Genetic counselors' preferences for coverage of preimplantation genetic diagnosis: A discrete choice experiment
Abstract
Preimplantation genetic diagnosis (PGD) allows couples to test for a genetically affected embryo prior to implantation. Patient access to this ethically complex and expensive technology differs markedly across jurisdictions, with differences in private/public insurance coverage and variations in patient inclusion and diagnostic criteria. The objective of the study was to identify trade-offs regarding PGD coverage decisions amongst genetic counselors. To quantify stated preferences for PGD coverage, we conducted a discrete choice experiment with Canadian genetic counselors (GC) considering attributes regarding the scope of testing (PGD indication, risk of the condition and number of cycles covered) and patient inclusion criteria (fertility status and family history). Multinomial logit regression was used to estimate trade-offs amongst attributes using part-worth utilities and importance scores. The completed response rate was 41% with 126 GC completing the survey. Risk of the genetic condition was the most important attribute. Overall, GC were more responsive to the scope of testing criteria including the condition's risk (importance score of 42%) and PGD indication (31%) rather than family history (11%) and fertility status (8%). Based on this study's attributes and levels, condition characteristics are prioritized even above patient characteristics for PGD coverage.
1 INTRODUCTION
Preimplantation genetic diagnosis (PGD) allows couples to avoid the birth of a child with a genetic condition by testing for genetically affected embryos during in-vitro fertilization (IVF) and implanting only unaffected embryos. While effective, PGD is expensive given the need for IVF, and ethically complex, resulting in variable and oftentimes limited access for patients. The majority of couples pay out-of-pocket for these services, as public/private IVF coverage with and without PGD is highly limited internationally.1-3
Access is complicated by issues of expense and variability in testing criteria.
The policy decisions made in Canada, where this study was conducted, and their impact on access, may be instructive for international jurisdictions grappling with PGD coverage.4 The province of Quebec publicly subsidized both PGD and IVF until 2015 when the program expenditures due to liberal criteria and high volumes,5 prompted a move to a tax credit and more defined criteria.6 The province of Ontario added IVF subsidization in 2015 but did not fund PGD.7 Other provinces have no public funding, resulting in costs being a barrier to access.8 In the United States, approximately 25% of health insurance plans cover IVF and 15 states have mandated private insurance plan legislation for infertility treatments.9
In addition to cost, differences in access within countries are complicated by two broad policy issues: ethical complexity regarding the scope of testing and the patient inclusion criteria for coverage.
No clear consensus exists regarding the scope of testing for the type or risk of a condition. For instance, Quebec used “severe” in reference to PGD coverage indications,10 the Netherlands used “high” disease risk with a working group looking at acceptability, capability and safety of the test,11 and the United Kingdom provides a list of PGD coverage indications.12 In general, the main policy question is whether less severe conditions such as adult-onset predispositions and other ethically contentious scenarios could be collectively subsidized.13 In addition, no consensus exists regarding the degree of genetic risk, as the United Kingdom specifies coverage only for risks greater than 10%,14 while Quebec had no risk restrictions.10
The policy debate extends to whether coverage should be restricted based on patient characteristics; for example, whether coverage should be extended to fertile couples7, 10 and those with unaffected children.15, 16 Relevant stakeholder preferences can be useful to inform policy development in contested areas of healthcare resource prioritization17, 18 and formulation of testing criteria.19 Severin et al reported that a condition's risk was highly valued by various stakeholders including 28 genetic counselors (GC) in a discrete choice experiment (DCE) assessing preferences for genetic test prioritization.18 In an Australian DCE of GC preferences for disclosure of incidental findings, age of onset (childhood vs adulthood) was second after availability of treatment for preferred characteristics.20 Both studies use DCE to inform types of genetic conditions preferred. However, neither DCE study examined patient characteristics as factors for consideration. As a DCE has been proven to be a robust method to ascertain stated preferences in the health care context,21-24 a DCE combining both condition and patient characteristics would inform this policy debate.
Stated preference studies on PGD coverage with relevant stakeholders could inform the above policy debates. Specific DCEs on PGD stated preferences are lacking. Instead, there are preference studies linking PGD use to family history. One patient-based study expressed the reason for preimplantation sex selection was either because the couple had no children or had children all of a certain sex.25 One study found that the majority of patients undergoing PGD had no children26 while another found that patients undergo PGD despite having unaffected children.27
There is a paucity of health care providers' preference studies for PGD. Available studies have focused on attitudes about which conditions to offer PGD and demonstrated that clinical practice varies based on the provider.28, 29 However, attitude data do not take into account trade-offs in characteristics like in a DCE. Furthermore, while there is support to use PGD for severe genetic conditions, attitudes amongst providers vary in the use of PGD for adult-onset disease.27 Clinical attitude differences create PGD access differences. In many countries, those who are referred for PGD are referred through the genetic clinics.29 As genetic counselors are clinical experts whose judgment informs practice, eliciting the preferences of GC for PGD coverage conditions using DCE would provide valuable insight. Therefore, given the complex issues in defining the scope of coverage and the potential for wide variation in preferences amongst GC, the objective of this DCE study was to identify trade-offs regarding attributes relevant to PGD coverage decisions amongst genetic counselors. Eliciting preferences of GC for PGD related to condition characteristics and patient inclusion criteria have relevance internationally, for any region developing PGD coverage policy where limited resources need to be accessed and allocated wisely.
2 MATERIALS AND METHODS
This study was approved by the Research Ethics Boards of the Hospital for Sick Children (number 1000032845) and University of Toronto. For the pilot and main studies, hardcopy and online surveys contained statements that consent was implied with survey completion.
2.1 Study design
The discrete choice method is based on random utility theory, which states that a good can be described in terms of its utility related to its known attributes as well as unobservable factors that can also alter its utility.30 By describing the utility of a good in this way, the various characteristics of the good can be quantified and ordered so that the strength of stated preferences can be estimated.
The methods for this study were based on the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) checklist for Good Research Practices for Conjoint Analysis.21
2.2 Recruitment
The inclusion criteria included all Canadian GC whether or not they were currently practicing, received training in genetic counseling, conducting research, and living or working in Canada to reflect a broad sample of the Canadian GC population. Members of the Canadian Association of Genetic Counselors (CAGC) were invited (n = 204) to participate. After three email blasts to the entire CAGC membership, recruitment was expanded to include snowball sampling of all GC in Canada regardless of their CAGC membership status. Emails were sent to GC or geneticist contacts at Canadian genetic centers to invite them to circulate the survey link to colleagues. Additional recruitment also took place at the 2014 CAGC Annual Education Meeting.
2.3 Survey design
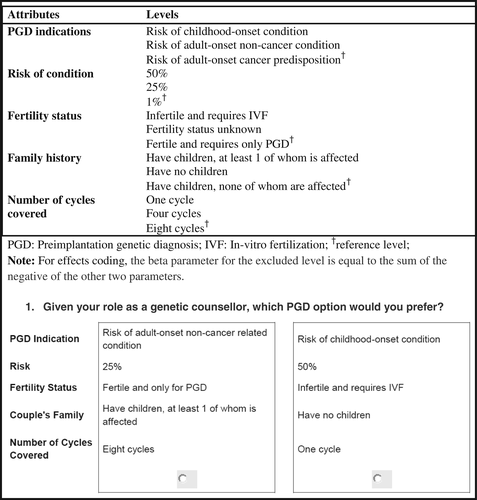
Identification of potential attributes and levels were generated through a literature review using published and gray literature. Relevant studies were identified in Embase, Medline, Google Scholar, public infertility/IVF sites and governmental sites with key terms “PGD,” “preferences,” “policy,” and “genetic counselors.” Five relevant studies were found25, 27, 28, 31, 32 from which potential attributes and levels were extracted for discussion in two focus groups held with Toronto-area GC. For the first focus group, PGD characteristics were discussed openly without prompting from the literature review to ensure that all important PGD characteristics were captured. Second focus group participants were presented with the generated attributes and levels identified from the literature and the first focus group to validate their appropriateness and to create a list of important PGD characteristics. The attributes suggested by each group were ranked and the average ranking was ordered from highest to lowest to compile a list of putative attributes (Supporting Information Appendix S1). An attribute describing a condition in terms of severity, whether it was life-limiting, and its treatability was not included based on variation in interpretation amongst focus group participants and to limit respondent burden. Although cost was identified as an important attribute by focus groups, GC do not allocate the budgets or consider opportunity costs in the health care system. Therefore, the cost attribute was not included in the study and number of cycles was chosen to represent coverage issues of greater relevance to GC. Based on focus group feedback, the maternal age was fixed at 30 years to avoid increased aneuploidy risk, and fertility decline with increased maternal age.33 Based on the focus group data, five possible attributes were selected for pretesting. The risk attribute levels were chosen to reflect autosomal dominant (50%), autosomal recessive (25%) and gonadal mosaicism (1%) risks, which are standard risks familiar to GC.
An experimental design was used that was level balanced and that optimized D-efficiency.23 Initially, an orthogonal design was proposed but could not be used as one of the potential levels of “HLA-matching” under PGD indications had to be restricted to a fixed recurrence risk of 25%. A main-effects attribute interaction between PGD indication and risk was considered but not included since inclusion of attribute interaction terms increased the standard error, decreased the D-efficiency and complicated the ability to comment on the part-worth utility of individual attributes. Furthermore, due to insufficient statistical power to draw conclusions about the influence of demographic variables on preference, interactions between attribute levels and demographic variables were not included. Pretesting was undertaken with seven GC to clarify wording and comprehension of the choice tasks that were constructed. The DCE questionnaire was constructed using Sawtooth software (Sequim, Washington) with two full profiles per choice task and 18 choice tasks. A pilot study was undertaken with 20 GC using online surveys and modifications were subsequently made to the survey instrument following a pilot data analysis. The fertility attribute was changed to include a third level “Fertility unknown” to allow for uniformity of three levels per attribute across the study thus improving level balance. The “unknown” fertility status was thought to be a reasonable category according to expert informants, given that if a couple were to try IVF for their first pregnancy, and then decided to have another child again through IVF; it would remain unknown whether they could have conceived naturally without IVF. Figure 1 shows the five attributes with three levels used in the study, and a sample choice set. By having all five attributes with three levels, the design was balanced in terms of level frequency. Therefore, there were 243 possible combinations of attribute alternatives (35) that could be arrayed in 122 pairs of options. The “complete enumeration” method through Sawtooth software's design option was used. This method takes a subset of the full-choice design and ensures minimal level overlap, balanced frequency of attribute levels, and maximizes orthogonality.23 Using four blocks of 18 choice tasks per block allowed for a small enough number of choice tasks to ensure survey completion of all blocks while increasing relative D-efficiency compared to three blocks. Respondents were randomly assigned one of the four questionnaire versions to complete online or on paper.
When the technology is one that users may decline, it is not unusual to include an “opt-out” option either as a third choice or as a two-stage DCE.21 In the present study, a two-stage approach was used in which respondents selected their preferred choice and then indicated whether they would opt-out or maintain the same choice. This provides an indication of how many respondents would have preferred neither option while allowing for part-worth estimation of all the data. One-way sensitivity analysis was performed with the opt-out compared to the forced-choice data.
2.4 Survey components
The complete survey package (Appendix S1) contained: (a) an explanatory document with the study background, a statement of implied consent by answering the survey, a preamble with definitions of the attributes and levels, and instructions on how to complete the survey; (b) the choice questionnaire; and (c) brief demographic and attitude questionnaires. The choice questionnaire was framed by asking genetic counselors to consider that they were on an advisory committee to decision makers in selecting which PGD option they would prefer between two profiles for each choice task. The attitude questionnaire included four true and false questions about the technique, process and ability of PGD to detect genetic conditions within an embryo in order to test respondent knowledge. In the pilot study, a fixed-choice task with a dominant option was embedded where all the most desirable attribute levels were presented. This rationality check was included to see whether respondents would always pick coverage for a high-risk childhood-onset condition in a childless, infertile couple as the dominant choice compared to a low risk adult-onset cancer predisposition in a fertile couple with no affected children. The rationality check was removed from the main study to reduce burden as all pilot study participants answered in the predicted way.
2.5 Data management
All data from electronic surveys were exported from Sawtooth Software into SAS (version 4.3; Cary, North Carolina). All hard copy responses collected at the CAGC Annual Education Meeting were entered into a data template created by Sawtooth Software with an assigned study number. The data were cross-checked at the time of transcription and a 10% random sample of hard copy responses were cross-checked by a second individual. No data required re-entry as a result of error. Data were managed and stored in a password protected computer. If a respondent started the main survey but then decided not to participate, the information collected prior to stopping was analyzed. The individual was counted as part of the response rate but was not counted in the completed survey response rate.
2.6 Statistical analysis
The software program SAS (version 4.3; Cary, North Carolina) was used for statistical analysis. Effects coding was used for all attributes, except for number of cycles, which was coded as a continuous variable. Descriptive statistics for the demographic questions were summarized using means and standard deviations (SD) for continuous variables and frequency distributions for categorical variables.
Multinomial logit regression (MNL) was used to analyze DCE data.34 MNL was chosen, as the focus of this study was to explore the explainable component of GC’ preferences and not to account for preference variation due to unexplained or random error. While the assumption of independence of irrelevant alternatives (IIA) property was not tested, Cheng and Long found that the tests were “unsatisfactory” and they recommended to ensure that the outcomes are distinct and can be weighed independently by the respondents.35 Pretesting was done to ensure that respondents found the choice sets to be reasonable and the covariance matrix data for individual attributes were examined with no correlations found amongst the attribute levels. Beta parameter estimates represent the mean part-worth utilities for each characteristic of PGD.
The attribute weighting was then calculated and used to generate importance scores for each attribute (Appendix S1). The attribute importance score was calculated based on the proportion an individual attribute contributes to the sum of ranges of part-worth utilities for all attributes (Appendix S1). Ninety-five percent confidence intervals (CI) for beta estimates were generated using bootstrapping by sampling from the original data 1000 times with replacement. The 1000 datasets were analyzed via regression analysis and the 25th and 975th ranked values for each beta estimate were used as the lower and upper confidence limits for each level.36
The opt-out effect was tested on the outcome variable using the PROC CATMOD command in SAS. When this was tested, the coefficient constant was extremely small and not statistically significant. Therefore, the analysis proceeded without focusing on the opt-out data.
3 RESULTS
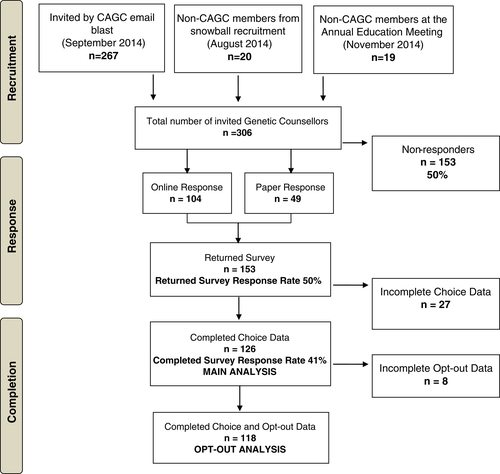
Figure 2 shows the recruitment process for the study and the resultant completed response rate of 41% (126/306). In order to ensure that respondents completed the survey only once, respondents were asked not to fill out the paper survey if already done online. The online response rate was 34% (104/306). Out of 146 paper surveys, 49 were returned for a response rate of 34% (49/146) (an underestimate since some respondents may have already filled out the survey online). The online survey completion rate was 79% (82/104) and 90% (44/49) for the paper survey. A token $5 gift card was offered for completing either version. Table 1 summarizes the characteristics of respondents (n = 126). The majority were female (98.4%), full-time genetic counselors (60.3%), practicing in Canada (81.0% of all respondents and 91.9% of those currently practicing) and practicing in academic centers only (54.8%). They were generally knowledgeable about PGD with 94.4% answering four true or false questions correctly regarding the technique, process and ability of PGD to detect genetic conditions within an embryo. When asked in the demographic questionnaire, the majority (82.5%) of genetic counselors believed that public coverage for both PGD and IVF should be provided by the government.
| Characteristics | Respondents (n = 126) | % / Mean (SD) |
|---|---|---|
| Age (years) | 33.7 (7.5) | |
| Female | 124 | 98.4 |
| Have no children | 69 | 54.8 |
| Full-time genetic counselor | 76 | 60.3 |
| >10 years of practice | 33 | 26.2 |
| Practices in an academic center only | 69 | 54.8 |
| Currently practicing in Canada | 102 | 81.0 |
| Practices in Quebec | 11 | 8.7 |
| Primary area of practice prenatal genetics | 54 | 42.9 |
| Have experience with at least one patient undergoing PGD | 54 | 42.9 |
| Preference for public coverage of PGD and IVF | 104 | 82.5 |
| Answered all four knowledge questions about PGD correctly | 119 | 94.4 |
- Abbreviation: PGD, preimplantation genetic diagnosis.
3.1 Stated preferences
The multinomial logit regression results are found in Table 2 and a graphical representation of the mean part-worth utilities categorized by attribute is presented in Figure 3. The interpretation is dependent on the attributes and levels selected for this study. Overall, all the part-worth utilities of levels for each attribute were statistically significant except for the No children level for Family history. The part-worth utility for Unknown Fertility Status (−0.173) was not significantly different from Fertile (−0.195) within the Fertility Status attribute. Respondents expressed the largest negative preference for PGD testing (−1.725; P value < 0.001) for a 1% risk of condition and the largest positive preference for a Childhood-onset condition (1.122; P value <0.001). Within Family history, a positive preference was observed for the affected children (0.396; P value < 0.001). In regards to Fertility status, a positive preference for PGD was observed for the Infertile couple (0.369; P value <0.001). Number of cycles was found to have a negative part-worth utility, with the magnitude of the negative preference increasing with the number of cycles.
| Attribute | Levels | Beta | 95% CI | SE | T-ratio | P value | Pr > χ2 | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Risk of condition | 50% | 1.057 | 1.002 | 1.115 | 0.059 | 17.915 | <0.001 | <0.0001 |
| 25% | 0.669 | 0.621 | 0.724 | 0.056 | 11.946 | <0.001 | <0.0001 | |
| 1%a | −1.725 | −1.839 | −1.622 | 0.079 | −21.835 | <0.001 | — | |
| PGD indication | Childhood-onset | 1.122 | 1.060 | 1.191 | 0.070 | 16.029 | <0.001 | <0.0001 |
| Adult-onset non-cancer | −0.179 | −0.219 | −0.140 | 0.055 | −3.255 | 0.010 | 0.001 | |
| Adult-onset cancer predispositiona | −0.944 | −1.051 | −0.841 | 0.058 | −16.276 | <0.001 | — | |
| Family history | Affected children | 0.396 | 0.352 | 0.444 | 0.057 | 6.947 | <0.001 | <0.0001 |
| No children | −0.033 | −0.071 | 0.002 | 0.050 | −0.660 | 0.526 | 0.515 | |
| Unaffected childrena | −0.363 | −0.446 | −0.280 | 0.052 | −6.981 | <0.001 | — | |
| Fertility status | Infertile | 0.369 | 0.329 | 0.409 | 0.054 | 6.833 | <0.001 | <0.0001 |
| Unknown | −0.173 | −0.206 | −0.143 | 0.052 | −3.327 | 0.009 | 0.0008 | |
| Fertilea | −0.195 | −0.266 | −0.123 | 0.051 | −3.824 | 0.004 | - | |
| Number of cyclesb | 1 | −0.079 | −0.088 | −0.069 | 0.013 | 17.915 | <0.001 | <0.0001 |
| 4 | −0.314 | −0.353 | −0.278 | |||||
| 8 | −0.629 | −0.706 | −0.556 | |||||
| -2Log likelihood of model without predictors (null) | 3144 | |||||||
| -2Log likelihood (predictor) | 1672 | |||||||
| Pseudo R2 | 0.468 | |||||||
| Adjusted pseudo R2 | 0.474 | |||||||
| Akaike information criterion | 1690 | |||||||
| Degrees of freedom | 9 | |||||||
- Abbreviation: α = 0.05; CI, confidence interval; Pr, probability.
- a Reference level.
- b Continuous coding.
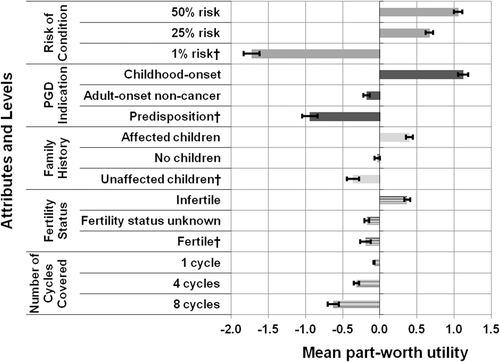
In general, attributes related to the risk of the condition and the PGD indication showed a larger strength of preference compared to the attributes related to inclusion criteria for PGD. The importance score calculation (Appendix S1) found that Risk of condition (42%), followed by PGD indication (31%), and Family history (11%) had greater weight of preference compared to Fertility status (8%) and Number of cycles (8%), which were found to be less important attributes related to preference for coverage. These importance scores are relative to the attributes and levels included in the study.
The opt-out option sensitivity analysis was based on fewer respondents (n = 118 compared to n = 126) since eight respondents did not complete the second question for all choice tasks. The forced-choice MNL analysis for n = 118 is shown in the supplemental material. The constant term using opt-out as a variable was not found to be statistically significant. The directionality and significance of the parameter estimates for all levels from the opt-out regression were similar to the n = 118 forced-choice analysis (Appendix S1). The exception was the parameter estimate for having No children which changed from −0.022 analyzed as a forced-choice to 0.047 analyzed with the opt-out (Appendix S1). However, this term was not significant. There were no differences in the levels that were statistically significant (P ≤ 0.05) when analyzed with the opt-out.
In the opt-out regression, there was a greater spread between the parameter estimates for the Risk of condition and PGD indication attributes, while the spread between the Number of cycles parameters decreased. The spread between the parameter estimates for Family history and Fertility status were similar between the two analyses.
4 DISCUSSION
In this discrete choice experiment of genetic counselors' preferences for PGD, choice tasks were presented regarding scope of testing based on a condition's age of onset, its risk and the amount of coverage, and the patient characteristics of family history and fertility status. The first key finding was that genetic counselors prioritize condition characteristics above patient inclusion factors, relative to the attributes and levels included in this study. In the literature, the condition's risk was highly valued in priority setting for genetic testing18 and the age of onset was a preferred criterion in determining management.20 However, the present Canadian study included patient inclusion attributes, which were not directly examined in the previous studies. Therefore, relative to the attributes and levels in this study, genetic counselors preferred condition characteristics over patient characteristics for coverage.
A possible explanation as to why genetic counselors in this study prioritized condition characteristics over other criteria relates to their role as health care professionals. Assessment and understanding of risk is an important part of the role of a genetic counselor.37 Genetic counselors may prefer to base decisions on clinical knowledge of risk and types of conditions rather than on patient characteristics for eligibility, which may depend on social and ethical considerations. It is also possible that by removing direct interaction with patients, a DCE may underestimate the importance patient characteristics may have on real-life choices.
The second key finding is that there is still some valuation of patient's characteristics for PGD coverage. Genetic counselors preferred PGD coverage for infertile couples. Since IVF is the treatment for infertility, infertile couples have already accepted the maternal IVF health risks. Based on De Wert's proportionality principle, infertile couples could therefore be more accepting of maternal risks for a broader range of PGD criteria compared to fertile couples.38
Family history valuation by GC was somewhat discordant with the literature. It was surprising that in this study, couples having no children did not seem to affect preference for PGD coverage, despite the fact that according to the literature, the majority of patients seeking PGD have no children.26 A possible explanation for the finding is that genetic counselors value the family history differently than patients. In Canada where this study was situated, it is interesting that policy makers in Quebec have also shown discordance, where previous to 2015, Quebec covered PGD regardless of family history, and then in evaluating the program in 2014, the province's Health and Welfare commissioner recommended that the assisted reproduction program should be amended to include limitations based on the number of existing children.5 Thus, there is value in considering patient characteristics in policy discussion.
The findings of the present study may have implications for public/private insurance PGD coverage. Clear guidelines about condition characteristics could affect the volume of patients eligible for coverage. If coverage was based on the proportionality principle whereby coverage for infertile couples with a risk for a genetic condition includes lower risk and adult-onset conditions,38 the scope of testing and the volume of patients eligible for PGD would increase. Increased eligibility would potentially increase demand and the total costs of a funded program. This occurred in Quebec which went over-budget without developing specific criteria for coverage.5 However, if coverage was based on a first-come first-served basis by placing an upper limit on the budget of the program similar to in Ontario as a cost-containment measure,16 milder indications for testing could be covered and as a result, consume resources which might have otherwise been spent on couples using PGD to detect earlier onset or higher risk conditions. Stakeholder preference studies such as the current study with genetic counselors could provide insight into how to consider and balance condition and patient characteristics to determine what PGD scenarios could be covered.
The study had several limitations. First, the hypothetical nature of the scenarios and the instrument design restricting choice tasks to defined attributes have been described in the literature as limitations in DCE studies.19, 39 By limiting the study to five important PGD attributes, other unobserved factors that may have influenced preference were not studied. We attempted to control for these factors by asking respondents to mentally hold all other characteristics equal to enhance internal validity. Focus groups were held to verify the factors suggested by the literature. The findings presented about PGD characteristics can be used as information rather than a prescribed set of restrictions based on genetic conditions or types of patients and should be interpreted relative to the attributes and levels that were included in this study. Second, the study restricted preference elicitation based on the onset of the condition and whether the condition was a predisposition or not. Therefore the generalizability of preferences for types of conditions to cover is restricted. However, GC were asked in the pilot study about the conditions they had thought about for each criterion. Since the answers from the pilot study were consistent, the preamble content for the main study was altered to include a few examples of conditions to ensure that respondents were considering similar clinically relevant conditions in their decision-making process. Third, two typos were in the study guide, one stating two levels for Fertility status and the other stating four levels for Amount of Public Funding. However, preamble descriptive bullets reflected the accurate number of levels. These errors were not expected to impact the study since respondents were presented with the right option number for each choice task. Fourth, there may have been survey sampling bias since participants were not randomly selected to participate but rather invited from organization membership via email and through an educational meeting. Attempts were made to avoid duplication given the recruitment strategies with online and paper surveys. Respondents may have participated because of their experience in the field or interest in the study topic resulting in volunteer bias. Yet, the demographic and practice characteristics of the study sample were comparable to the 2011 Professional Status Survey by the CAGC, providing reassurance that volunteer bias was not present.40 Since less than half of the GC were practicing primarily in Prenatal Genetics, it can be argued that a majority of the respondents may be clinical experts within the field. Furthermore, since 94.4% of genetic counselors answered all knowledge questions correctly, most respondents demonstrated adequate knowledge about PGD. Fifth, the response rate for this study was on the low end of the 18 to 88% range observed for choice-based conjoint analysis studies in health care.41 This study nevertheless represents the largest study of Canadian GC's preferences for PGD coverage. As the targeted respondents were genetic counselors, the study did not take into account the preferences of other relevant stakeholders such as couples. Finally, the cost of PGD was not included as an attribute which precluded calculation of willingness to pay, a measure that can help decision makers consider the perceived value of an emerging technology. Cost was excluded since GC are not the payers and would not be expected to consider affordability, budget allocation, or opportunity costs. GC were not explicitly asked to exclude considerations of cost from their choices as this aspect may influence their stated preferences with regard to number of cycles covered. A cost attribute would be informative in future research to assess payer's willingness-to-pay.
5 CONCLUSION
Genetic counselors prioritized condition characteristics above patient characteristics of family history and fertility status for PGD coverage relative to the attributes and levels in the current study. Clinical indications based on the risk and onset of the condition, are criteria that utilize genetic counselors' clinical expertise while use of patient characteristics may depend on social and ethical considerations. Further research in obtaining PGD coverage preferences from stakeholders such as patients and policy makers, as well as research into the ethical and social issues of restrictive vs permissive criteria for public coverage could be beneficial.
The findings from this study add a novel perspective from genetic counselors through preference elicitation regarding PGD coverage, which could be applicable to public/private insurance coverage in various jurisdictions. While the study was limited to genetic counselors, the results increase the knowledge around provider preferences and can help inform discussion about relevant policy issues. Discussion of these issues is timely, especially in the midst of ethical complexity surrounding the scope of PGD testing and patient inclusion criteria, as well as the rapid evolution of genetic testing and sequencing technology. Combined with further research, there is hope of defining appropriate access for PGD patients and decreasing the complexity surrounding PGD policy issues.
ACKNOWLEDGEMENTS
E.G. was supported by a Canadian Institutes of Health Research Fellowship (#493101) and a Restracomp Award 2011-2013 supported, fully or in part by the Ontario Student Opportunity Trust Fund, Hospital for Sick Children Foundation Student Scholarship Program. D.M. is supported by a Canada Research Chair in Health Systems and Services Research and the Arthur J.E. Child Chair in Rheumatology.
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
CONFLICT OF INTEREST
Nothing to declare.