Self-Management Intervention to Improve Self-Care and Quality of Life in Heart Failure Patients
Abstract
Self-management intervention is a good method to improve self-care ability, as such, to promote quality of life. However, the research focused on self-management intervention in heart failure patients in Taiwan is very limited. Therefore, the purposes of this study were to test the effectiveness of self-management intervention in patients with heart failure in Taiwan and examine the relationship between self-care ability and quality of life. A quasi-experimental design was used in this study with convenience sampling. Of the 82 subjects participating in this study, 40 of them chose to join the experimental (self-management intervention plus usual care) and 42 of them chose to join control (usual care) group. Three questionnaires were used to collect the data, which were the demographic questionnaire, the self-care questionnaire (Self-Care of HF Index V 6), and the quality of life questionnaire (Minnesota Living with Heart Failure Questionnaire). To examine the effectiveness of the intervention, self-care ability and quality of life were measured, using a pretest, 1- and 2-month follow-up assessment. Generalized estimation equations (GEE) were used to compare changes over time among groups for outcomes to ensure the effectiveness of the intervention. This study confirmed the effectiveness of the self-management intervention. The clinical provider should increase the awareness of the importance of self-management skills and self-care ability especially for heart failure patients. The designated disease-specific self-management patient book and individualize intervention should be dispensing and implementing.
Heart failure (HF) is considered an epidemic health problem1 and its incidence and prevalence have increased globally.2, 3 In 2009 in Taiwan, heart disease was among the top two leading causes of death, representing 10.6% of all deaths, with 2% from HF.4 Although there have been improvements in medical treatment and symptom management, HF patients experience poor quality of life overall.5
Pressler and colleagues6 indicated that the quality of life (QOL) among interviewed HF patients was poor, and lower levels of HF severity, younger age, and lower levels of depressive symptoms were related to better QOL. The results from an Asian study were consistent with these findings, and Chinese HF patients perceive their QOL as poor.7
Another important factor related to QOL in patients with HF is self-care.8 Self-care refers to the behaviors that individuals use to manage, condition, and promote health.9, 10 Chiaranai and colleagues11 found that better self-care was associated with a better QOL. Relative to these findings, previous research demonstrated that self-care among HF patients is considered low.12, 13 In Taiwan, Tung and colleagues14 found a low level of self-care maintenance and management, although self-care confidence was adequate.
Self-management means that patients take an active role in their treatment and are responsible for day-to-day disease management.15, 16 Both self-care and self-management embrace proactive processes to deal with health conditions and to adhere to medical treatment.17 The key difference between self-care and self-management is that self-management is more specific and refers to actively identifying symptoms and seeking medical advice.18 More recently, Smeulders and colleagues19 reported that three-quarters of participants stated that they had benefited from the program with an immediate post-program and 12-month follow-up. The authors concluded that interventions based on self-management are effective ways to enhance self-care and promote better QOL.19
Grady10 conducted a literature search for the period of 1995 to 2007 for studies that tested self-care interventions to improve QOL in HF patients. Of the 21 articles identified, 17 used random controlled trails (RCTs) and 4 used longitudinal, pre-/post-, or repeated measures designs. The findings from studies that used RCTs did not support the effects of this intervention on QOL and therefore call for further research.10 The remaining 4 studies found that while patients in both the intervention and control groups improved over time, patients in the intervention group experienced greater improvement.10
Nevertheless, research on self-management interventions for HF patients in Taiwan is very limited. Therefore, the purpose of this study was to test the effectiveness of a self-management intervention for HF patients in Taiwan based on the hypothesis that self-care and QOL would be enhanced by a self-management intervention. This study examines the effectiveness of self-management intervention in patients with HF by examining self-care and QOL as outcome measures.
Methodology
Design
An historical comparison, single-blind design, using convenience sampling, was utilized. The inclusion criteria were (1) HF for more than 6 months; (2) left ventricular ejection fraction <50%; (3) diagnosis of New York Heart Association class I, II, or III; (4) age 18 years or older; (5) able to communicate; (6) clock drawing test score >7; and (7) no major surgery within the past half year. To determine the sample size, the significance level was set at α=.05, the statistical power at 1-β=.80, and effect size at .30. Based on this, at least 58 participants should be recruited. The software used to estimate sample size was G*Power version 3.1 (Department of Criminology, University of Melbourne, Parkville, Victoria, Australia).
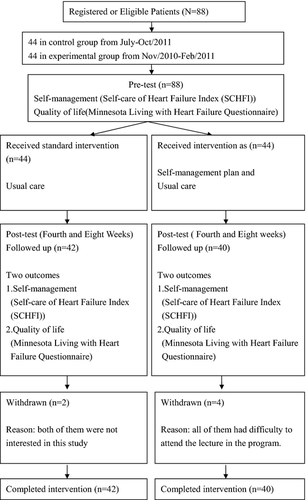
Samples
Intervention was conducted from July 2010 to February 2011, with historical comparison of outcomes. Forty-four participants in a control (usual care) group were sampled from July to October 2010 and 44 participants in an experimental (self-management intervention plus usual care) group were recruited from November to February 2011 by convenience sampling. A total of 82 participants with 40 patients in the experimental and 42 in the control group (92%) completed the program. The primary reason of using historical (nonconcurrent) comparison is to avoid sharing information between groups that might affect the results. To collect the data, 3 questionnaires were used: (1) a demographic questionnaire; (2) a self-care questionnaire (Self-Care of HF Index, V. 6); and (3) a QOL questionnaire (Minnesota Living With HF Questionnaire [MLHFQ]). To examine the effectiveness of the intervention, self-care and QOL were measured using a pretest as well as a 1-month and 2-month follow-up assessment.
Ethical Consideration
The study received ethics approval from the hospital, and all participants provided written consent. Participants were provided with both written and verbal information about the aims and process of the study prior to data collection. Participants were informed that due to the voluntary nature of their participation, they could withdraw at any time. Anonymity and confidentiality were assured.
Data Analysis
SPSS (version 17.0 for Windows, Chicago, IL) was used for all analyses. The study population was presented in terms of descriptive statistics. Nonparametric tests were used for significance testing because the sample was not normally distributed. Study outcomes included change in self-care and QOL from baseline, as measured at 1 and 2 months after the initiation of the intervention.
The generalized estimating equations (GEEs) model was used to control the effect of study covariates and analyze the independent effect of the intervention program. We used the GEE approach to consider a within-person variability and account for correlated data resulting from repeated measurements across different time points and multiple observations of the same individual.20 The GEE approach has been proposed as a nonparametric and appropriate method to conduct repeated-measurement analysis. Its main advantage (when compared with the maximum likelihood approaches) is its robustness against the working correlation structure, which must be assumed as correct for within-subject correlations. Additionally, a Mann-Whitney U test was used to examine differences in unpaired data. Differences between categorical variables were tested with a chi-square test. The significance level was set at P<.05 (2-tailed).
Self-Management Intervention
The self-management intervention consisted of 3 components that were implemented simultaneously. Participants in the experimental group were given a self-management patient book, were involved in self-management training, and received multiple follow-up telephone calls to determine the extent of their adherence to the intervention. The self-management intervention was developed by a panel of experts based on Reigel's21 situation-specific theory of HF self-care.17 The contents of the patient book and the self-management training were based on key concepts of Reigel's theory and 5 steps of the management process: recognizing a new symptom, evaluating change in health status, taking action, implementing a treatment plan, and evaluating the effects of the treatment plan.
The self-management patient book is divided into 4 chapters. The first chapter, or introduction, includes an overview of self-management and the benefits of self-management for health status. This chapter also presents the nature of home care for HF. The second chapter presents self-management skills. The third chapter covers appropriate attitudes and confidence in regards to managing the disease. It also addresses the importance of becoming an active self-manager, taking actions, and forming an action plan based on the self-management theory. The fourth chapter deals with the behavior needed to manage symptoms and illness as well as to improve compliance to treatment and promoting a healthy lifestyle. A medication log, symptoms management sheet, biological data sheet, and lifestyle pattern (diet and exercise) sheet are included in the book. In each chapter, space is provided for the participants to write about their concerns and what they learned from the program as well as to keep track of their learning progress and health status.
Each participant in the experimental group took an hour-long individual self-management skills training session twice a week for 2 weeks, totaling 4 sessions. The instructor was an acute care nurse practitioner with 12 years of working experience. The training took place in a quiet room in an outpatient clinic. These 4 sessions covered the following areas: (1) overview of the symptoms of HF and of the self-management concept; (2) assessment of the symptoms; (3) management of symptoms including appropriate attitudes to enhance self-management and to become an active self-manager; and (4) evaluation of self-management, improving adherence to treatment and promoting a healthy lifestyle.
The ongoing discipline-specific feedback regarding adherence was provided by telephone. Researchers carried out weekly follow-up telephone calls during the first month and bi-weekly follow-up phone calls during the second month, after the initiation of the intervention. Prior to initiating the intervention, its validity was assessed by an expert panel that included a cardiologist, nursing supervisor, acute care nurse practitioner, registered nurse, and a nursing doctorate faculty member.
Usual Care
Participants in the control group received usual care, which included the HF patient education sheets including the symptoms of HF and importance of adherence of treatment. Further, regular follow-up phone calls to assess adherence 1 week after the doctor appointment. They were not, however, provided with self-management training skills.
Study Instruments
Demographic Questionnaire
The demographic questionnaire consisted of two sections. The first section, filled in by the patient, included items on age, sex, religion, employee status, educational status, marital status, and economic resources. The second section, filled in by the researchers, included comorbid condition, left ventricle ejection fraction (LVEF), causes of HF, and associated clinical data drawn from the patient's record.
Self-Care of HF Index
Self-care behavior was measured by the Chinese version of the Version 6 (SCHFI-V6). The SCHFI is an ordinal, self-administered instrument that yields a performance rating score and has 3 subscales: self-care maintenance (10 items), self-care management (6 items), and self-care confidence (6 items). The reliability and validity of this instrument were confirmed in previous research and its developer recommends scoring the 3 subscales individually (scores range from 0–100) instead of determining a total summary score.21
Self-care is best represented by self-care maintenance and self-care management. Adequate self-care is indicated by a score ≥70 on each of the subscales.17, 21-23 The Chinese version of the SCHFI-V6 was first used with a Chinese HF population in a study by Tung et al (25). The results by Tung et al (25) indicated an α coefficient for internal consistency of .635 for self-care maintenance, .716 for self-care management, and .860 for self-care confidence.14 In the present study, the α coefficient was .696 for self-care maintenance, .670 for self-care management, and 946 for self-care confidence.
Minnesota Living With HF Questionnaire
QOL was measured by the MLHFQ, an HF-specific, self-report scale that measures patients' perceptions of their HF impact and its treatment on their daily life. The original MLHFQ developed by Rector and Cohn24 included 21 items divided into 2 subscales: physical QOL and emotional QOL. The score range for each item is 0 (no impact on QOL) to 5 (very high impact on QOL). The total score ranges from 0 to 105, a higher score representing a poorer QOL. The psychometric properties of original MLHFQ have been confirmed.24-27
In regard to the reliability and validity of the MLHFQ Chinese version,28 the content validity index (CVI) was .98 as confirmed by a panel of experts. In addition, the instrument was shown to have a Cronbach's α of .95 for the overall scale and .93 to .95 for the subscales. In the current study, the α coefficient was .907 for the overall scale. However, using factor analysis, Ho and colleagues29 identified 3 dimensions (physical, emotional, and social) of the Chinese version, instead of two dimensions (physical and emotional), as were found in the original version.
Results
Clinical and Demographic Characteristics of the Sample
As presented in Table 1, there were 40 participants in the experimental group and 42 in the control group; in both groups, men comprised the majority. The mean age of participants in the experimental group was 61.6 years (standard deviation [SD]=12.24) and 68.5 (SD=3.02) in the control group. The majority of patients were unemployed, specifically 62.5% of patients in the experimental group and 64.3% in the control group. There was no significant difference in the mean of ejection fraction between the two groups, with 35.7 (SD=16.20) for the experimental group and 35.14 (SD=14.39) in the control group.
| Variable | Experimental (n=40) | Control (n=42) | χ2/t | P Value |
|---|---|---|---|---|
| Sex, No. (%) | 1.29 | .256 | ||
| Male | 32 (80) | 29 (69) | ||
| Female | 8 (20) | 13 (31) | ||
| Age, No. (%) | 2.522 | .014 | ||
| Mean (SD) | 61.5 (12.24) | 68.55 (13.02) | ||
| <54 y | 10 (25) | 4 (9.5) | ||
| 55–64 y | 14 (35) | 13 (31.5) | ||
| 65–74 y | 12 (30) | 8 (19) | ||
| >75 y | 4 (10) | 17 (39.5) | ||
| Education, No. (%) | 8.499 | .131 | ||
| Illiterate | 2 (5.0) | 7 (16.7) | ||
| Elementary | 24 (60) | 19 (45.3) | ||
| Junior/high | 12 (30) | 11 (26.2) | ||
| Associate | 2 (5.0) | 5 (11.9) | ||
| Marital status, No. (%) | 2.788 | .594 | ||
| Married | 33 (82.5) | 30 (71.4) | ||
| Single/other | 7 (17.5) | 12 (28.6) | ||
| Economic, No. (%) | 7.324 | .120 | ||
| Self-support | 25 (62.5) | 17 (40.5) | ||
| Retired fund | 4 (10) | 14 (41.4) | ||
| Children support | 11 (27.5) | 11 (26.2) | ||
| Religion, No. (%) | 7.632 | .106 | ||
| Yes | 24 (60) | 32 (76.2) | ||
| No | 16 (40) | 10 (23.8) | ||
| Employ status, No. (%) | 7.723 | .052 | ||
| Yes | 15 (37.5) | 15 (35.7) | ||
| No | 25 (62.5) | 27 (64.3) | ||
| Primary care, No. (%) | 15.251 | <.001 | ||
| Self-care | 37 (92.5) | 31 (73.8) | ||
| Family | 2 (5) | 11 (26.2) | ||
| Diet preparation, No. (%) | .513 | .474 | ||
| Self | 33 (82.5) | 37 (88.1) | ||
| Eat out | 7 (17.5) | 5 (11.9) | ||
| BMI, No. (%) | 5.662 | .059 | ||
| ≦23.9 Kg㎏/m2 | 22 (55) | 19 (45.2) | ||
| 24–26.9 Kg㎏/m2 | 13 (32.5) | 8 (19) | ||
| ≧27 Kg㎏/m2 | 5 (12.5) | 14 (33.3) | ||
| Years diagnosis with HF | 6.88 (±7.05) | 8.47 (±8.61) | –.902t | .370 |
| NYHA, No. (%) | 4.006 | .135 | ||
| Class I | 4 (9.5) | |||
| Class II | 23 (57.5) | 22 (52.4) | ||
| Class III | 17 (42.5) | 16 (38.1) | ||
| LVEF, % | 35.7 (±16.20) | 35.14 (±14.39) | –.152t | .879 |
| Causes of HF, No. (%) | 1.359 | .057 | ||
| Ischemic | 12 (30) | 15 (35.7) | ||
| Nonischemic | 28 (70) | 27 (64.3) | ||
| Comorbidities, No. (%) | .968 | .328 | ||
| <2 | 30 (75) | 30 (71) | ||
| >3 | 10 (25) | 12 ( 29) | ||
- Abbreviations: BMI, body mass index; HF, heart failure; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; SD, standard deviation. t:t test
In regard to the causes of HF, the majority of the participants were nonschemic in both groups (28 [70%] in the experimental group and 27 [64.3%] in the control group). There were no significant differences in demographics except for age and primary care between the experimental and control groups. The descriptive data for participants' self-care and QOL for both groups at different points of time are presented in Table 2. Scores on the self-management and self-confidence subscales remained below 70 in week 8, which indicates inadequate self-management and self-confidence. The lowest score for self-management was in regards to an extra diuretic pill taken for swelling or dyspnea. The lowest score for self-confidence was in regards to the evaluation of the importance of symptoms.
| Time | Experimental | Control | P Value | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| Self-management | ||||
| Self-maintenance | n=40 | n=42 | ||
| Baseline | 66.24 (14.58) | 56.66 (20.29) | .009 | |
| Week 4 | 69.16 (12.96) | 54.99 (20.73) | <.001 | |
| Week 8 | 70.66 (12.18) | 57.06 (21.30) | .001 | |
| Self-management | n=16 | n=12 | ||
| Baseline | 65.94 (9.87) | 47.50 (20.94) | .033 | |
| Week 4 | 67.19 (9.48) | 52.50 (20.62) | .066 | |
| Week 8 | 67.50 (9.49) | 54.17 (22.75) | .28 | |
| Self-confidence | n=40 | n=42 | ||
| Baseline | 37.53 (10.13) | 41.70 (25.65) | .276 | |
| Week 4 | 45.59 (12.08) | 37.60 (22.47) | .005 | |
| Week 8 | 46.70 (11.79) | 39.85 (19.26) | .058 | |
| Quality of life | n=40 | n=42 | ||
| Physical | Baseline | 16.38 (9.77) | 17.73 (9.82) | .578 |
| Week 4 | 13.0 (8.79) | 17.31 (10.36) | .058 | |
| Week 8 | 11.83 (8.39) | 17.0 (9.80) | .013 | |
| Baseline | 4.85 (4.79) | 8.37 (6.61) | .006 | |
| Emotion | Week 4 | 4.33 (4.47) | 7.12 (7.06) | .088 |
| Week 8 | 3.93 (4.04) | 6.98 (6.70) | .031 | |
| Baseline | 10.33 (5.18) | 18.17 (8.35) | <.001 | |
| Social | Week 4 | 8.20 (4.60) | 13.45 (7.44) | <.001 |
| Week 8 | 7.83 (4.72) | 13.26 (7.07) | <.001 | |
- Abbreviation: SD, standard deviation.
Effects of Self-Management Intervention
To determine the effects of the self-management intervention, self-care and QOL were examined as outcome measures by GEEs, with age, sex, primary care, and baseline QOL and self-care status as covariants.
As shown in Table 3, statistically significant changes occured between baseline and 2 months postintervention for self-maintenance and self-management among the experimental and control groups (P=.049 and P=.039, respectively). This indicates that the participants in the experimental group achieved better self-maintenance and self-management after the self-management intervention. There was no difference in the changes for self-confidence among these two groups.
| Variables | Self-Maintenance | Self-Management | Self-Confidence | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | P Value | B | SE | P Value | B | SE | P Value | |
| Intercept | 3.226 | 2.8938 | .265 | 17.268 | 4.5386 | <.001 | 55.897 | 14.0772 | <.001 |
| Group | |||||||||
| Experimental vs control | 4.027 | 1.1566 | .001 | –3.260 | 2.2320 | .144 | 2.518 | 3.8203 | .510 |
| Time | |||||||||
| Week 4 vs baseline | 0.569 | 1.1834 | .631 | 2.857 | 1.9793 | .149 | 1.831 | 1.8570 | .324 |
| Week 8 vs baseline | 2.357 | 1.1954 | .049 | 3.75 | 1.8145 | .039 | 3.526 | 2.0103 | .079 |
| Sex | |||||||||
| Female vs male | –1.078 | 1.5533 | .488 | 1.894 | 2.2300 | .396 | –5.441 | 4.3829 | .214 |
| Age | 0.047 | 0.0463 | .312 | –0.106 | 0.0657 | .107 | –0.202 | 0.1756 | .249 |
| Primary care | |||||||||
| Self-care vs family | 0.382 | 0.7521 | .612 | –2.860 | 1.2723 | .025 | 1.675 | 1.8936 | .376 |
| Baseline self-maintenance | 0.878 | 0.0341 | <.001 | ||||||
| Baseline self-management | 0.866 | 0.0553 | <.001 | ||||||
- Using generalized estimation equations for repeated measurements and the correlation structure exchangeable.
In Table 4, statistically significant changes are seen among baseline, 1 month, and 2 months postintervention in the physical, mental, and social aspects of QOL between the experimental and control groups (P<.001, P<.001, and P<.001, respectively). This indicates that the participants in the experimental group achieved better physical, mental, and social QOL after the self-management intervention.
| Variables | Physical | Emotion | Social | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | P Value | B | SE | P Value | B | SE | P Value | |
| Intercept | –7.810 | 4.9071 | .111 | –0.354 | 0.8921 | .692 | 0.875 | 1.4461 | .545 |
| Group | |||||||||
| Experimental vs control | –0.318 | 1.8446 | .863 | –0.022 | 0.3403 | .948 | –0.381 | 0.5243 | .467 |
| Time | |||||||||
| Week 4 vs baseline | –1.707 | 0.4988 | .001 | –0.840 | 0.3198 | .009 | –3.317 | 0.5615 | <.001 |
| Week 8 vs baseline | –2.439 | 0.5942 | <.001 | –1.111 | 0.3176 | <.001 | –3.598 | 0.5423 | <.001 |
| Sex | |||||||||
| Female vs male | 8.172 | 2.2844 | .001 | 1.127 | 0.4231 | .008 | 2.506 | 0.7197 | <.001 |
| Age | 0.184 | 0.0640 | .004 | –0.005 | 0.0118 | .678 | –0.001 | 0.0220 | .957 |
| Primary care | |||||||||
| Self-care vs family | 1.711 | 0.5719 | .003 | –0.047 | 0.1448 | .743 | –0.040 | 0.2097 | .850 |
| Baseline emotion | 0.900 | 0.0348 | <.001 | ||||||
| Baseline social | 0.740 | 0.0408 | <.001 | ||||||
Discussion
In this study, the percentage of male participants and the age distribution were similar to those of previous studies with similar inclusionary criteria.28, 30, 31 The majority of HF patients in Taiwan were unemployed, in contrast to a recent study conducted in the United States showing that fewer than half of HF patients are unemployed.32 This vast difference warrants further investigation to verify whether this is due to cultural differences or to other factors.
Self-care at baseline was less than 70, indicating that the participants' self-care was inadequate. This finding supports previous findings, which also revealed a low level of self-care in HF patients.12, 13 Notably, the mean score for self-confidence was 39.7, which is much lower than the score of 85.8 obtained by Tung and colleagues14 from another study in Taiwan. This might be due to participants being recruited from a rural area in Taiwan, while the previous study recruited participants from an urban area in Taipei, Taiwan.14 Participants in rural areas may not have the same opportunities for self-care as do those from an urban area. Therefore, the self-confidence level of those with HF living in rural areas in Taiwan needs further investigation.
The results demonstrate that patients with HF who received self-management intervention showed significantly better outcomes than those who did not. These findings are comparable with other studies8, 33, 34 indicating that patients in an intervention group feel more capable of dealing with disease-related symptoms and experience a better QOL than do those who did not participate in such program. The results of our study validate the contribution of a self-management intervention in obtaining better outcomes.
The most common nursing intervention for the care of both inpatients and outpatients with HF is education. Due to staffing shortages, primary care nurses usually provide limited patient education, generally using a standardized HF education sheet. Additionally, most educational programs for HF patients emphasize knowledge about the illness process and lack information on managing their symptoms or improving self-care.28, 34 The results of this study show that the use of an HF patient book, which includes individualized self-management intervention would enable a population to achieve optimal outcomes. Therefore, determining how to promote intervention as part of routine care is the next thing suggesting investigation.
Limitations and Recommendation
All participants were recruited from one hospital in the rural area of Taichung. Thus, the findings may not fully describe HF patients throughout Taiwan or worldwide. Due to limited resources, data were collected only at baseline, 1 month, and 2 months postintervention. Therefore, the long-term impact on self-care and QOL a year after the intervention has not been determined. Longitudinal research designed to determine the trajectories of self-care and QOL in this population over time is recommended.
A Cronbach's α of .696 for the self-care maintenance and .670 self-care management subscale is another limitation. Revised wording or current content of the Self-Care of HF Index by an expert panel and conduct pilot testing to enhance reliability are recommended. In addition, there was no ability to control for the effects of increased attention in the intervention group since the control group was historical.
Although there was significant improvement in self-care maintenance and self-care management after the intervention, the score for self-care management was still below 70, which is considered inadequate. Additionally, scores on the self-care confidence subscale were low and were not improved by the intervention. Therefore, any item for which the mean score was below 70 needs to be investigated and the cause of the low score needs to be determined. It also would be useful to interview patients in regard to their perspectives on barriers to desired outcomes.
In addition, patient education should be modified to include the presentation of case scenarios and the use of role playing regarding self-management skills. Experts must take these concerns into consideration when designing future self-management programs, which should be pilot-tested before their actual use. Additional administrative resources such as classroom availability and funding to support HF programs and to assess patient adherence to treatment are needed. Adding qualitative data to deepen our understanding of self-management and to be used to refine patient education programs, specifically concerning the identifying and addressing of certain symptoms, is recommended.
Conclusions
Results from this study revealed a low self-care score among HF patients and a positive correlation between self-care and QOL. Self-management interventions have been found to have the potential to improve self-care and to promote QOL. In this regard, future research on self-management interventions is needed to validate the findings of this research. Overall, regular care for HF patients after discharge including follow-up outpatient clinic appointments needs improvement in Taiwan. Because this study confirmed the effectiveness of a self-management intervention, a designated self-management patient book and individualized self-management education should be part of routine care for every patient with HF. Clinical providers must consider the importance of self-management skills and self-care, especially for chronic disease patients. In addition, hospital-based community services should provide education on self-management skills, thus, enabling patients to take an active role in managing their health conditions. In future research, double-blinded, random assignment to experimental and control groups should be applied to ensure valid measurement of the intervention effect.
Acknowledgments
We would like to express our deep appreciation for the patients in Tungs' Taichung Metro Harbor Hospital in Taichung Taiwan for their participation.




