Endophthalmitis following intravitreal injections administered by junior medical officers in rural Western Australia
Abstract
Background
Patients in rural Australia have limited access to intravitreal treatments due to a maldistribution of the ophthalmology workforce. To improve access, a novel outreach service model was implemented whereby junior medical staff administered intravitreal injections under a supervising ophthalmology consultant. This model involves outreach visits in hospitals, mobile clinics and a remote hub with intravitreal injections administered by junior doctors overseen by an ophthalmologist. The article explores the safety of this approach with respect to the rate of post-injection endophthalmitis.
Methods
A retrospective audit was conducted by the Lions Outback Vision outreach ophthalmology service from 2017 to mid-2023. The number of injections, locations, diagnoses, intravitreal agents used, designation of administering doctor and cases of endophthalmitis were reviewed.
Results
A 12 632 intravitreal injections were administered across 32 locations throughout rural Western Australia in the 6.5-year period. Three cases of endophthalmitis occurred representing a rate of 0.0237%.
Conclusion
The rate of endophthalmitis in the outreach service is comparable to other centres. The outreach model with supervising ophthalmology consultant support in person or via telehealth and administration of injections by junior medical staff has improved access for underserved or marginalised populations.
1 INTRODUCTION
The advent of intravitreal injections has brought about a paradigm shift in the treatment of various ophthalmic conditions. Previously, limited therapeutic options existed for sight-threatening diseases, such as age-related macular degeneration (ARMD), diabetic macular oedema (DMO) and retinal vein occlusions (RVO) with macular oedema. However, the utilisation of intravitreal injections, particularly with anti-vascular endothelial growth factors (anti-VEGF) medications, has revolutionised the management of these conditions.1-5 These injections are highly effective in stabilising or even improving visual acuity, altering the course and progression of these diseases. However, treatment for neovascular ARMD may be required on a recurrent basis on a 4–16-week interval.6 Thus, it is vital that these treatments are readily accessible to those in need.
Unfortunately, patients in rural areas face obstacles when accessing intravitreal injections due to the limited availability of ophthalmologists in these regions.7 Travel to urban centres where ophthalmologists are based is a physical and financial burden. Telehealth services are able to overcome most of these obstacles, however, most ophthalmic procedures do require in person attendance.8 The Royal Australian and New Zealand College of Ophthalmologists (RANZCO) acknowledges the unequal distribution of ophthalmic care and actively advocates for novel strategies to improve the accessibility of eye care services for individuals residing in underserved regions.9-12 A recent report from the Macular Disease Foundation Australia (MDFA) described access to intravitreal injection as ‘postcode lottery’ and highlighted the inequity in access to intravitreal injection based on location.13
Recognising this service delivery needed, Lions Outback Vision, part of the Lions Eye Institute, had successfully implemented an innovative public model of care to tackle these challenges and improve access to intravitreal injections in rural areas of Western Australia. The population served by Lions Outback Vision is approximately 300 000 people dispersed in towns of 500–35 000 people in a state of 2.5 million square kilometres.14-19 This article aims to describe this model and explore its safety through an evaluation of the rate of post-injection endophthalmitis.
2 METHODS
This study was approved by the University of Western Australia Human Research Ethics Committee (2023/ET001043) in accordance with the requirement of the National Statement on Ethical Conduct in Human Research.
2.1 Service model
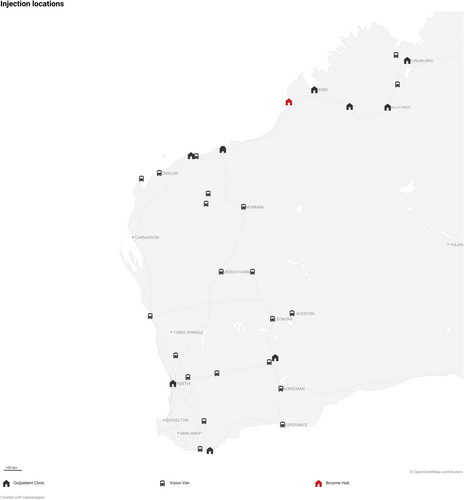
- Lions Outback Vision has a permanent ophthalmology service in Broome, where the injections were administered in an outpatient clinic.
- Nine locations are served via regular monthly outreach trips, and the injections were administered in outpatient clinics located in regional hospitals. These clinics are also utilised by other specialties at different times.
- Twenty-two locations are served through the Vision Van, which is a mobile clinic travelling across parts of Western Australia, as described previously.20 Intravitreal injections were performed in the mobile clinic.
2.2 Study design
A retrospective audit of this service was performed between 1st January 2017 and 30th June 2023. Post-treatment outcomes were recorded until 31st July 2023. The number of intravitreal injections administered, agents used, indication, designation of administering doctor, locations, and cases of endophthalmitis were recorded into a pre-designed data collection sheet. When endophthalmitis was suspected, patients had a consultation with either an ophthalmologist from Lions Outback Vision or with the on-call ophthalmology service of tertiary hospitals in Perth. As endophthalmitis is a rare but significant complication, Lions Outback Vision were notified of diagnoses made at these hospitals. Furthermore, as the primary eyecare team, Lions Outback Vision continued ongoing follow-up for cases initially managed in hospital. Any endophthalmitis that was diagnosed clinically by any ophthalmologist within 1 month after the intravitreal injection was included, regardless of microscopy or culture outcomes.
2.3 Training
Most injections were performed by junior medical staff, who work under the supervision of ophthalmology fellows or consultants. During this audit, there were 14 fellows, including five international medical graduates. Junior medical staff refers to any doctor who would be at least in their second post-graduate year (PGY) or beyond, but not yet entered a specialist training program. They hold ‘General Registration’ with the Medical Board of Australia.21 Specific to this audit, the junior medical staff range from PGY two to PGY six, and they have varying levels of ophthalmic experience.
All junior medical staff were trained upon joining Lions Outback Vision in the techniques of intravitreal injections, under the guidance and instruction of their supervisors according to well described practice.22 Once they were deemed competent by their supervisor and have been directly observed for 20 cases, they may perform the injections without direct supervision.
The decision for treatment is overseen by an ophthalmology fellow or consultant, either in person or via telehealth. In cases where there were limited staff members available, a minority of the injections were performed by the ophthalmology fellows or consultants themselves.
2.4 Technique used
A sterile technique was employed during intravitreal injections without the use of a speculum, calliper, or antibiotic drops. Hand sterilisation was performed with either alcohol-based hand rubs or hand scrub with soap. The treating doctor wears a mask and sterile gloves throughout the procedure. All patients receive at least 2 drops of topical oxybuprocaine 0.4% followed by subconjunctival anaesthesia using up to 0.1 mL of 2% lidocaine. The eye is cleaned and disinfected using either chlorhexidine 0.1% or half-strength Povidone-iodine solution 5%.23, 24 The solution is used around the eye, although ensuring that it reaches the conjunctival fornices. The tip of a 1 mL luer slip tip syringe (baremedical®, TERUMO™) is used to impress a ring on the conjunctiva as a guide to injection site (Figure 1). Any male luer slip tips compliant with ISO 80369-7:2016-2021 standards should have an external lumen diameter between 3.970 and 4.072 mm.25 After the procedure, the eyes were rinsed with sterile normal saline. The patient's vision is checked to ensure they can at least count fingers post-procedure. In instances where patient is unable to count fingers post-injection, the junior medical staff wait for 5 min to recheck vision and intraocular pressure. If the patient remains unable to count fingers and exhibits elevated intraocular pressure, the supervising consultant will be contacted without delay to guide further assessment and management.
2.5 Treatment regimens
Treatment regime is targeted at optimising visual outcome and balancing the burden to patients and carer. The service adopts a treat and extend protocol for patients with neovascular ARMD. Patients with DMO and RVO were initiated on a treat and extend protocol and, if stable without treatment for more than 3 months, they were converted to pro re nata (PRN) protocol with monitoring by local optometrist.
3 RESULTS
3.1 Total number of injections and rate of endophthalmitis
A 12 632 intravitreal injections were performed by Lions Outback Vision from January 1st, 2017 to June 30th, 2023. These injections were administered across 32 locations (Figure 2), with 22 of them being performed on the Vision Van and the remaining 10 in outpatient clinical settings in regional hospitals. Among these injections, there were three reported cases of endophthalmitis, resulting in an endophthalmitis rate of 0.0237%.
3.2 Indications
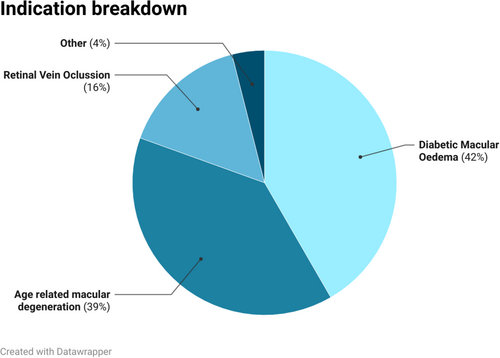
Of the 12 632 injections, 37% were provided for ARMD, 46% were provided for DMO, 13% were provided for RVO with macular oedema, and 4% were provided for other indications (Figure 3).
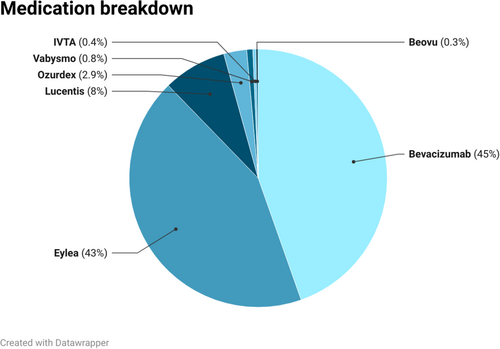
3.3 Medication used
The medication breakdown is as follows: bevacizumab accounted for 44.89%, aflibercept for 43.71%, ranibizumab for 7.18%, dexamethasone intravitreal implant (Ozurdex) for 2.85%, faricimab for 0.82%, triamcinolone for 0.31%, and brolucizumab for 0.24% (Figure 4). Out of bevacizumab, 5301 units were Avastin, and 369 units MVASI. Both bevacizumab preparations were prefilled compounded injections.
3.4 Case summary
All three patients were transferred to tertiary hospital for treatment of endophthalmitis.
3.4.1 Patient 1
The patient developed a painful red eye with decreased vision 2 days after receiving intravitreal bevacizumab (Avastin) for DMO. The patient was promptly transferred to a tertiary hospital where it was noted that they had a visual acuity of hand movement only in the affected eye. The patient received intravitreal antibiotics and a subsequent vitrectomy. Staphylococcus epidermidis was isolated. On the most recent visit, the patient's visual acuity improved to 6/7.5.
3.4.2 Patient 2
Four days following the administration of intravitreal bevacizumab (Avastin) for DMO, the patient experienced a painful red eye with decreased vision. The visual acuity in the affected eye was reduced to hand movement only. On the day of diagnosis, the patient underwent vitrectomy and received intravitreal antibiotics. S. epidermidis was isolated from the vitreous sample. Unfortunately, the patient did not attend multiple follow-up appointments and consequently developed chronic retinal detachment in the affected eye, resulting in a final visual acuity of perception of light only.
3.4.3 Patient 3
This patient presented with a painful red eye with decreased vision 4 weeks after receiving intravitreal bevacizumab (Avastin) for DMO. The visual acuity in the affected eye was hand movement only upon presentation. During the same visit, the patient received intravitreal antibiotics and was later transferred to a tertiary centre where a vitrectomy was performed. The vitreous culture was negative, and no pathogen was isolated. The most recent visual acuity assessment showed an improvement to 6/9.
4 DISCUSSION
This novel ophthalmic outreach service model, whereby junior medical staff administer the intravitreal injections, had a favourable safety profile with only three cases of endophthalmitis (0.024%) after administering 12 632 injections over 6.5 years across 32 locations in Western Australia. Intravitreal injections are a widely utilised treatment modality for various ophthalmic conditions across the globe. Although the specific model of care for administering intravitreal injections may differ among different healthcare systems and regions, the overarching goal remains consistent—to provide safe and effective treatment to patients in need.
The technique used for injection administration does not include topical antibiotics pre- or post-injection as there is limited evidence in reducing the rate of endophthalmitis.26-28 Additionally, prefilled compounded bevacizumab injections were used, as these are associated with lower rates of endophthalmitis compared with using multiple injections from a single vial.29
Bevacizumab remains a commonly used therapeutic agent (off label) to overcome access barriers. The pharmaceutical benefits scheme (PBS) is part of the Australian Medicines Policy, which lists the medications subsidised by the government. Even though most intravitreal injections (apart from bevacizumab) are subsidised, application for their use and delivery of the medication has to be planned days in advance. As the nature of our service is mobile and experiences unpredictable clinic attendance, access to PBS subsidised medication was challenging.30 Initially, our service heavily relied on bevacizumab, a lower cost option, due to these access limitations. Securing a supply of bevacizumab became problematic following the discontinuation of Avastin. During this period, with a maturing service and logistics, more patients have been able to access subsidised medications through the PBS. Injection in the rural areas is supplied by community pharmacies. They are discouraged to stock large quantities of injections due to the high upfront cost of medication in combination with the unpredictable attendance of patients. This continues to pose challenges in the supply logistics of subsidised medications and remain a potential barrier for our patient population.
In rural settings where access to ophthalmologists is limited, alternative models of care for intravitreal injections are relevant to provide timely access to care. Other models of care have been implemented, including hospital-based, clinic-based, or community-based approaches. Some regions have adopted different models of care to increase accessibility and efficiency. For example, a nurse-administered intravitreal injection service under ophthalmologist supervision described in the National Health Service in United Kingdom has shown favourable results.31 Nurse-administered intravitreal injections have also been trialled in Singapore.32
In the Lions Outback Vision model, junior medical staff are trained to perform intravitreal injections under supervision. Junior medical staff are well-equipped with essential workplace safety skills, including aseptic techniques, medication administration, safe handling of sharps, and managing bodily fluids. These comprehensive skills are transferrable when learning to perform intravitreal injections.
In this care model, an ophthalmologist assumes responsibility for patient care and decision-making, providing oversight whenever necessary. Supervision by ophthalmologists ensures that junior medical staff were appropriately trained, adhere to established protocols, and collaborate closely with the supervising professionals. Regular communication and structured supervisory sessions between junior medical staff and ophthalmologists are essential. This model enhances access to intravitreal injections in rural areas and promotes the professional growth of junior medical staff. By working closely with highly skilled professionals, junior medical staff can expand their knowledge, acquire new skills, and contribute effectively to patient care, thereby improving healthcare outcomes in underserved regions.
The reported rates of endophthalmitis performed by ophthalmologists after undergoing intravitreal injection vary significantly with studies reporting 0.021%–0.053%.28, 33-35 Our observed rate of 0.0237% lies within this range. A limitation of the study is that there was a lack of data on the rate of other complications associated with intravitreal injections, such as cataract formation, vitreous haemorrhage, rhegmatogenous retinal detachment, intraocular inflammation and sustained increase in intraocular pressure requiring anterior chamber paracentesis.36 Another limitation is the possibility of underreporting cases of endophthalmitis. The likelihood of underreporting cases of endophthalmitis is expected to be very low for several reasons. First, the severity and nature of the condition typically prompt patients to seek medical attention urgently. Seeking care locally usually involves visiting the Emergency Department, General Practitioner or optometrist, resulting in either direct contact with or referral to tertiary public hospitals. Lions Outback Vision medical staff are in regular communication relating to regional transfer of patients for hospital care and feedback is well established for shared care. Any potential endophthalmitis case would have coordinated regionally based follow-up for the patient post discharge. Additionally, Lions Outback Vision services are free of charge and closer to home which reduces the likelihood of patients travelling 500–3000 km to seek private urban care and bypass Lions Outback Vision regionally based services since government supported transport cost reimbursement is unavailable due to visiting or regional service availability via Lions Outback Vision.
The main strength of the study is that it spans 6.5 years of data from a real-world service involving multiple junior medical staff across 32 sites. This robust dataset improves the study's external validity and generalizability, making the findings more applicable to broader patient populations and healthcare settings. As the field of ophthalmology continues to evolve, it is crucial to strike a balance between providing accessible, patient-centred care and prioritising safety, efficiency and quality outcomes.
As global demand for intravitreal injection is forecasted to grow, it is important for health networks to collectively refine and optimise models of care for intravitreal injections to deliver the best possible care to patients in diverse healthcare settings.37 In our model of care, we have observed that junior medical staff were able to perform intravitreal injections in rural regions with a low rate of endophthalmitis.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
Research data are not shared.