0.4 (0.7) | 0.0679 |
| OD | 0.0 (0.0) | 0.3 (0.7) | 0.1 (0.3) | 0.1 (0.3) | 0.0 (0.0) | 0.2 (0.4) | 0.0 (0.0) | ||||||||
| 6 | LW | 0.2 (0.6) | 0.3173 | 1.0 (1.2) | 0.0198 | 0.2 (0.6) | 0.9422 | 0.5 (1.0) | 0.0679 | 0.2 (0.6) | 0.3173 | 0.4 (0.7) | 0.2548 | 0.3 (0.7) | 0.1468 |
| OD | 0.0 (0.0) | 0.1 (0.3) | 0.1 (0.3) | 0.0 (0.0) | 0.0 (0.0) | 0.1 (0.3) | 0.0 (0.0) | ||||||||
| 7 | LW | 0.0 (0.0) | NA | 1.0 (1.2) | 0.0198 | 0.2 (0.6) | 0.9422 | 0.4 (1.0) | 0.1468 | 0.2 (0.6) | 0.3173 | 0.2 (0.4) | 0.5416 | 0.2 (0.4) | 0.1462 |
| OD | 0.0 (0.0) | 0.1 (0.3) | 0.1 (0.3) | 0.0 (0.0) | 0.0 (0.0) | 0.1 (0.3) | 0.0 (0.0) |
- Abbreviations: LW, lateral window; OD, osseodensification; OHIP-14, Oral Health Impact Profile-14; SD, standard deviation.
3.2.3 Other postoperative symptoms
Overall, participants in the LW group significantly experienced more edema (p < 0.001; mean average days with edema = 7.0 in LW and 0.5 in OD), as described in Table 5. In the OD group, 50% (n = 5) of the patients did not report any swelling on any of the seven postoperative days while all patients (100%) in the LW group reported some degree of swelling from Day 0 to Day 4. Moreover, the LW group also experienced significantly more hematoma/bruising (p < 0.001) and epistaxis were only reported by patients (40%; n = 4) in the LW group (Table 5).
| OD | LW | p-value | |
|---|---|---|---|
| Implant insertion torque (Ncm), mean (SD) | 48.0 (17.8) | 31.8 (16.0) | 0.062 |
| ISQ, mean (SD) | |||
| T0 (baseline) | 65.5 (11.1) | 61.5 (10.9) | 0.184 |
| T6 (6 months) | 74.4 (4.0) | 69.8 (5.1) | 0.046 |
| Δ[T6–T0] | 9.2 (11.5) | 8.6 (8.0) | 0.818 |
| Surgery time (min), mean (SD) | 32.9 (5.3) | 71.1 (10.4) | <0.001 |
| Medication usage in 7 days, median (IQR) | 2.0 (1.0) | 7.5 (6.5) | <0.001 |
| Average days using pain medication, median (IQR) | 1.0 (0.8) | 4.5 (2.0) | <0.001 |
| Surgical complications | |||
| Schneiderian membrane rupture, % (n) | 10.0 (1) | 40.0 (4) | <0.001 |
| Postoperative symptoms | |||
| Edema, % (n) | 50.0 (5) | 100.0 (10) | <0.001 |
| Average days (n), mean (SD) | 0.5 (2.8) | 7.0 (2.0) | <0.001 |
| Hematoma, % (n) | 10.0 (1) | 30.0 (3) | <0.001 |
| Average days (n), mean (SD) | 0.0 (0.0) | 0.0 (0.5) | <0.001 |
| Epistaxis, % (n) | 0.0 (0) | 40.0 (4) | <0.001 |
| Average days (n), mean (SD) | 0.0 (0.0) | 0.0 (2.0) | <0.001 |
- Note: Mann–Whitney test.
- Abbreviations: IQR, interquartile range; ISQ, implant stability quotient; LW, lateral window; OD, osseodensification; SD, standard deviation.
3.3 Surgery duration
The mean duration of the surgical procedure was significantly shorter (p < 0.001) in the OD group compared to the LW group (32.9 ± 5.3 vs. 71.1 ± 10.4 min) (Table 5).
3.4 Clinical outcomes and complications
There was no significant difference between the groups in terms of IT (p = 0.062) and ISQ T0 (p = 0.184), although mean values were higher in the OD group for both parameters. ISQ T6 was significantly higher (p < 0.05) in the OD group (74.4 ± 4.0) compared to LW (69.8 ± 5.1) (Table 5).
Regarding surgical intraoperative complications, there were significantly more Schneiderian membrane perforations in LW (p < 0.001) (Table 5). No other types of intraoperative complications were observed in both groups.
Early exposure of cover screw was detected in two implants (one in OD and one in LW) 3 weeks after surgery. All the remaining implants healed uneventfully, with an overall osseointegration success rate of 100%. All implants were successfully restored with screw-retained zirconia crowns.
4 DISCUSSION
Although the OD technique has demonstrated promising results for SFE with reduced RBH,25, 33 the LW technique has still been considered the gold standard approach when the RBH is less than 5 mm despite the associated patient morbidity.11-13 Therefore, the purpose of this randomized clinical trial was to compare PROMs and clinical parameters after SFE by crestal approach with OD versus LW technique, both with simultaneous implant placement in similar local conditions (RBH ≤ 4 mm).
According to a systematic review on PROMs after SFE, moderate patients' discomfort mainly expressed by pain and edema should be expected.34 In this study, the overall impact of SFE on patients' QoL was significantly lower in the OD group. Crestal approach with OD also resulted in significantly lower VAS scores for pain experience from Day 0 to Day 3 and significantly less need for analgesics intake compared to the LW technique. On Day 4, the mean VAS score for pain experience in the LW group was still greater than the overall highest mean score in the OD group, registered on Day 0.
Regarding postoperative symptoms (edema, hematoma, and epistaxis) self-reported by patients, all were significantly more prevalent in the LW group; in fact, epistaxis was only referred by patients (n = 4) in this group, presumably due to the higher incidence of membrane perforation observed. The difference in postoperative edema may be explained by the flap design which included a vertical releasing incision in the LW group but also by the duration of the surgical procedure which was on average more than twice as compared to the OD group (p < 0.001). In the LW group, all patients (100%) reported some degree of swelling from Day 0 to Day 4 while 50% (n = 5) of the patients did not report any edema on any of the seven postoperative days. These results are in accordance with another randomized clinical trial16 that also reported a significantly lower incidence of swelling, bruising, and nasal discharge/bleeding with transcrestal SFE compared to the lateral approach.
Among the potential intraoperative complications during SFE reported in the literature, sinus membrane perforation is the most common.35 In fact, it was the only intraoperative complication observed in both groups of this study, with a higher incidence in the LW (40%; n = 4) than in the OD group (10%; n = 1) (p < 0.001). This is in accordance with previous clinical trials that also showed a higher prevalence of this complication in LW compared to transcrestal approach.18, 36 The detection of sinus membrane perforations may be difficult in the crestal approach due to limited visibility.40 In our study, only one perforation was reported in the OD group since all the remaining cases had the grafting material fully contained in the immediate postoperative periapical radiograph. In the LW group, all perforations occurred during the elevation phase with manual curettes and not during antrostomy with the piezo device which was demonstrated to be extremely safe as reported in the literature.22, 37 A resorbable collagen membrane was used for perforation repair during surgery and its occurrence did not affect implant osseointegration. According to several authors,38, 39 sinus membrane perforations, if properly managed and repaired, do not appear to influence vital bone formation and implant survival. On the other hand, the single membrane perforation in the OD group was only detected in the postoperative periapical radiograph and therefore could not be repaired. However, the patient was followed during the healing period and it did not result in any type of complication. Six months after the surgery, before implant exposure, a CBCT was taken which did not reveal extruded grafting material into the sinus cavity.40
Regarding the bone grafting material in SFE, there seems to be no difference in the literature on implant treatment outcome with synthetic bone substitutes compared with other materials such as xenografts.41-43 In this study, a synthetic calcium phosphosilicate bone substitute was used in two different delivery options: putty for the transcrestal approach with OD and particulate for the LW approach. The putty delivery option is extremely user-friendly and particularly indicated for transcrestal approach since it is applied directly into the osteotomy site with a cartridge system, minimizing the potential contamination of the graft. A major possible cause for graft contamination is the use of the same instruments for flap reflection and for graft placement in the sinus. Regarding the application of the particulate grafting material in the LW technique, the surgeon (J.G.) used separate sterile instruments for that particular step of the surgical procedure to prevent graft contamination. Furthermore, the antibiotic medication protocol followed proved to be effective in preventing postoperative infections in this study.
Simultaneous implant placement during SFE is a predictable treatment modality even in cases with 1–3 mm of RBH provided meticulous surgical techniques are applied.44-47 In this study, SFE with concomitant implant placement was performed in all 20 patients (overall mean RBH of 2.7 ± 0.69 mm) and no implants were lost.
Implant site preparation with OD drilling has been shown to present higher IT and ISQ compared to conventional drilling.28, 48-50 In this study, although the mean IT and ISQ T0 values were higher in the OD group than in the LW group in which traditional osteotomy was used, the difference was not statistically significant. This may be explained by the very reduced RBH until the sinus floor for the OD technique to make a significant difference. On the other hand, ISQ T6 was significantly higher (p < 0.05) in OD group compared to LW. In fact, after the second-stage surgery, 3 implants in the LW group had ISQ T6 < 68 and therefore were not immediately restored. These patients were recalled for a new ISQ measurement after 3 weeks and two of them already had a value above the minimum established for the final impression and loading. However, 9 weeks after implant exposure, the remaining implant in the LW group persisted with an ISQ value below the threshold so our decision was to initiate a progressive loading protocol with a provisional crown out of occlusion in attempt to stimulate bone remodeling and increase ISQ. After 3 weeks, ISQ value was 73 so final impression was made and the implant was restored with a screw-retained zirconia crown. One possible reason for this apparent faster osseointegration in the OD group may be the full maintenance of the buccal wall of the sinus, contrary to the LW technique. Although we can infer that healing and graft maturation in SFE seems to be faster with OD compared to LW, these results should be further studied in future preclinical and clinical research.
A resorbable collagen membrane was used to cover the window in the LW group. Although implant survival rate seems not to be significantly influenced by the use of a barrier membrane for antrostomy coverage,51 it may reduce the postoperative displacement of the grafting material and increase the percentage of newly formed bone by reducing the proliferation of nonmineralized tissue.52, 53
Unintentional early exposure of cover screw occurred in two implants (one in each group) and were detected 3 weeks after surgery. Patients were instructed to perform meticulous plaque control, apply 0.2% chlorhexidine gel twice a day and were examined every 2 weeks for the first 2 months followed by a monthly check-up to assess the need of intervention. As described in the literature,54, 55 these implants ended up having slightly more marginal bone loss; however, the prompt diagnosis and the regular recalls allowed to prevent further severe complications. All the remaining implants healed uneventfully. After the second-stage surgery, all implants were clinically stable resulting in an overall osseointegration success rate of 100%.
Pain can be defined as a subjective experience which is dependent on several factors and on each individual. The subjectivity of PROMs in general along with the relatively small sample size can be considered the main limitations of this study. Furthermore, the experience of the surgeon may have played a role in the results since both procedures are technique-sensitive. In order to reduce as much as possible the presence of biases, the study was designed as a randomized clinical trial so participants were blinded and randomly allocated into either test or control group. In addition to the main purpose of this study, it will be interesting to follow these patients and evaluate the long-term stability of the implants.
5 CONCLUSION
Within the limitations of this study, it can be concluded that OD and LW techniques were similarly effective in SFE with simultaneous implant placement when RBH ≤ 4 mm. However, OD significantly outperformed LW in pain experience, impact on self-perceived QoL, surgery duration, postoperative edema, and analgesics intake.
AUTHOR CONTRIBUTIONS
João Gaspar: Conceptualization (lead); investigation (lead); methodology (lead); project administration (supporting); writing—original draft (supporting). Luís Proença: Formal analysis (supporting); writing—original draft (supporting). João Botelho: Formal analysis (lead); investigation (supporting); methodology (supporting); conceptualization (supporting); writing-original draft (lead). Vanessa Machado: Investigation (supporting); methodology (supporting); writing—original draft (supporting). Leandro Chambrone: Conceptualization (supporting); investigation (supporting); methodology (supporting); writing—original draft (supporting). Rodrigo Neiva: Conceptualization (supporting); investigation (supporting); methodology (supporting); writing—original draft (supporting). José João Mendes: Project administration (lead); writing—original draft (supporting).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.